Abstract
Purpose
Our aim was to review and update the existing evidence-based and consensus-based recommendations for the management of chest injuries in patients with multiple and/or severe injuries in the prehospital setting. This guideline topic is part of the 2022 update of the German Guideline on the Treatment of Patients with Multiple and/or Severe Injuries.
Methods
MEDLINE and Embase were systematically searched to May 2021. Further literature reports were obtained from clinical experts. Randomised controlled trials, prospective cohort studies, cross-sectional studies, and comparative registry studies were included if they compared interventions for the detection and management of chest injuries in severely injured patients in the prehospital setting. We considered patient-relevant clinical outcomes such as mortality and diagnostic test accuracy. Risk of bias was assessed using NICE 2012 checklists. The evidence was synthesised narratively, and expert consensus was used to develop recommendations and determine their strength.
Results
Two new studies were identified, both investigating the accuracy of in-flight ultrasound in the detection of pneumothorax. Two new recommendations were developed, one recommendation was modified. One of the two new recommendations and the modified recommendation address the use of ultrasound for detecting traumatic pneumothorax. One new good (clinical) practice point (GPP) recommends the use of an appropriate vented dressing in the management of open pneumothorax. Eleven recommendations were confirmed as unchanged because no new high-level evidence was found to support a change.
Conclusion
Some evidence suggests that ultrasound should be considered to identify pneumothorax in the prehospital setting. Otherwise, the recommendations from 2016 remained unchanged.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Germany, the chest is the body region that is most affected in polytrauma patients. A serious injury, i.e. an injury with an Abbreviated Injury Scale score of at least 3, is present in 46.1% of patients [1]. Several thoracic injuries can lead to acute life-threatening conditions that, based on the ABCDE priorities of trauma management, affect a patient’s breathing (B) or circulation (C). These conditions and their immediate consequences can develop dynamically and must therefore be expected to occur even in the prehospital setting. Since qualified emergency medical services (EMS) personnel usually arrive at the scene of an incident at an early stage, it is possible that life-threatening conditions and their causes can be detected, and appropriate life-saving interventions can be performed in this setting. The objective of this systematic review is to identify the current evidence on diagnostic and treatment approaches especially in the prehospital setting and to assess its usefulness as a basis for evidence-based clinical recommendations for emergency physicians and EMS personnel.
Methods
This guideline topic is part of the 2022 update of the German Guideline on the Treatment of Patients with Multiple and/or Severe Injuries [2]. The guideline update is reported according to the RIGHT tool [3], the systematic review part according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 reporting guideline [4]. The development and updating of recommendations followed the standard methodology set out in the guideline development handbook issued by the German Association of the Scientific Medical Societies (AWMF) [5]. All methods were defined a priori, following the methods report of the previous guideline version from July 2016 [6, 7] with minor modifications, as detailed below. The “Discussion” section of this publication is a direct translation of the original guideline text [2].
PICO questions and eligibility criteria
Population, intervention, comparison, and outcome (PICO) questions were retained from the previous guideline version. In addition, the participating professional societies involved in guideline development were asked to submit new PICO questions. The overarching PICO question for this topic area was:
In adult patients (≥14 years) with known or suspected polytrauma and/or severe injuries, does a specific prehospital approach to the management of chest injuries improve patient-relevant outcomes compared to any other intervention?
The full set of predefined PICO questions is listed in Table S1 (Online Resource). The study selection criteria in the PICO format are shown in Table 1.
Literature search
An information specialist systematically searched for literature in MEDLINE (Ovid) and Embase (Elsevier). The search strategy described in the 2011 Guideline was used with modifications. It contained index (MeSH/Emtree) and free-text terms for the population and intervention. The searches were completed on 19 May 2021. The start date for update searches was 1 June 2014. Table S2 (Online Resource) provides details for all searches. Searches were conducted for both prehospital and inhospital care. Clinical experts were asked to submit additional relevant references.
Study selection
Study selection was performed independently by two reviewers in a two-step process using the predefined eligibility criteria: (1) title/abstract screening of all references retrieved from database searches using Rayyan software [9] and (2) full-text screening of all articles deemed potentially relevant by at least one reviewer at the title/abstract level in Endnote (Endnote, Version: 20 [Software]. Clarivate, Boston, Massachusetts, USA; https://endnote.com/). Disagreements were resolved through consensus or by consulting a third reviewer. The reasons for full-text exclusion were recorded (Table S3, Online Resource).
Assessment of risk of bias and level of evidence
Two reviewers sequentially assessed the risk of bias of included studies at study level using the relevant checklists from the NICE guidelines manual 2012 [10] and assigned each study an initial level of evidence (LoE) using the Oxford Centre for Evidence-based Medicine Levels of Evidence (2009) [11]. Any disagreements were resolved through consensus or by consulting a third reviewer.
Data extraction and data items
Data were extracted into a standardised data table by one reviewer and checked by another. A predefined dataset was collected for each study, consisting of study characteristics (study type, aims, setting), patient selection criteria and baseline characteristics (age, gender, injury scores, other relevant variables), intervention and control group treatments (including important co-interventions, index and reference tests for diagnostic studies), patient flow (number of patients included and analysed), matching/adjusting variables, and data on outcomes for any time point reported.
Outcome measures
Outcomes were extracted as reported in the study publications. For prospective cohort studies and registry data, preference was given to data obtained after propensity-score matching or statistical adjustment for risk-modulating variables over unadjusted data.
Synthesis of studies
Studies were grouped by interventions. An interdisciplinary expert group used their clinical experience to synthesise studies narratively by balancing beneficial and adverse effects extracted from the available evidence. Priority was given to diagnostic test accuracy, reducing prehospital and inhospital mortality, immediate complications, and long-term adverse effects. Clinical heterogeneity was explored by comparing inclusion criteria and patient characteristics at baseline as well as clinical differences in the interventions and co-interventions.
Development and updating of recommendations
For each PICO question, the following updating options were available: (1) the recommendation of the preceding version remains valid and requires no changes (“confirmed”); (2) the recommendation requires modification (“modified”); (3) the recommendation is no longer valid or required and is deleted; (4) a new recommendation needs to be developed (“new”). An interdisciplinary expert group of clinicians with expertise in trauma and acute care (comprising prehospital emergency physicians, anaesthesiologists, trauma surgeons, thoracic surgeons) reviewed the body of evidence, drafted recommendations based on the homogeneity of clinical characteristics and outcomes, the balance between benefits and harms, as well as their clinical expertise, and proposed grades of recommendation (Table 2). In the absence of eligible evidence, recommendations were made based on clinical experience, data from studies with a lower level of evidence, and expert consensus in cases where the Guideline Group felt a statement was required due to the importance of the topic. These were not graded, and instead labelled as good (clinical) practice points (GPP). For GPPs, the strength of a recommendation is presented in the wording shown in Table 2.
Consensus process
The Guideline Group finalised the recommendations during web-based, structured consensus conferences on 13 September 2021 and 15 March 2022 via Zoom (Zoom, Version: 5.x [Software], Zoom Video Communications, Inc., San José, California, USA; https://zoom.us). A neutral moderator facilitated the consensus conference. Voting members of the Guideline Group were delegates of all participating professional organisations, including clinicians, emergency medical services personnel, and nurses, while guideline methodologists attended in a supporting role. Members with a moderate, thematically relevant conflict of interest abstained from voting on recommendations; members with a high, relevant conflict of interest were not permitted to vote or participate in the discussion. Attempts to recruit patient representatives were unsuccessful. A member of the expert group presented recommendations. Following discussion, the Guideline Group refined the wording of the recommendations and modified the grade of recommendation as needed. Agreement with both the wording and the grade of recommendation was assessed by anonymous online voting using the survey function of Zoom. Abstentions were subtracted from the denominator of the agreement rate. Consensus strength was classified as shown in Table 3.
Recommendations were accepted if they reached consensus or strong consensus. For consensus recommendations with ≤ 95% agreement, diverging views by members of the Guideline Group were detailed in the background texts. Recommendations with majority approval were returned to the expert group for revision and further discussion at a subsequent consensus conference. Recommendations without approval were considered rejected.
External review
During a 4-week consultation phase, the recommendations and background texts were submitted to all participating professional organisations for review. Comments were collected using a structured review form. The results were then assessed, discussed, and incorporated into the text by the guideline coordinator with the relevant author group.
The guideline was adopted by the executive board of the German Trauma Society on 17 January 2023.
Quality assurance
The guideline recommendations were reviewed for consistency between guideline topic areas by the steering group. Where necessary, changes were made in collaboration with the clinical leads for all topic areas concerned. The final guideline document was checked for errors by the guideline chair and methodologist.
Results
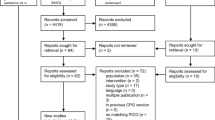
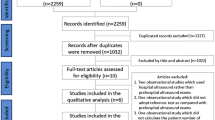
The database searches identified 4419 unique records (Fig. 1). Ten additional records were obtained from clinical experts. Two studies were eligible for this update [12, 13]. A total of 70 full-text articles were excluded (Table S3, Online Resource).
Characteristics of studies included in this update
Study characteristics, main outcomes, levels of evidence, and risk-of-bias assessments are presented in Table 4. Full details are provided in Table S4 (Online Resource). The evidence included two diagnostic accuracy studies. Both studies were performed in the USA. Eligible patient populations were adults with severe injuries and suspected injuries to the chest. The detection of pneumothorax using in-flight ultrasonography was studied in both publications.
Risk-of-bias assessment for included studies and levels of evidence
One study was judged to be of low risk of bias in all domains. The risk of bias regarding flow and timing was unclear in one study.
Recommendations
One recommendation was modified and one new recommendation as well as one new GPP were developed based on the updated evidence and expert consensus. Eleven recommendations were confirmed as unchanged because no new high-level evidence was found to support a change (Table 5). All achieved strong consensus. One recommendation from the 2016 Guideline was not retained in the 2022 update (Table S5, Online Resource).
Discussion and Rationale for Recommendations
Diagnosis
Physical examination supported using EMS technical equipment is essential for the formulation of a (working) diagnosis [7, 14,15,16]. Decisions about any necessary treatment cannot be made without a diagnosis. There is a lack of comprehensive evidence regarding the relative role of individual diagnostic measures. Nevertheless, chest auscultation, respiratory rate measurement, and the assessment of spontaneous pain and pain/tenderness on palpation have been shown to have sufficient diagnostic accuracy and to provide information that is relevant for treatment in the acute setting [7, 14, 17,18,19,20]. Other types of examination (palpation, percussion) can be used in individual cases, but their accuracy and relevance are not well studied [7]. Continuous monitoring using pulse oximetry and capnography (in ventilated patients) together with repeated physical examinations may help detect dynamic deterioration. Progression of pneumothorax (or another chest injury) should be considered a possible cause of deterioration.
Small mobile ultrasound devices have become increasingly available for use in the prehospital care setting (and their quality has progressively improved over the years). A Cochrane review has shown that the sensitivity of ultrasound in trauma patients (91%) was almost twice as high as that of standard chest X-ray (47%) in hospital emergency departments [21]. Compared with computed tomography, the sensitivity of ultrasound was still 81% [22]. The specificity of ultrasound was found to be 98–99%.
Different results regarding the use of ultrasonography in the prehospital setting were reported in two prospective observational studies. In the earlier study, which was published in 2014, ultrasonography for pneumothorax had a sensitivity of only 18.7% and a specificity of 99.5% [23]. In the study by Quick et al. [13], ultrasonography correctly identified 68% of pneumothoraces and had a specificity of 96%. Positive predictive values of 80% and 94.2% and negative predictive values of 92.7% and 97.7% were obtained. Diagnostic accuracy in the prehospital setting was thus slightly lower than that reported for the resuscitation room setting. It was, however, still higher than the diagnostic accuracy of a purely clinical examination. This applies to patients with decreased levels of consciousness. A possible explanation for this slightly poorer result may be that examinations in the prehospital setting take place in less favourable conditions (lighting, time pressure, weather, and other environmental conditions, etc.). Moreover, selection bias was present in both studies and different reference standards (chest computed tomography, standard chest X-ray, and clinical examination) were used. In both studies, ultrasound examinations were performed by EMS personnel (with special training in ultrasound but mostly without previous experience in ultrasound imaging). By contrast, ultrasound is predominantly used by emergency physicians in Germany. Whether emergency physicians have better ultrasound skills than EMS personnel is unknown. Although ultrasound devices have been available to air medical services for many years, there are no systematic reports or clinical studies with large sample sizes. Inhospital results cannot be simply transferred to the prehospital setting. In the inhospital setting, ultrasound examinations are often performed by radiologists. The expertise of emergency physicians and EMS personnel is unknown.
Likewise, it is completely unclear how often ultrasonographic evidence of the presence or absence of pneumothorax results in, or would result in, therapeutic consequences and better outcomes. A benefit-risk analysis cannot be carried out based on current knowledge.
As long as there are no data from Germany or similar emergency medical service systems which provide reliable evidence for a broad competence in prehospital ultrasound among emergency physicians and for therapeutic consequences of ultrasonographic findings that lead to a positive benefit-risk assessment, there is no basis for a higher grade of recommendation.
Diagnosis of pneumothorax
In patients with unilaterally decreased breath sounds in association with shortness of breath and/or chest pain, the probability of pneumothorax is 90–99% [14]. If none of these three signs and symptoms is present, the probability of pneumothorax is less than 1%. This also means that a major pneumothorax can be largely ruled out in the absence of these auscultation findings, especially in patients with normal breathing and no chest pain. In patients with detected pneumothorax but equal bilateral breath sounds, the mean volume of pneumothorax was reported to be 378 mL (maximum volume, 800 mL) [24]. When auscultation findings are interpreted, correct positioning of the endotracheal tube (if present) must be ensured as far as possible. The specificity and positive predictive value of soft tissue emphysema or flail chest are unknown [14]. The presence of bilateral pneumothorax must be considered in patients with severe bilateral chest trauma and may be associated with atypical examination results. Data that help differentiate between a pneumothorax and a haemothorax, or a combination of both, are not available. Percussion can be helpful but is of limited relevance in the prehospital setting since the differentiation between pneumothorax and haemothorax does not have a verifiable effect on treatment needs.
If left untreated, pneumothorax can progress to tension pneumothorax. Even occult pneumothoraces can progress to pneumothoraces that require chest tube drainage in 6–9.5% [25,26,27,28,29,30] and in as much as 14% of ventilated patients [29]. It can be assumed that the rate of progression is higher for large pneumothoraces, but this is not definitely known. The main risk is that an originally asymptomatic pneumothorax progresses to a tension pneumothorax.
Diagnosis of tension pneumothorax
The signs and symptoms and the order of occurrence of signs and symptoms differ between patients who are breathing unassisted and patients receiving assisted ventilation [31]. Respiratory distress and tachycardia are the usual predominant presenting features of tension pneumothorax in awake, spontaneously ventilating patients [15]. Chest pain, tachypnoea, and decreased breath sounds were reported to be present in more than 45% of spontaneously breathing patients. Dyspnoea/respiratory distress, hypoxia and requirement for supplemental oxygen, tachycardia, and percussion hyperresonance were noted in 30 to 45%. Contralateral tracheal deviation (15–30%) or hypotension (developing in a relatively delayed fashion), jugular venous distention, subcutaneous emphysema, and cardiac arrest (each in less than 15%) were less common [31]. Experimental studies have shown that respiratory distress and paralysis of the respiratory centre as a result of hypoxia precede cardiac arrest in awake patients and that hypotension progressing to cardiac arrest is a late sign of tension pneumothorax [32, 33].
By contrast, the haemodynamic consequences of tension pneumothorax (e.g. decrease in blood pressure, shock) were reported to occur much earlier in ventilated patients and usually at the same time as respiratory signs and symptoms [15, 31]. Decreased breath sounds, hypotension (often with sudden onset), and hypoxia were noted with equal frequency (> 45%). Tachycardia, subcutaneous emphysema, and cardiac arrest were common as well (30–45%) [31]. In ventilated patients, considerably elevated or increasing airway pressure is another symptom that is seen in about 20% of patients with haemothorax/pneumothorax [16, 17].
According to expert opinion, the presence of tension pneumothorax is highly probable in patients with a combination of (unilaterally) absent breath sounds (after confirmation of correct tube position) and life-threatening respiratory or cardiovascular dysfunction so that the diagnosis should be established based on these findings and the necessary therapeutic measures should be initiated. Further additional diagnostic procedures should not be undertaken since they would present an avoidable delay. The consequences of a false positive diagnosis of tension pneumothorax appear to be less severe than those of not performing any necessary decompression.
Treatment of pneumothorax and tension pneumothorax (indications for treatment)
Tension pneumothorax is an acute life-threatening condition and, if left untreated, usually leads to death. Death can occur within a few minutes of the onset of signs and symptoms of impaired pulmonary and cardiovascular function. There is no alternative to decompression. Expert opinion is that emergency decompression must be immediately performed especially in patients with haemodynamic or respiratory compromise and that patient transport, even to a nearby hospital, would cause an unacceptable delay. A study involving 3500 autopsy records identified 39 cases of tension pneumothorax (incidence, 1.1%), half of which had not been diagnosed while the patients were still alive. Among soldiers serving in the Vietnam War, tension pneumothorax was detected in 33% of patients with fatal chest injuries [34]. An analysis of 20 patients who had been identified as unexpected survivors based on the Trauma and Injury Severity Score (TRISS) showed that seven of these 20 patients had undergone prehospital decompression for tension pneumothorax [35]. Four of 18 trauma patients who had undergone resuscitation in the prehospital setting had a return of cardiac output following decompression [36]. An analysis of patients with traumatic cardiac arrest identified decompression of tension pneumothorax as the most important factor contributing to an improvement in prognosis [37]. In recent analyses, too, untreated tension pneumothorax has been identified as one of the most common causes of potentially preventable deaths [38].
A large pneumothorax, which must be assumed in the presence of typical auscultation findings, is an indication for pleural space evacuation. Whether this must be done in the prehospital or in the hospital setting is difficult to decide in individual cases since the risk of progression from simple pneumothorax to tension pneumothorax and the period over which progression can take place vary and are difficult to estimate. Ventilated patients have a considerably higher risk of pneumothorax progression [39]. According to expert opinion, it is therefore plausible that a pneumothorax detected by auscultation in ventilated patients is associated with a considerably elevated risk of developing into a tension pneumothorax and thus is an indication for prehospital decompression. Conversely, pneumothoraces develop into tension pneumothoraces in less than 10% of spontaneously breathing patients [39]. Based on a benefit-risk assessment, prehospital decompression therefore appears to be unnecessary in patients with no or mild signs and symptoms and no signs and symptoms of progression. These patients must be managed by observation, close monitoring, and clinical reevaluation. If patients cannot be easily monitored and clinically reviewed, for example during helicopter transport, there is a certain non-quantifiable risk that a tension pneumothorax develops and that this condition is not detected in time or that there is not enough space to provide appropriate treatment. In such situations, and depending on individual circumstances, decompression of pneumothorax may also be performed in non-intubated patients with relevant clinical signs and symptoms prior to transport.
If equal bilateral breath sounds are found, a clinically relevant pneumothorax will unlikely be present. This means there is no indication for prehospital decompression or pleural space evacuation even if other signs of chest trauma (but no specific signs of pneumothorax) are present. In a systematic review [14], the incidence of pneumothorax was reported to be relatively low despite the presence of chest trauma (10 to 50%). This means that if there is no clear evidence of pneumothorax and an intervention is performed based on a diagnosis of chest trauma alone, at least every second patient or even up to nine out of 10 patients will undergo an unnecessary invasive procedure. Since relevant studies also included occult pneumothoraces that were detected only via computed tomography, the percentage of cases requiring chest tube drainage may be even lower. Even when pneumothorax was suspected based on specific clinical signs, the rate of unnecessary needle decompressions and chest tube drainage ranged between 9 and 65% [17, 40, 41]. Under these conditions, there is no indication for decompression in non-ventilated patients.
In general, chest drainage for haemothorax is not indicated in the prehospital setting. Although a large haemothorax (approximately > 300 mL) is usually an indication for the drainage of blood from the pleural cavity, the space-occupying effect of an accumulation of blood does not pose a direct danger unless the rare situation of a tension haemothorax is present. Only then is emergency chest drainage indicated. Tension haemothorax, however, commonly presents with similar signs and symptoms as tension pneumothorax (absent breath sounds on one side and severe respiratory and/or circulatory compromise).
Management of pneumothorax and tension pneumothorax
Tension pneumothorax can be treated with needle decompression, simple thoracostomy (without chest tube insertion), or tube thoracostomy. There are no comparative studies providing evidence of the superiority of one of these three modes of treatment.
From a pathophysiological perspective, sustained decompression requires that the amount of air that enters the pleural space during a spontaneous or mechanical breath be removed through the drainage device (regardless of the method used). Volumetric flow is proportional to the fourth power of the internal diameter of the needle. Needle decompression (or even single chest tube insertion, e.g. for the management of tracheobronchial injuries) can thus be ineffective if the lumen is too small for adequate drainage.
As a result of the low level of evidence for the various methods and benefit-risk profiles that can be used as a basis for a direct comparison of methods, treatment decisions should address practical aspects and potential risks and should therefore also consider the skills of prehospital care providers and the availability of drainage devices.
Thoracostomy
Chest tube insertion not only is an appropriate and highly effective (> 85%) procedure for the decompression of tension pneumothorax but is also associated with complications. It must be used when other measures fail or are inadequate. Usually, it is a definitive procedure and has the highest success rate. Prehospital pleural drainage was successfully used as a definitive procedure in 79–95% of cases [7, 14]. At the same time, pleural drainage was reported to have a mean failure rate of 11.2% because of incorrect positioning or insufficient effectiveness of the tube [7, 14] so that additional chest tube insertion was required. Chest tubes that are inserted in the prehospital setting are associated with significantly higher complication rates than those inserted in the hospital setting. Complications included subcutaneous tube placement (2.53% versus 0.39%), intraparenchymal tube placement (1.37% versus 0.63%), and intra-abdominal tube misplacement (0.87% versus 0.73%) [7, 14].
Simple thoracostomy (without chest tube insertion) is an appropriate, effective, and relatively rapid procedure for tension pneumothorax decompression. This technique, however, can only be used for patients undergoing positive pressure ventilation since pressure in the intrapleural space never becomes negative in these patients. Spontaneous ventilation generates negative intrapleural pressures that may be sufficient to suck air through the thoracostomy into the pleural cavity. In a case series involving 45 patients, simple thoracostomy was used in the prehospital setting and was found to be an effective treatment that did not cause relevant complications [42]. In a prospective observational study, 55 patients with 59 suspected pneumothoraces were treated with simple thoracostomy by a helicopter emergency medical service over a period of 2 years. Mean oxygen saturation increased after the procedure from 86.4 to 98.5%. A pneumothorax or a haemopneumothorax was found in 91.5% of the patients. The authors did not observe any cases of recurrent tension pneumothorax or major complications such as major bleeding, lung laceration, or pleural empyema [43]. A chest tube is then inserted through the thoracostomy in the hospital setting.
Controlled studies addressing the different techniques for chest tube insertion are not available. Most experts recommend the following standardised technique. Chest tubes must be placed using a sterile technique. Local and systemic analgesia must be used in patients who are not unconscious. A trocar should never be inserted blindly to guide the tube through the chest. Studies investigating the trocar technique reported higher complication rates than studies addressing the surgical technique (11.0% versus 1.6%) [7, 14]. In a prospective cohort study (of critically ill patients), the use of a trocar was also associated with a significantly higher rate of chest tube malposition [44].
Small catheters (≤ 14 Fr) are usually inserted using the Seldinger technique, and large-bore chest tubes using mini-thoracotomy. In addition, modified Seldinger techniques using consecutive dilation are also available for large-bore chest tubes [45, 46].
It is generally recommended that the tip of the chest tube be directed in a specific location: posterior and inferior chest tube placement for haemothorax, anterior and superior placement for pneumothorax. This recommendation has been challenged by a recent study that did not detect any effects of chest tube position on the rate of success (drainage of air and blood) [47].
Typical locations for chest tube placement in trauma patients are the second or third intercostal space (ICS) in the mid-clavicular line (MCL) and the fourth or fifth ICS in the mid-axillary line (MAL). Reliable data on differences in the success rates and complication rates for tube placement in the MCL (in the second or third ICS) versus tube placement in the MAL (in the region of the fifth ICS) are not available [7, 14]. For this reason, there is no site that can be recommended as the preferred location for tube placement.
Several recommendations regarding tube size can be provided. In a small randomised controlled study, tube-site pain was assessed immediately after tube insertion and on the two following days in patients with uncomplicated traumatic pneumothorax and no relevant haemothorax (patients were awake, able to consent, and haemodynamically stable). Patients who were treated with 14-Fr catheters had significantly lower tube-site pain scores than patients who were treated with 28-Fr chest tubes. Success and complication rates were similar in the two groups [48]. In a systematic review that was published in 2018 [49], no other randomised studies addressing traumatic pneumothorax were identified.
In a small, randomised study on patients with uncomplicated traumatic haemothorax (patients were awake, able to consent, and haemodynamically stable), failure rates were 10% for small-calibre (14-Fr) catheters and 17% for large-bore (28–32 Fr) chest tubes. There was no difference between the two groups in drainage volumes (600 mL versus 400 mL). Patients with 14-Fr catheters, however, reported a significantly better insertion experience [50]. These results confirmed trends that were reported in two retrospective studies [51, 52].
By contrast, all severely injured patients with haemothorax or haemopneumothorax (patients are haemodynamically unstable and unable to provide consent due to trauma) are treated with large-bore chest tubes [53,54,55,56]. These patients have an increased risk of a large fistula volume or a large amount of blood. Large-bore chest tubes are used to prevent chest tube blockage by blood clots. A prospective observational study involving a total of 353 chest tubes found no difference between smaller chest tubes (28–32 Fr) and larger chest tubes (> 36 Fr) in terms of retained haemothoraces and the need for additional tube insertion [57].
Patients who present with uncomplicated pneumothorax or haemothorax and who are haemodynamically stable and awake can be treated with 14-Fr drainage catheters. Patients who present with complicated pneumothorax or haemothorax and who are haemodynamically unstable or unable to provide consent due to trauma should be treated with larger chest tubes (24–32-Fr).
Needle decompression
Needle decompression is an appropriate and simple drainage procedure that is often effective (approximately 32–53%) but not free of complications [7, 14]. If the procedure fails or is insufficient, surgical decompression and/or chest tube insertion must be performed immediately. A failure rate of 58% was reported in a swine model. Causes were mechanical failure (due to kinking, obstruction, or dislodgment) within 5 min of placement or inadequate relief of tension [58]. In prehospital studies, needle decompression resulted in the release of air in 32–47% and clinical improvement in 12–60% of the patients who underwent needle decompression [17, 59, 60]. In 40% of cases, inadequate relief of tension required chest tube insertion after needle decompression. In other prehospital studies [59, 61], 53–67% of all patients were treated by needle decompression and subsequent chest tube insertion in the prehospital setting.
In two studies, total time on scene was significantly shorter (approximately 5 min) for patients treated with needle decompression (20.3 min) than for patients who underwent chest tube placement (25.7 min) [17, 59]. The time interval between the decision to perform decompression and successful decompression is more important than total time on scene. Needle decompression is the fastest method even for well-established teams and experienced surgeons. This applies to cases where prehospital providers are faced with nonoptimal conditions and have no relevant experience in chest tube insertion. For this reason, needle decompression is recommended as the first and fastest treatment for life-threatening tension pneumothorax. Needle decompression also appears to be an appropriate initial procedure in specific situations, for example when a patient is trapped or must be managed in adverse conditions (e.g. in underground tunnels).
If the first attempt at needle decompression is unsuccessful, a second attempt should not be made. Instead, thoracostomy should be performed immediately.
The Guideline Group is of the opinion that definitive treatment with mini-thoracotomy and chest tube insertion should be performed as soon as possible after successful needle decompression. Reasons for this are possible dislodgment, kinking, or obstruction of the needle during treatment, (re)positioning or transport as well as insufficient decompression in patients with large fistula volumes on positive pressure ventilation. This opinion is supported by a study in which 85% of patients required tube thoracostomy after needle decompression because of persistent symptoms or persistent pneumothorax on imaging [62].
Data on the size or type of cannula to be used are not available. A cannula with a diameter as large as possible (14 gauge or 12 gauge) is usually recommended to allow as much air as possible to be released.
Typical locations are the second or third intercostal space (ICS) in the mid-clavicular line (MCL), the fourth or fifth ICS in the mid-axillary line (MAL), and the fourth or fifth ICS in the anterior axillary line (AAL). In a meta-analysis, the mean distance from the skin surface to the pleural space was reported to be 34 mm (CI, 28–41 mm) at the AAL and was thus the shortest distance when compared to other sites [63]. The mean distance was 40 mm (CI, 29–51 mm) at the MAL and 43 mm (CI, 39–47 mm) at the MCL. As a result of the high level of heterogeneity among the studies included, however, these differences were not significant. In some studies, the distance at the MCL was reported to be even shorter than that at the MAL [7, 14]. The distance from the skin surface to the pleural space is significantly longer in women than in men [7, 14, 63]. In addition, there is a significant direct correlation between this distance and body mass index [64,65,66].
The use of a 3.2-cm cannula was associated with a failure rate of 65% [67]. Failure rates were considerably lower when a 5-cm cannula was used at the AAL (13%), MAL (31%), and MCL (38%) [63]. A failure rate of 89% was observed when a 5-cm cannula was used in obese patients (BMI > 30) [66].
A meta-analysis including 18 studies found that a catheter of at least 6.44 cm in length would be theoretically required to ensure that 95% of the patients would have penetration of the pleural space at the site of needle decompression [68]. In a study based on magnetic resonance imaging data from 2574 healthy volunteers who were representative of the population as a whole, Hecker et al. [69] found that decompression at an anterior location (MCL) might theoretically be successful in about 85% of cases when a 6.5-cm needle was used and in about 90% when a 7-cm needle was used. An evaluation of possible injuries to organs was limited to the internal mammary artery. The risks to this artery were assessed as minimal. There is, however, no clinical evidence of an improved success rate or a possible increase in procedure-related complications.
Success rates must be weighed against possible complications. A model-based study showed that, when an anterior location was used, there was a strong trend to performing needle decompression medial to the midclavicular line, which risked injuries to the heart, internal thoracic vessels, or other mediastinal vessels [70].
The longer the needle, the higher the risk of injuries to deep structures [7, 14, 63]. In a study based on CT images, the use of an 8-cm cannula could have led to injuries to vital structures in 32% of cases [64]. Clinical studies assessing the actual risks and benefits of longer versus normal cannulas are not available. The use of a 4.5-cm or 5-cm needle appears to have a relatively low risk of injuring vital structures but fails in at least one-third of cases. A longer needle (8 cm) is likely to achieve successful decompression in a larger number of cases but has a higher risk of injuries to vital structures (especially in association with left-sided procedures and lateral approaches).
Firm recommendations as to the most appropriate location of needle decompression cannot be made. Decisions as to the use of the MCL or AAL should be based on a patient’s individual anatomical features. The needle should have a minimum length of 5 cm. The optimum length of the cannula cannot be definitively determined. The use of a shorter cannula is associated with greater safety than the use of a longer cannula, which, however, has a higher success rate. Especially cannulas with a length of 8 cm or more must be expected to cause injuries to vital organs in up to 32% of cases [39].
Open pneumothorax
Experimental studies have shown that open pneumothorax or haemopneumothorax can be successfully managed with appropriate dressings. These dressings usually allow air and blood to escape from the chest and can thus prevent the development of a tension pneumothorax [71,72,73,74]. There is concern that dressings can fail due to poor adherence to wet skin, that they do not evacuate air and blood effectively, and that blood clogs the valve. Provisional dressings using plastic (packaging) film appear to be generally unsuitable [73, 74]. Commercially available dressings, too, were reported to differ widely in efficacy [71,72,73]. Chest seals with laminar venting channels may be the most effective devices. [72]
Limitations of the guideline
Patient values and preferences were sought but not received. The effect of this on the guideline is unclear, and there is a lack of research evidence on the effect of patient participation on treatment decisions or outcomes in the emergency setting.
Data availability
A full version of the guideline and its methods/evidence report are available online at https://register.awmf.org/de/leitlinien/detail/187-023
Abbreviations
- AAL :
-
Anterior axillary line
- ABCDE :
-
Airway, breathing, circulation, disability, exposure
- AWMF :
-
German Association of the Scientific Medical Societies
- BMI :
-
Body mass index
- CI :
-
Confidence interval
- CT :
-
Computed tomography
- GPP :
-
Good Practice Point
- ICS :
-
Intercostal space
- LoE :
-
Level of evidence
- MAL :
-
Mid-axillary line
- MCL :
-
Mid-clavicular line
- MRI :
-
Magnetic resonance imaging
- PICO :
-
Population, intervention, comparison, outcome
- PRISMA :
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT :
-
Randomised controlled trial
- TRISS :
-
Trauma and Injury Severity Score
References
Hoefer C, Lefereing R, Arbeitskreis TraumaRegister der Sektion Notfall- & Intensivmedizin und Schwerverletztenversorgung. Jahresbericht 2022 des TraumaregistersDGU® Akademie der Unfallchirurgie; 2022 [cited 2024 29.01.]. https://www.traumaregister-dgu.de/fileadmin/user_upload/TR-DGU-Jahresbericht_2022.pdf.
S3-Leitlinie Polytrauma/Schwerverletzten-Behandlung, Registernummer 187–023, Version 3.0. 2022. https://www.awmf.org/leitlinien/detail/ll/187-023.html. Accessed 29 Jan 2024
Chen Y, Yang K, Marusic A, Qaseem A, Meerpohl JJ, Flottorp S, et al. A reporting tool for practice guidelines in health care: the RIGHT Statement. Ann Intern Med. 2017;166(2):128–32. https://doi.org/10.7326/M16-1565.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF)-Ständige Kommission Leitlinien. AWMF-Regelwerk „Leitlinien“. 2nd Edition 2020. http://www.awmf.org/leitlinien/awmf-regelwerk.html. Accessed 11 November 2021.
Deutsche Gesellschaft für Unfallchirurgie e.V. (DGU). Leitlinienreport zur AWMF Leitlinie Polytrauma / Schwerverletzten-Behandlung, Registernummer 012–019 (2016). https://www.awmf.org/leitlinien/detail/ll/012-019.html. Accessed 21 March 2022.
Bouillon B, Marzi I. The updated German “Polytrauma - Guideline”: an extensive literature evaluation and treatment recommendation for the care of the critically injured patient. Eur J Trauma Emerg Surg. 2018;44(Suppl 1):1. https://doi.org/10.1007/s00068-018-0949-0.
Gliklich RE, Dreyer NA, Leavy MB, editors. Registries for evaluating patient outcomes: a user's guide [Internet]. 3rd ed. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014. Report No.: 13(14)-EHC111. PMID: 24945055.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4.
National Institute for Health and Care Excellence (NICE). The guidelines manual: Appendices B-I, Published: 30 November 2012. https://www.nice.org.uk/process/pmg6/resources/the-guidelines-manual-appendices-bi-2549703709. Last accessed March 21, 2022.
OCEBM Levels of Evidence Working Group*. Oxford Centre for Evidence-based Medicine Levels of Evidence (March 2009). https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009. Last accessed March 21, 2022. 2009.
Press. Prospective evaluation of prehospital trauma ultra-sound during aeromedical transport. J Emerg Med. 2014;47(6):638–45.
Quick JA, Uhlich RM, Ahmad S, Barnes SL, Coughenour JP. In-flight ultrasound identification of pneumothorax. Emerg Radiol. 2016;23(1):3–7. https://doi.org/10.1007/s10140-015-1348-z.
Waydhas C, Sauerland S. Pre-hospital pleural decompression and chest tube placement after blunt trauma: a systematic review. Resuscitation. 2007;72(1):11–25. https://doi.org/10.1016/j.resuscitation.2006.06.025.
Leigh-Smith S, Harris T. Tension pneumothorax - time for a re-think. Emerg Med J. 2005;22:8–16.
Committee on Trauma. Advanved Trauma Life Support (ATLS) - reference manual. Chicago: American College of Surgeons; 1997.
Barton E, Epperson M, Hoyt D, Fortlage D, Rosen P. Prehospital needle aspiration and tube thoracostomy in trauma victims: a six-year experience with aeromedical crews. J Emerg Med. 1995;13:155–63.
Chen SC, Markmann JF, Kauder DR, Schwab CW. Hemopneumothorax missed by auscultation in penetrating chest injury. J Trauma. 1997;42(1):86–9. https://doi.org/10.1097/00005373-199701000-00015.
Hirshberg A, Thomson SR, Huizinga WK. Reliability of physical examination in penetrating chest injuries. Injury. 1988;19(6):407–9. https://doi.org/10.1016/0020-1383(88)90135-0.
Thomson SR, Huizinga WK, Hirshberg A. Prospective study of the yield of physical examination compared with chest radiography in penetrating thoracic trauma. Thorax. 1990;45(8):616–9. https://doi.org/10.1136/thx.45.8.616.
Chan KK, Joo DA, McRae AD, Takwoingi Y, Premji ZA, Lang E, et al. Chest ultrasonography versus supine chest radiography for diagnosis of pneumothorax in trauma patients in the emergency department. Cochrane Database Syst Rev. 2020;7:CD013031. https://doi.org/10.1002/14651858.CD013031.pub2.
Staub LJ, Biscaro RRM, Kaszubowski E, Maurici R. Chest ultrasonography for the emergency diagnosis of traumatic pneumothorax and haemothorax: a systematic review and meta-analysis. Injury. 2018;49(3):457–66. https://doi.org/10.1016/j.injury.2018.01.033.
Press GM, Miller SK, Hassan IA, Alade KH, Camp E, Junco DD, et al. Prospective evaluation of prehospital trauma ultrasound during aeromedical transport. J Emerg Med. 2014;47(6):638–45. https://doi.org/10.1016/j.jemermed.2014.07.056.
Bokhari F, Brakenridge S, Nagy K, Roberts R, Smith R, Joseph K, et al. Prospective evaluation of the sensitivity of physical examination in chest trauma. J Trauma. 2002;53(6):1135–8. https://doi.org/10.1097/00005373-200212000-00017.
Collins J, Levine G, Waxman K. Occult traumatic pneumothorax: immediate tube thoracostomy versus expectant management. Am Surg. 1992;58:743–6.
Enderson B, Abdalla R, Frame S, Casey M, Gould H, Maull K. Tube thoracostomy for occult pneumothorax: a prospective randomized study of its use. J Trauma. 1993;35:726–9.
Brasel K, Stafford R, Weigelt J, Tenquist J, Borgstrom D. Treatment of occult pneumothoraces from blunt trauma. J Trauma. 1999;46:987–90.
Yadav K, Jalili M, Zehtabchi S. Management of traumatic occult pneumothorax. Resuscitation. 2010;81(9):1063–8. https://doi.org/10.1016/j.resuscitation.2010.04.030.
Kirkpatrick AW, Rizoli S, Ouellet JF, Roberts DJ, Sirois M, Ball CG, et al. Occult pneumothoraces in critical care: a prospective multicenter randomized controlled trial of pleural drainage for mechanically ventilated trauma patients with occult pneumothoraces. J Trauma Acute Care Surg. 2013;74(3):747–54. https://doi.org/10.1097/TA.0b013e3182827158. (discussion 54-5).
Moore FO, Goslar PW, Coimbra R, Velmahos G, Brown CV, Coopwood TB Jr, et al. Blunt traumatic occult pneumothorax: is observation safe?–results of a prospective, AAST multicenter study. J Trauma. 2011;70(5):1019–23. https://doi.org/10.1097/TA.0b013e318213f727. (discussion 23-5).
Roberts DJ, Leigh-Smith S, Faris PD, Blackmore C, Ball CG, Robertson HL, et al. Clinical presentation of patients with tension pneumothorax: a systematic review. Ann Surg. 2015. https://doi.org/10.1097/sla.0000000000001073.
Barton E. Tension pneumothorax. Curr Opin Pulm Med. 1999;5:269–74.
Rutherford RB, Hurt HH Jr, Brickman RD, Tubb JM. The pathophysiology of progressive, tension pneumothorax. J Trauma. 1968;8(2):212–27.
McPherson JJ, Feigin DS, Bellamy RF. Prevalence of tension pneumothorax in fatally wounded combat casualties. J Trauma. 2006;60(3):573–8.
Bushby N, Fitzgerald M, Cameron P, Marasco S, Bystrzycki A, Rosenfeld JV, et al. Prehospital intubation and chest decompression is associated with unexpected survival in major thoracic blunt trauma. Emerg Med Australas. 2005;17(5–6):443–9.
Mistry N, Bleetman A, Roberts KJ. Chest decompression during the resuscitation of patients in prehospital traumatic cardiac arrest. Emerg Med J. 2009;26(10):738–40. https://doi.org/10.1136/emj.2008.065599.
Huber-Wagner S, Lefering R, Qvick M, Kay MV, Paffrath T, Mutschler W, et al. Outcome in 757 severely injured patients with traumatic cardiorespiratory arrest. Resuscitation. 2007;75:276–85.
Kleber C, Giesecke MT, Tsokos M, Haas NP, Buschmann CT. Trauma-related preventable deaths in Berlin 2010: need to change prehospital management strategies and trauma management education. World J Surg. 2013;37(5):1154–61. https://doi.org/10.1007/s00268-013-1964-2.
Johnson G. Traumatic pneumothorax: is a chest drain always necessary? J Accid Emerg Med. 1996;13(3):173–4. https://doi.org/10.1136/emj.13.3.173.
Schmidt U, Stalp M, G T, Blauth M, Kimball I, Tscherne H. Chest decompression of blunt chest injuries by physician in the field: effectiveness and complications. J Trauma. 1998;44:98–100.
Aufmkolk M, Ruchholtz S, Hering M, Waydhas C, Nast-Kolb D, Unfallchirurgie ANdDGf. Wertigkeit der subjektiven Einschätzung der Thoraxverletzungsschwere durch den Notarzt. Unfallchirurg. 2003;106:746–53.
Deakin C, Davies G, Wilson A. Simple thoracostomy avoids chest drain insertion in prehospital trauma. J Trauma. 1995;39:373–4.
Massarutti D, Trillo G, Berlot G, Tomasini A, Bacer B, D’Orlando L, et al. Simple thoracostomy in prehospital trauma management is safe and effective: a 2-year experience by helicopter emergency medical crews. Eur J Emerg Med. 2006;13(5):276–80.
Remerand F, Luce V, Badachi Y, Lu Q, Bouhemad B, Rouby JJ. Incidence of chest tube malposition in the critically ill: a prospective computed tomography study. Anesthesiology. 2007;106(6):1112–9.
Nosher JL, Siegel R. Over-the-wire placement of large bore thoracostomy tubes. Cardiovasc Intervent Radiol. 1993;16(3):195–7.
Thal AP, Quick KL. A guided chest tube for safe thoracostomy. Surg Gynecol Obstet. 1988;167(6):517.
Benns MV, Egger ME, Harbrecht BG, Franklin GA, Smith JW, Miller KR, et al. Does chest tube location matter? An analysis of chest tube position and the need for secondary interventions. J Trauma Acute Care Surg. 2015;78(2):386–90. https://doi.org/10.1097/ta.0000000000000479.
Kulvatunyou N, Erickson L, Vijayasekaran A, Gries L, Joseph B, Friese RF, et al. Randomized clinical trial of pigtail catheter versus chest tube in injured patients with uncomplicated traumatic pneumothorax. Br J Surg. 2014;101(2):17–22. https://doi.org/10.1002/bjs.9377.
Chang SH, Kang YN, Chiu HY, Chiu YH. A Systematic review and meta-analysis comparing pigtail catheter and chest tube as the initial treatment for pneumothorax. Chest. 2018;153(5):1201–12. https://doi.org/10.1016/j.chest.2018.01.048.
Bauman ZM, Kulvatunyou N, Joseph B, Gries L, O’Keeffe T, Tang AL, et al. Randomized Clinical Trial of 14-French (14F) Pigtail catheters versus 28–32F chest tubes in the management of patients with traumatic hemothorax and hemopneumothorax. World J Surg. 2021;45(3):880–6. https://doi.org/10.1007/s00268-020-05852-0.
Maezawa T, Yanai M, Huh JY, Ariyoshi K. Effectiveness and safety of small-bore tube thoracostomy (</=20 Fr) for chest trauma patients: a retrospective observational study. Am J Emerg Med. 2020;38(12):2658–60. https://doi.org/10.1016/j.ajem.2020.09.028.
Tanizaki S, Maeda S, Sera M, Nagai H, Hayashi M, Azuma H, et al. Small tube thoracostomy (20–22 Fr) in emergent management of chest trauma. Injury. 2017;48(9):1884–7. https://doi.org/10.1016/j.injury.2017.06.021.
Beall AC Jr, Bricker DL, Crawford HW, Noon GP, De Bakey ME. Considerations in the management of penetrating thoracic trauma. J Trauma. 1968;8(3):408–17.
Hyde J, Sykes T, Graham T. Reducing morbidity from chest drains. BMJ. 1997;314(7085):914–5.
Symbas P. Chest drainage tubes. Surg Clin N Am. 1989;69:41–6.
Tomlinson MA, Treasure T. Insertion of a chest drain: how to do it. Br J Hosp Med. 1997;58(6):248–52.
Inaba K, Lustenberger T, Recinos G, Georgiou C, Velmahos GC, Brown C, et al. Does size matter? A prospective analysis of 28–32 versus 36–40 French chest tube size in trauma. J Trauma Acute Care Surg. 2012;72(2):422–7. https://doi.org/10.1097/TA.0b013e3182452444.
Martin M, Satterly S, Inaba K, Blair K. Does needle thoracostomy provide adequate and effective decompression of tension pneumothorax? J Trauma Acute Care Surg. 2012;73(6):1412–7. https://doi.org/10.1097/TA.0b013e31825ac511.
Davis DP, Pettit K, Rom CD, Poste JC, Sise MJ, Hoyt DB, et al. The safety and efficacy of prehospital needle and tube thoracostomy by aeromedical personnel. Prehospital Emerg Care : Off J Natl Assoc EMS Phys Natl Assoc State EMS Directors. 2005;9(2):191–7.
Eckstein M, Suyehara D. Needle thoracostomy in the prehospital setting. Prehospital Emerg Care : Off J Natl Assoc EMS Phys Natl Assoc State EMS Directors. 1998;2:132–5.
Coats T, Wilson A, Xeropotamous N. Pre-hospital management of patients with severe thoracic injury. Injury. 1995;26:581–5.
Dominguez KM, Ekeh AP, Tchorz KM, Woods RJ, Walusimbi MS, Saxe JM, et al. Is routine tube thoracostomy necessary after prehospital needle decompression for tension pneumothorax? Am J Surg. 2013;205(3):329–32. https://doi.org/10.1016/j.amjsurg.2013.01.004. (discussion 32).
Laan DV, Vu TD, Thiels CA, Pandian TK, Schiller HJ, Murad MH, et al. Chest wall thickness and decompression failure: a systematic review and meta-analysis comparing anatomic locations in needle thoracostomy. Injury. 2016;47(4):797–804. https://doi.org/10.1016/j.injury.2015.11.045.
Chang SJ, Ross SW, Kiefer DJ, Anderson WE, Rogers AT, Sing RF, et al. Evaluation of 8.0-cm needle at the fourth anterior axillary line for needle chest decompression of tension pneumothorax. J Trauma Acute Care Surg. 2014;76(4):1029–34. https://doi.org/10.1097/ta.0000000000000158.
Inaba K, Ives C, McClure K, Branco BC, Eckstein M, Shatz D, et al. Radiologic evaluation of alternative sites for needle decompression of tension pneumothorax. Arch Surg. 2012;147(9):813–8. https://doi.org/10.1001/archsurg.2012.751.
Powers WF, Clancy TV, Adams A, West TC, Kotwall CA, Hope WW. Proper catheter selection for needle thoracostomy: a height and weight-based criteria. Injury. 2014;45(1):107–11. https://doi.org/10.1016/j.injury.2013.08.026.
Ball CG, Wyrzykowski AD, Kirkpatrick AW, Dente CJ, Nicholas JM, Salomone JP, et al. Thoracic needle decompression for tension pneumothorax: clinical correlation with catheter length. Can J Surg J Can Chir. 2010;53(3):184–8.
Clemency BM, Tanski CT, Rosenberg M, May PR, Consiglio JD, Lindstrom HA. Sufficient catheter length for pneumothorax needle decompression: a meta-analysis. Prehosp Disaster Med. 2015;30(3):249–53. https://doi.org/10.1017/s1049023x15004653.
Hecker M, Hegenscheid K, Volzke H, Hinz P, Lange J, Ekkernkamp A, et al. Needle decompression of tension pneumothorax: population-based epidemiologic approach to adequate needle length in healthy volunteers in Northeast Germany. J Trauma Acute Care Surg. 2016;80(1):119–24. https://doi.org/10.1097/TA.0000000000000878.
Netto FA, Shulman H, Rizoli SB, Tremblay LN, Brenneman F, Tien H. Are needle decompressions for tension pneumothoraces being performed appropriately for appropriate indications? Am J Emerg Med. 2008;26(5):597–602.
Arnaud F, Tomori T, Teranishi K, Yun J, McCarron R, Mahon R. Evaluation of chest seal performance in a swine model: comparison of Asherman vs. Bolin seal. Injury. 2008;39(9):1082–8. https://doi.org/10.1016/j.injury.2008.03.003.
Kheirabadi BS, Terrazas IB, Miranda N, Voelker AN, Arnaud F, Klemcke HG, et al. Do vented chest seals differ in efficacy? An experimental evaluation using a swine hemopneumothorax model. J Trauma Acute Care Surg. 2017;83(1):182–9. https://doi.org/10.1097/TA.0000000000001501.
Kuhlwilm V. The use of chest seals in treating sucking chest wounds: a comparison of existing evidence and guideline recommendations. J Spec Oper Med. 2021;21(1):94–101.
Schachner T, Isser M, Haselbacher M, Schrocker P, Winkler M, Augustin F, et al. Rescue blanket as a provisional seal for penetrating chest wounds in a new ex vivo porcine model. Ann Thorac Surg. 2021. https://doi.org/10.1016/j.athoracsur.2021.06.083.
Acknowledgements
The authors would like to thank Lena Heinen, Simone Hess, Käthe Gooßen, and Dawid Pieper for their methodological support. We would also like to thank Barbara Isenberg from the German Office of Languages in Huerth for the linguistic advice. In addition, thanks go to all the delegates from the medical societies who were involved in the consensus conferences and to all contributors of the current German polytrauma guideline and their previous versions.
We acknowledge support by the Open Access Publication Funds of the University of Duisburg-Essen
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was funded by the German Society for Trauma Surgery (Deutsche Gesellschaft für Unfallchirurgie, DGU), a non-profit organisation. The guideline chair and several co-authors of this guideline topic are DGU members and contributed to the results in an interdisciplinary consensus process.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this work. B.P. and J.B. conducted the systematic literature search, reduced the data, and wrote the Supplementary Information. C.W. and B.P. (methods section) wrote the main paper, All authors devised the concept, interpreted and discussed the results, discussed its implications and the recommendations, and commented on the manuscript at all stages. All authors contributed extensively to the work presented in this paper.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was not required because the study used publicly accessible documents as evidence.
Competing interests
The authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Waydhas, C., Prediger, B., Kamp, O. et al. Prehospital management of chest injuries in severely injured patients—a systematic review and clinical practice guideline update. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02457-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02457-3