Abstract
Purpose
The study investigates changes in the injury characteristics of hospitalised children in a paediatric trauma centre during the COVID-19 pandemic.
Methods
Data from injured children from the pre-pandemic year 2019 were compared to the pandemic year 2020 using Pearson’s chi-squared test and the Mann–Whitney U test. The period of highly restrictive regulations (HRP) was evaluated separately. A comprehensive literature review with defined search terms resulted in a descriptive data synthesis.
Results
Data from 865 patients indicated reductions in admissions of 5.6% and 54.4% during the HRP. In 2020, the hospitalisation time was longer (2.2 ± 2.7 days in 2019 vs. 2.4 ± 2.6 in 2020, p = 0.045); the proportions of wounds requiring surgical therapy (p = 0.008) and of observational treatments, primarily for mild brain injuries (p = 0.046), were higher; and conservative treatments, primarily for contusions, were lower (p = 0.005). There were no significant changes in age, location of lesions, or frequency of surgical therapy; nor were there differences in the HRP, except for fewer injuries in school and kindergarten (p < 0.001). The literature review summarises the main results of 79 studies.
Conclusion
Limited resources did not alter the indications for surgical therapy. Further studies should examine whether the more common injuries sustained at home were caused by excessive work/childcare demands on parents. Reduced inpatient conservative treatment implies that hospital resources possibly were overused previously. The literature offers answers to many detailed questions regarding childhood injuries during a pandemic and more efficient safe treatment.
Registration Ethical committee of RWTH Aachen University EK 22-320; Center for Translational & Clinical Research RWTH Aachen University (CTC-A) 21-430.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
On March 11, 2020, the World Health Organization (WHO) declared COVID-19 a worldwide pandemic. The subsequent lockdown in 2020 resulted in a significant change in the locations and activities of children and adolescents compared to 2019. Therefore, it seems likely that injury patterns and frequencies among children also changed during this period. Many international studies have focused on the influence of the lockdown on the characteristics of childhood injuries and changes in their management during this time [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. However, to the best of our knowledge, no study has reported data from Germany regarding these aspects. Therefore, we aimed to report changes in admissions to the paediatric trauma centre of our university hospital in North Rhine-Westphalia/Germany as well as alterations in injury patterns and treatments.
We performed a comprehensive systematic literature search to place our results in the context of previously published international studies. We deliberately did not choose the format of a systematic literature review, with or without meta-analysis, so as not to restrict the inclusion criteria and thus provide an overview of the comprehensive number of studies on the most diverse aspects concerning this topic during this extraordinary period worldwide.
Methods
Patients admitted to the paediatric trauma centre of University Hospital RWTH Aachen
This part of the present study was performed according to the guidelines for reporting observational studies (STROBE) [32] and was approved and registered by the ethics committee of the University Hospital RWTH Aachen (project ID EK 22-320). The database of the Department of Orthopaedics, Trauma and Reconstructive Surgery, University Hospital RWTH Aachen/Germany (Level 1 trauma centre) was accessed. All patients younger than 18 years who were hospitalised with trauma diagnoses between January 1, 2019, and December 31, 2020, were included. Data from the pre-pandemic year January 1, 2019, to December 31, 2019, were compared to the pandemic year January 1, 2020, to December 31, 2020. In addition, the period of highly restrictive regulations (HRP), from the closure of kindergartens and schools until the reopening of both institutions, was evaluated separately (March 16, 2020, to June 7, 2020, versus the same period in 2019). The following endpoints were compared: length of hospitalisation, age of patients, place of lesion, type of lesion, activity during injury, and type of management. Observational treatments were carried out for injuries in which life-threatening conditions could occur after a symptom-free interval, i.e. traumatic brain injuries or blunt thoracic or abdominal injuries. Conservative treatment included injuries, mostly contusions and sprains, and more rarely fractures, that did not require surgical treatment, but which initially could not be treated at home due to severe pain and immobility.
The data were recorded in a database in Microsoft® Excel®. Statistical analyses were performed using the software IBM SPSS version 29. For the categorical variables, Pearson’s chi-squared test was used to determine whether there was a statistically significant difference between the expected frequencies and the observed frequencies of the contingency table. After checking for normality using the Shapiro–Wilk test, continuous data were analysed using the Mann–Whitney U test. Values of p < 0.05 were considered statistically significant.
Literature review
On April 29, 2023, a PubMed search was performed with the search terms and Boolean operators listed in Table 1. From the resulting 177 records, those that contained information on the development and care of children’s injuries before, during, and sometimes after the COVID-19 pandemic were selected. Ninety-two records that matched this topic were selected for full-text screening. In studies that included both adults and children, only data from children were considered. On September 26, 2023, a final search with the same scheme was done, and six further reports were found.
The records were reviewed according to the aspects author and publication year, study period, study institution/region, considered patients, and main findings regarding the following:
-
Trauma-associated paediatric surgery
-
Incidences/numbers of treated patients or injuries
-
Special injury types, locations, or aetiologies
-
Changes in the treatment process
Results
Patients admitted to the paediatric trauma centre of University Hospital RWTH Aachen
The data of 865 patients were collected: 445 from 2019 and 420 from 2020. Of these, 57 patients came to the trauma centre during the highly restricted period (HRP) in 2020 and 125 in the same period in 2019. We observed a 5.6% reduction in admissions over the entire 2020 and a 54.4% reduction in the HRP of 2020.
There was no significant difference in age between the two groups over the entire year or in looking only at the HRP. In the pandemic year 2020, the length of hospitalisation was longer compared to the pre-pandemic year 2019 (p = 0.045) (Table 2).
Regarding the place of the lesions, there were no differences either for the entire year or for the HRP (Table 3). There were also no differences in the type of lesions except during the pandemic year when significantly more wounds requiring surgical therapy were the reason for hospitalisation (Table 4).
In 2020, there was a significant reduction in admissions of patients with lesions that were treated conservatively (p = 0.005) and an increase of patients who were hospitalised for observation (p = 0.046). However, there was no significant change in surgical cases between the two entire years. In the HRP, no significant changes were observed in any of these aspects (Table 5). There was no significant difference in whether the injury took place during free time or school/kindergarten time over the entire years 2019 and 2020. However, this was significantly the case during the HRP (p < 0.001) (Table 6).
Reported results in literature
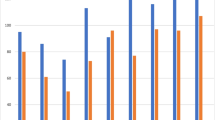
Using the above-mentioned search criteria, 79 publications dealing with paediatric patients presenting to trauma departments during the COVID-19 pandemic were identified. These studies are listed in Table 7 to Table 10 of the supplement, with a presentation of the main findings and the investigation period. Twenty studies commented on surgical aspects (Table 7), 28 studies on general treatment numbers (Table 8), 24 studies on specific injury regions or types (Table 9), and 7 studies on changes in the treatment process (Table 10). Most publications came from Europe, North America, and Asia (Fig. 1).
Changes in surgical management and absolute numbers of treated patients
In accordance with our results, most studies describe a decrease in the absolute numbers of treated patients or injuries during the lockdown in 2020 (Supplement, Table 8) and no significant change in the proportion of surgically managed patients (Supplement, Table 7) [1,2,3,4, 13, 14, 33,34,35,36,37]. However, in a few studies, divergent changes in surgical management, with either a preference for non-operative management of lower leg fractures [38] or a significantly elevated frequency of operative treatment during the lockdown [12, 39, 40], are described. Simon et al. reported altered management, without complications: elbow pins left protruding were removed in consultation rather than in the outpatient surgery room, as was done previously. Under general anaesthesia, only overriding frontally misaligned fractures of the distal quarter of the two forearm bones were reduced [27]. We did not change our surgical procedures for our patients in 2020.
Injury types, locations, and aetiologies (Supplement, Table 9)
Domestic injuries
Our results show a significant decrease in injuries sustained during the HRP in public facilities. In the literature, during the pandemic, the majority of studies reported an increase in the proportion of injuries occurring in the domestic environment [4, 8, 23, 26, 41,42,43,44], whereas the incidence of outdoor injuries acquired in public areas or in sports clubs significantly decreased [8, 23, 26, 42, 44, 45].
Sports-related injuries
In line with the above findings, sports-related injuries were less likely to occur during the lockdown [11, 15, 38, 41, 45,46,47]. It might be suggested that the nationwide lockdown and the cancellation of sports and other hobbies markedly decreased injuries among children aged 13–17 years, while the decrease was lower among younger children, as the cancellation of sports and hobbies did not affect patients in this age group as much as it did adolescents [13]. However, many studies have found a significantly younger age of patients requiring admission or surgery during the lockdown [2, 3, 5, 7,8,9, 12, 20, 25, 26, 29, 31, 34, 38, 39, 42, 46, 48,49,50]. Although not significantly, the mean age of our patients was also lower during the pandemic.
Fracture and injury patterns
In accordance with our results, in a study from Colorado, USA, there was no significant shift in the frequency of upper extremity fractures, lower extremity fractures, and axial/pelvic fractures [26]. However, some studies have shown a shift towards an increased occurrence of certain types of fractures in specific body regions [12, 14, 18, 38, 39] or a decrease in them [3, 12]. Other studies have reported that wound therapy was more common during the pandemic, as our study did [3, 8, 16, 20].
Mild traumatic brain injuries
The increase in mild traumatic brain injuries (commotio cerebri) only just missed the significance level in our patients. However, these injuries account for most hospitalised childhood injuries that present in our clinic for observation, and that proportion increased significantly in our patient population in 2020. Payr et al. also found a significant increase in mild traumatic brain injuries during the lockdown period [20].
Child abuse and neglect
Regarding non-accidental trauma (NAT), we have not yet carried out any analysis of our patients. However, the literature indicates that falls from windows were significantly elevated during the California-wide shelter-in-place mandate [51]. Some studies have reported significantly higher cases of child abuse and neglect during lockdown [9, 52]. Furthermore, the severity of abusive head trauma (AHT) worsened in 2021 in terms of mortality [53]. In contrast, McCauley et al. analysed American data and did not find significant changes in the frequency of NAT or the risk of fracture due to NAT [54]. Furthermore, no difference between positive/negative radiographic skeletal survey (SkS) rates was found [55, 56].
Vehicle accidents
We did not evaluate the detailed causes of these injuries in our patients, but there are reports that traffic restrictions resulted in a reduction in fractures associated with traffic accidents [48]. However, due to reduced public transport, children and young people were likely to use bicycles more often, so bicycle injuries were significantly higher during the pandemic [57,58,59,60].
Management aspects (Supplement, Table 10)
In our study, we did not examine possible changes in the treatment processes of injured children and adolescents. However, the literature contains some interesting findings in this regard, such as the higher effectiveness of conservative and surgical treatment processes.
In this context, changes in the management of conservatively treated fractures showed significant potential for cost savings through reduced numbers of clinic appointments and cast removals, without increased complication rates [61]. In terms of surgical management, the average waiting times for operations dropped significantly, with patients waiting 80% less time from the date of their injury [38]. Sabaghzadeh et al. also reported lower times for the transfer of patients to the operating room [43].
Memeo et al.’s study in Milan, Italy, found a reduction of paediatric visits to the ER, with an increased ‘positive’ fracture and surgery rate due to the government’s reorganisation of patient flow to hospitals, which involved the creation of more effective outpatient services, with only severe cases presenting to the ER [17]. Accordingly, Sugand et al. reported a greater use of outpatient telemedicine in the COVID-19 period, with more virtual fracture clinic use and, subsequently, fewer patients seen for consultation and followed up face to face [28]. These changes also explain the reduction in the proportion of negative studies (with no evidence of bone fractures in radiological diagnostics) by about one-fifth [62].
Further measures to reduce in-hospital care during the pandemic included the development of guidelines for the more efficient treatment of distal forearm fractures. There was high compliance with these guidelines after the pandemic [63]. Moreover, the increased use of easily accessible media for patient education has been shown to be effective regarding paediatric humeral supracondylar fractures during the pandemic [64].
Postpandemic period and further aspects in the literature
The years after 2020 were not considered in our study, but the literature shows interesting results for this period. For example, a trend towards decreased injuries persisted for 12 months after the peak of the pandemic [5], and the number of paediatric orthopaedic surgery visits did not return to prepandemic levels in 2021 [6]. In contrast, a study by Kalem et al. [35] found that after the first 3 months following the lockdown, the prevalence of outdoor traumas, high-energy traumas, the rate of patients treated with surgery, and the rate of admission to the emergency department were significantly higher than in the previous year. The authors assumed that children’s lower extremity muscle strength and neuromuscular control decreased after staying at home for a prolonged period. In addition, in investigating the reasons for a higher fracture rate, Lee et al. [65] found a higher prevalence of vitamin D deficiency in healthy Korean children with fractures during the pandemic.
Discussion
The data collected from hospitalised children in the paediatric trauma centre of our university hospital in North Rhine-Westphalia/Germany show that the COVID-19 lockdown in 2020 resulted in a 5.6% drop in treatments compared to 2019, without a significant change in the average age of patients, locations, and most types of injuries. However, the year-on-year comparison revealed a longer hospitalisation time, an increased proportion of wounds requiring surgical therapy, a lower proportion of conservative treatments, and an increased proportion of injuries that required observation. The proportion of surgical treatments did not change. Looking at the highly restrictive period (HRP) of the 12-week lockdown, the absolute number of cases fell by 54.4% compared to the respective period in 2019. Again, there were no differences in average patient age, hospitalisation length, location, type of lesion, or management. As expected, there was a highly significant difference in terms of whether the injuries occurred in school or kindergarten or outside these facilities.
Decreased absolute numbers of admitted and hospitalised children in paediatric traumatology departments during the pandemic are in accordance with the published literature (Supplement, Table 7 to Table 10), although in our population, this was only very clear in the HRP. The discussed and obvious reasons for this are the stay-at-home order and the associated lower exposure to injury-prone activities and settings that require a hospital visit (e.g. playgrounds, sports clubs, and traffic) [24].
The longer hospitalisation time in 2020 in our patient clientele can most likely be explained by a lack of resources among operating room staff due to high levels of sick leave over the entire year, meaning that patients waited longer for their operations. The slightly increased number of patients who had injuries that necessitated observation probably also resulted in longer hospital stays. Children who undergo surgery are usually discharged the day after the operation, while observations are usually scheduled for 48 h. The injuries observed in our department were mostly mild traumatic brain injuries, which increased in 2020, although the significance threshold was narrowly missed.
The increase in mild traumatic brain injuries is also reflected in the study by Payr et al. in Vienna, also a Level I trauma centre in Europe [20]. The authors explained that this change could be explained by the increased number of parents working from home who had to look after their children at the same time and who may not have been able to give them their full attention in order to avoid injuries. The significantly increased proportion of treated wounds in 2020 in our population may also be due to this fact, which Payr et al. and Mason et al. also observed [16, 20]. The question of why this is only statistically noticeable over the entire year and not just in the HRP probably has statistical reasons due to the lower number of patients during the HRP. However, working from home and video conferencing options were not yet established in Germany at the start of the lockdown, and possibilities to work from home in the official sense were only implemented later in the year. However, this hypothesis needs to be substantiated with a targeted study on the risk of injury among children who are cared for by people working from home.
Similar to our study, an unchanged proportion of fractures was also observed in the study from Vienna mentioned above [20], an excellent comparable study in which the authors compared the entire year of 2020 with previous years’ injuries at a Level 1 trauma centre. In our literature review, we included publications that dealt with childhood injuries during the pandemic, most of them from the USA and the UK. The reports regarding the decrease, or sometimes increase, in treated patients, injuries, rate of fractures, mild injuries, and number of surgical cases vary between the studies. The most likely reason for this is the different structure of the clinics or databases, their catchment areas, their capabilities or sizes, the period of study, and the differences in healthcare and insurance, as well as the statistical methods used.
Regarding childhood fractures, in 2022, Oh et al. [19] published a review of the epidemiology of paediatric fractures before and during the pandemic, which considered studies from all over the world [2,3,4, 25, 38, 39, 41, 48]. They concluded that fractures in adolescents due to sports activities decreased relative to those in younger children with more low-energy trauma. This shift is seen as the main reason for the younger mean age of injured children during the pandemic. In our patients, including not only fractures, the mean age in 2020 was also younger, but the significance level was not reached.
A further aspect is the significantly reduced proportion of conservative treatments in 2020 in our patients. Similar to other studies, it is probable that only children with major trauma were brought to the hospital by their parents to avoid exposure to the virus, whereas children with contusions and sprains were treated conservatively at home [7]. It is worth considering whether this might prove that inpatient resources could be conserved in a more restrictive inpatient admission regime. This aspect should be used as an opportunity to review the criteria for the hospitalisation of injured children as part of the restructuring of the healthcare system. Therefore, further studies are desirable. In this context, also safe outpatient treatment options have to be ensured. However, the concern that conservative treatment decisions may have been favoured due to the scarcity of resources in the operating room has not been confirmed. The idea that compromises were made in surgical decisions due to reduced resources is not supported by the published literature and our results. Only in the study of Darling et al. was a preference for non-operative management in lower limb fractures reported [38]. We were unable to find many studies that explicitly reported that patients who would have had surgery before the pandemic were treated conservatively during it. The changes in the number of surgical cases were more likely due to changes in injury patterns and absolute patient numbers.
The studies that examined the handling of patient volumes during the pandemic in more detail revealed interesting results in relation to more efficient procedures, particularly in the context of follow-up treatment and the use of X-rays without worsened outcomes [10, 28, 61,62,63]. Reduced mobility and more domestic activities are also sustainable factors to consider in bone health density in children during possible future lockdowns or in times of suspected reduced activity in children [35, 65, 66].
Our literature search revealed that this study is the only one to date to report data from a university paediatric trauma centre in Germany. The Robert Koch Institute (RKI) is the German government’s central scientific institution in the field of biomedicine. It is one of the most important bodies for safeguarding public health in Germany. On May 10, 2023, this institution published a 66-page report entitled ‘Monitoring of Children’s Health in (and after) COVID-19 Pandemic’, which described the situation that detailed data from Germany are missing [67]. We aim to contribute to closing this gap through our data.
Limitations
In our patient clientele, we compared only the entire years of 2019 and 2020, as well as the highly restricted period in 2020, with the respective period in 2019. To exclude annual fluctuations due to other causes, a comparison with the years before and after the pandemic would be interesting.
We examined only injuries that resulted in hospitalisation. This meant that the more serious injuries could be recorded reliably, the evaluation of a defined organizational structure was guaranteed, and, with manageable case numbers, a more detailed evaluation could be carried out on the basis of reviewed patient records, not just on the basis of DRGs. However, changes in injuries treated on an outpatient basis are also necessary to illuminate the findings.
Our data came from a Level 1 trauma centre that did not turn away injured children during the pandemic and had few restrictions or triages. This means that our data cannot be transferred to smaller hospitals. The investigation of the transfer behaviour from other hospitals to ours and the areas where children and families came from during this time would be interesting for future optimisation efforts in the healthcare system.
We have not performed a comprehensive, detailed analysis of the causes of injury, which may be desirable for future preventive considerations in a variety of areas. However, these data were not consistently stored in the medical records. It would be particularly interesting to look at child abuse and non-accidental trauma during this period.
In our search strategy, the use of the term ‘fracture’ probably excluded some studies only dealing with soft-tissue injuries, mild brain injuries, or others. However, this made comparability with our patient clientele more feasible.
Conclusions
When comparing childhood injuries in the entire years 2019 and 2020, as well as patient numbers, there were slight differences in our patients, although there is a downward trend, as can be seen in most published studies on this topic.
The indications for surgical treatment of childhood injuries are so strict and clear that no or only minor compromises towards conservative approaches were made, even with limited resources.
Further studies should examine whether childhood injuries sustained in the domestic environment and requiring hospitalisation were caused by excessive demands on parents or carers and simultaneous workloads especially when opportunities to work from home are increasingly being established in the future.
Reduced inpatient conservative treatment during the pandemic implies that hospital resources may have been overused previously. This means that as the healthcare system is restructured, ways could be found to ensure efficient outpatient treatment without compromising safety.
With strict inclusion and exclusion criteria, the existing literature has much potential to answer detailed questions regarding childhood injuries during a pandemic, as well as to highlight possible changes in treatment processes. These data should also be used to reduce the burden on emergency rooms and clinics when treating injured children, without reducing their safety.
Data availability
A de-identifed dataset associated with the paper is available upon reasonable request.
Abbreviations
- vs :
-
Versus
- ED :
-
Emergency department
- ER :
-
Emergency room
- SCH :
-
Supracondylar humerus
- SkS :
-
Radiographic skeletal survey
- BOAST :
-
British Orthopaedic Association Standards for Trauma and Orthopedics
- HRP :
-
Highly restricted period
- SD :
-
Standard deviation
- PCA :
-
Physical child abuse
- ISS :
-
Injury Severity Score
References
Abunayan A, Aljadaan B, Almudayfir M, Alshareef S, Alamer A. The effect of COVID-19 on orthopedic elective/emergency procedures in a tertiary hospital Riyadh Saudi Arabia A cross-sectional study. Ann Med Surg. 2022;81:104331. https://doi.org/10.1016/j.amsu.2022.104331. (Lond).
Baxter I, Hancock G, Clark M, Hampton M, Fishlock A, Widnall J, et al. Paediatric orthopaedics in lockdown: a study on the effect of the SARS-Cov-2 pandemic on acute paediatric orthopaedics and trauma. Bone Jt Open. 2020;1:424–30. https://doi.org/10.1302/2633-1462.17.BJO-2020-0086.R1.
Bolzinger M, Lopin G, Accadbled F, Sales de Gauzy J, Compagnon R. Pediatric traumatology in “green zone” during Covid-19 lockdown: a single-center study. Orthop Traumatol Surg Res. 2023;109:102946. https://doi.org/10.1016/j.otsr.2021.102946.
Bram JT, Johnson MA, Magee LC, Mehta NN, Fazal FZ, Baldwin KD, et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop. 2020;40:373–9. https://doi.org/10.1097/BPO.0000000000001600.
Butler LR, Abbott E, Mengsteab P, Dominy CL, Poeran J, Allen AK, Ranade SC. Epidemiology of pediatric trauma and fractures during and beyond the COVID-19 pandemic. J Child Orthop. 2023;17:322–31. https://doi.org/10.1177/18632521231180161.
Culbert AA, Ren BO, Maheshwer B, Curtis A, Ajayakumar J, Gilmore A, et al. Disparities in pediatric orthopedic surgery care during the COVID-19 pandemic pre-vaccine and post-vaccine availability. J Pediatr Orthop. 2023;43:529–35. https://doi.org/10.1097/BPO.0000000000002469.
Dibello D, Salvemini M, Amati C, Colella A, Graziano G, Vicenti G, et al. Trauma in children during lockdown for SARS-CoV-2 pandemic. A brief report. Children. 2021. https://doi.org/10.3390/children8121131. (Basel).
Gokhale S, D’sa P, Badurudeen AA, Carpenter EC. Epidemiology of paediatric orthopaedic trauma, before, during, and after the outbreak of COVID-19 pandemic: an observational study from a tertiary referral center in Wales. Cureus. 2021;13:e19253. https://doi.org/10.7759/cureus.19253.
Hennocq Q, Adjed C, Chappuy H, Orliaguet G, Monteil C, Kebir CE, et al. Injuries and child abuse increase during the pandemic over 12942 emergency admissions. Injury. 2022;53:3293–6. https://doi.org/10.1016/j.injury.2022.08.013.
Johnson MA, Ganley TJ, Crawford L, Swarup I. Pediatric orthopedic trauma care during the COVID-19 pandemic: a survey of the Pediatric Orthopedic Society of North America. HSS J. 2022;18:205–11. https://doi.org/10.1177/15563316211056022.
Keays G, Friedman D, Gagnon I. Les blessures au temps de la COVID-19. [Injuries in the time of COVID-19]. Health Promot Chronic Dis Prev Can. 2020;40:336–41. https://doi.org/10.24095/hpcdp.40.11/12.02.
Köksal A, Çamurcu Y, Dırvar F, Yapıcı F, Akgün H, Kaya O. COVID-19 pandemisi karantina döneminde pediatrik kırıkların özelliklerinin değerlendirilmesi. [An evaluation of the characteristics of orthopedic pediatric traumas during the COVID-19 pandemic lockdown period]. Ulus Travma Acil Cerrahi Derg. 2022;28:94–8. https://doi.org/10.14744/tjtes.2020.67681.
Kuorikoski J, Kuitunen I, Uimonen M, Mattila VM, Ponkilainen V. Incidence of pediatric injury visits decreased while trauma surgeries remained stable during the first and second waves of the COVID-19 pandemic in Finland: a register-based study. World J Pediatr Surg. 2021;4:e000304. https://doi.org/10.1136/wjps-2021-000304.
Lapsa J, Bukola Badaki O, Xu A, Eaton C, Lee RJ, Ryan L. The COVID-19 pandemic: effects on pediatric fracture patterns in the emergency department and subspecialty follow-up care. J Pediatr Orthop. 2022;42:582–8. https://doi.org/10.1097/BPO.0000000000002222.
Markiewitz ND, Garcia-Munoz J, Lilley BM, Oduwole S, Shah AS, Williams BA. Epidemiologic changes in pediatric fractures presenting to emergency departments during the COVID-19 pandemic. J Pediatr Orthop. 2022;42:e815–20. https://doi.org/10.1097/BPO.0000000000002194.
Mason B, Stott S, Beamish R. Reduced presentations with fractures or orthopaedic infections to a major children’s hospital during a national COVID-19 elimination strategy. ANZ J Surg. 2022;92:206–11. https://doi.org/10.1111/ans.17354.
Memeo A, Priano D, Caldarini C, Trezza P, Laquidara M, Montanari L, Randelli P. How the pandemic spread of COVID-19 affected children’s traumatology in Italy: changes of numbers, anatomical locations, and severity. Minerva Pediatr. 2020. https://doi.org/10.23736/S0026-4946.20.05910-1.
Nabian MH, Vosoughi F, Najafi F, Khabiri SS, Nafisi M, Veisi J, et al. Epidemiological pattern of pediatric trauma in COVID-19 outbreak: data from a tertiary trauma center in Iran. Injury. 2020;51:2811–5. https://doi.org/10.1016/j.injury.2020.09.015.
Oh CH, Yoon S, Ko KR, Kwon YW, Kim KM, Park HS, et al. Epidemiology of pediatric fractures before versus during the coronavirus disease 2019 pandemic. Clin Exp Pediatr. 2022;65:330–6. https://doi.org/10.3345/cep.2021.01767.
Payr S, Schuller A, Dangl T, Scheider P, Sator T, Chocholka B, et al. Maintaining medical resources to treat paediatric injuries during COVID-19 lockdown is essential–an epidemiological analysis of a Level 1 Trauma Centre in Central Europe. Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph18115829.
Pepper MP, Leva E, Trivedy P, Luckey J, Baker MD. Analysis of pediatric emergency department patient volume trends during the COVID-19 pandemic. Medicine. 2021;100:e26583. https://doi.org/10.1097/MD.0000000000026583. (Baltimore).
Raitio A, Ahonen M, Jääskelä M, Jalkanen J, Luoto TT, Haara M, et al. Reduced number of pediatric orthopedic trauma requiring operative treatment during COVID-19 restrictions: a nationwide cohort study. Scand J Surg. 2021;110:254–7. https://doi.org/10.1177/1457496920968014.
Rasmussen MK, Larsen P, Rölfing JD, Kirkegaard BL, Thorninger R, Elsoe R. Epidemiology and incidence of paediatric orthopaedic trauma workload during the COVID-19 pandemic: a multicenter cohort study of 3171 patients. World J Orthop. 2022;13:70–7. https://doi.org/10.5312/wjo.v13.i1.70.
Rougereau G, Guedj R, Irtan S, Qassemyar Q, Vialle R, Langlais T. Emergency department visits for pediatric traumatic injuries during general confinement: a single-center study in an urban setting. Arch Pediatr. 2021;28:249–51. https://doi.org/10.1016/j.arcped.2021.02.012.
Ruzzini L, de Salvatore S, Lamberti D, Maglione P, Piergentili I, Crea F, et al. COVID-19 changed the incidence and the pattern of pediatric traumas: a single-centre study in a pediatric emergency department. Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph18126573.
Shaw KG, Salton RL, Carry P, Hadley-Miller N, Georgopoulos G. Multi-day delay to care identified in pediatric trauma cases during COVID-19. J Pediatr Orthop B. 2022;31:e56–64. https://doi.org/10.1097/BPB.0000000000000910.
Simon A-L, Kassab Hassan S, Julien-Marsollier F, Happiette A, Jehanno P, Delvaque J-G, Ilharreborde B. Descriptive analysis of pediatric orthopedic surgical emergencies during the COVID-19 lockdown: single-center observational study in a pandemic red-zone area in France. Orthop Traumatol Surg Res. 2023;109:103088. https://doi.org/10.1016/j.otsr.2021.103088.
Sugand K, Park C, Morgan C, Dyke R, Aframian A, Hulme A, et al. Impact of the COVID-19 pandemic on paediatric orthopaedic trauma workload in central London: a multi-centre longitudinal observational study over the “golden weeks.” Acta Orthop. 2020;91:633–8. https://doi.org/10.1080/17453674.2020.1807092.
Verdoni F, Ricci M, Di Grigoli C, Rossi N, Lombardo MDM, Curci D, et al. Effect of the COVID-19 outbreak on pediatric patients’ admissions to the emergency department in an Italian orthopedic trauma hub. Children. 2021. https://doi.org/10.3390/children8080645. (Basel).
Verma V, Mahendra M. Epidemiology of pediatric musculoskeletal trauma patients admitted to the trauma center of King George’s Medical University (KGMU) during COVID-19-induced lockdown. Cureus. 2022;14:e23648. https://doi.org/10.7759/cureus.23648.
Zacay G, Modan-Moses D, Tripto-Shkolnik L, Levy-Shraga Y. Decreases in pediatric fractures during the COVID-19 pandemic – a nationwide epidemiological cohort study. Eur J Pediatr. 2022;181:1473–80. https://doi.org/10.1007/s00431-021-04323-5.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening of the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008.
Elbardesy H, Meagher E, Guerin S. Impact of the COVID-19 pandemic on the trauma and orthopaedic department at level one major trauma centre in the republic of Ireland. Acta Orthop Belg. 2021;87:571–8.
Hampton M, Clark M, Baxter I, Stevens R, Flatt E, Murray J, Wembridge K. The effects of a UK lockdown on orthopaedic trauma admissions and surgical cases: a multicentre comparative study. Bone Jt Open. 2020;1:137–43. https://doi.org/10.1302/2633-1462.15.BJO-2020-0028.R1.
Kalem M, Özbek EA, Kocaoğlu H, Merter A, Karaca MO, Şahin E, Başarir K. The increase in paediatric orthopaedic trauma injuries following the end of the curfew during the COVID-19 period. J Child Orthop. 2021;15:409–14. https://doi.org/10.1302/1863-2548.15.210071.
Olech J, Ciszewski M, Morasiewicz P. Epidemiology of distal radius fractures in children and adults during the COVID-19 pandemic – a two-center study. BMC Musculoskelet Disord. 2021;22:306. https://doi.org/10.1186/s12891-021-04128-5.
Yavuz İA, Kahve Y, Aydin T, Gencer B, Bingöl O, Yıldırım AÖ. Comparison of the first and second waves of the COVID-19 pandemic with a normal period in terms of orthopaedic trauma: data from a level 1 trauma centre. Acta Orthop Traumatol Turc. 2021;55:391–5. https://doi.org/10.5152/j.aott.2021.21117.
Darling J, Nowicka M, Niazi N, Pillai A. The effect of COVID-19 lockdowns on paediatric lower limb orthopaedic presentations. Arch Orthop Trauma Surg. 2022;142:3193–200. https://doi.org/10.1007/s00402-021-04103-8.
Turgut A, Arlı H, Altundağ Ü, Hancıoğlu S, Egeli E, Kalenderer Ö. Effect of COVID-19 pandemic on the fracture demographics: data from a tertiary care hospital in Turkey. Acta Orthop Traumatol Turc. 2020;54:355–63. https://doi.org/10.5152/j.aott.2020.20209.
Hernigou J, Morel X, Callewier A, Bath O, Hernigou P. Staying home during “COVID-19” decreased fractures, but trauma did not quarantine in one hundred and twelve adults and twenty-eight children and the “tsunami of recommendations” could not lockdown twelve elective operations. Int Orthop. 2020;44:1473–80. https://doi.org/10.1007/s00264-020-04619-5.
Gumina S, Proietti R, Villani C, Carbone S, Candela V. The impact of COVID-19 on shoulder and elbow trauma in a skeletally immature population: an Italian survey. JSES Int. 2021;5:3–8. https://doi.org/10.1016/j.jseint.2020.08.003.
Soriano KKJ, Sabatini CS, Brar RK, Jagodzinski JE, Livingston KS. New injury patterns in pediatric supracondylar fractures during COVID-19: beds are the new monkey bars. J Pediatr Orthop. 2023;43:198–203. https://doi.org/10.1097/BPO.0000000000002350.
Sabaghzadeh A, Bonakdar S, Ebrahimpour A, Khoshkholghsima M, Gorji M, Soufiabadi K, Gholipour M. The effect of COVID-19 pandemic on the characteristics of pediatric supracondylar fracture: a retrospective cohort study. Adv Biomed Res. 2022;11:100. https://doi.org/10.4103/abr.abr_49_21.
Gornick BR, Mostamand M, Thomas ES, Weber M, Schlechter JA. COVID-19 pandemic restrictions unmasks dangers of frequent injury mechanisms for common surgically treated pediatric fractures. J Child Orthop. 2022;16:83–7. https://doi.org/10.1177/18632521221090135.
Sephton BM, Mahapatra P, Shenouda M, Ferran N, Deierl K, Sinnett T, et al. The effect of COVID-19 on a major trauma network. An analysis of mechanism of injury pattern, referral load and operative case-mix. Injury. 2021;52:395–401. https://doi.org/10.1016/j.injury.2021.02.035.
Johnson MA, Halloran K, Carpenter C, Pascual-Leone N, Parambath A, Sharma J, et al. Changes in pediatric sports injury presentation during the COVID-19 pandemic: a multicenter analysis. Orthop J Sports Med. 2021;9:23259671211010824. https://doi.org/10.1177/23259671211010826.
Wild JT, Kamani YV, Bryan JM, Hartman TN, Spirov LM, Patel NM. Timeout? The epidemiology of pediatric sports injuries during the COVID-19 pandemic. J Am Acad Orthop Surg Glob Res Rev. 2022. https://doi.org/10.5435/JAAOSGlobal-D-21-00092.
Li J, Yuan X, Cao Y, Liu T, Gou P, Li X, et al. The effects of home confinement on pediatric fractures during the COVID 19 outbreak. Ital J Pediatr. 2021;47:142. https://doi.org/10.1186/s13052-021-01092-7.
Payr S, Dangl T, Schuller A, Scheider P, Chocholka B, Jaindl M, et al. Course of treatment and short-term outcome of surgically treated paediatric upper limb fractures during the COVID-19 pandemic–experiences of a Level 1 Trauma Centre in Central Europe. Children. 2022. https://doi.org/10.3390/children9020172. (Basel).
SalomTaverner M, MartíCiruelos R, FernándezAnsorena A, Alvarez Muñoz M, García-Chamorro M, Muñoz López C, SanperaTrigueros I. Translated article. Effect of the COVID pandemic on paediatric trauma emergencies in three areas of Spain with different incidences. Rev Esp Cir Ortop Traumatol. 2022;66:T43–50. https://doi.org/10.1016/j.recot.2022.07.017.
Theodorou CM, Brown EG, Jackson JE, Castle SL, Chao SD, Beres AL. Unintended consequences of COVID-19 on pediatric falls from windows: a multicenter study. J Surg Res. 2022;279:187–92. https://doi.org/10.1016/j.jss.2022.05.022.
Kovler ML, Ziegfeld S, Ryan LM, Goldstein MA, Gardner R, Garcia AV, Nasr IW. Increased proportion of physical child abuse injuries at a level I pediatric trauma center during the Covid-19 pandemic. Child Abuse Negl. 2021;116:104756. https://doi.org/10.1016/j.chiabu.2020.104756.
Lãzãrescu A-M, Benichi S, Blauwblomme T, Beccaria K, Bourgeois M, Roux C-J, et al. Abusive head trauma in infants during the COVID-19 pandemic in the Paris metropolitan area. JAMA Netw Open. 2022;5:e2226182. https://doi.org/10.1001/jamanetworkopen.2022.26182.
McCauley KL, Kaelber DC, Mistovich RJ. Did the COVID-19 pandemic lead to increased pediatric musculoskeletal nonaccidental trauma? A cross-sectional study. J Pediatr Orthop B. 2023;32:192–6. https://doi.org/10.1097/BPB.0000000000000971.
Henry MK, Wood JN, Bennett CE, Chaiyachati BH, Egbe TI, Otero HJ. Child abuse imaging and findings in the time of COVID-19. Pediatr Emerg Care. 2022;38:65–9. https://doi.org/10.1097/PEC.0000000000002630.
Stivaros S, Paddock M, Rajai A, Cliffe H, Connolly DJ, Dineen RA, et al. Rate and severity of radiological features of physical abuse in children during the first UK-wide COVID-19 enforced national lockdown. Arch Dis Child. 2022;107:575–81. https://doi.org/10.1136/archdischild-2021-323444.
Moore A, Singleton A, Hiatt L, Miller R, Phillips S, Leskovan JJ. An assessment of the impact of SARS-CoV-2 on a Level 1 Trauma Center including subgroup analysis of orthopedic injuries and mechanism of injury. Cureus. 2022;14:e20954. https://doi.org/10.7759/cureus.20954.
Auger N, Lewin A, Brousseau É, Ayoub A, Blaser C, Luu TM. Les confinements et les blessures à vélo : une analyse temporelle des taux de blessures au Québec au cours de la première année de la pandémie. [Lockdowns and cycling injuries: temporal analysis of rates in Quebec during the first year of the pandemic]. Health Promot Chronic Dis Prev Can. 2023;43:330–7. https://doi.org/10.24095/hpcdp.43.7.03.
Heitz P-H, Gravel J, Jourdain N, Hupin M, Nault M-L. Are outdoor playgrounds the real culprit for elbow fractures in children? A lesson learned from COVID-19 sanitary measures. Can J Surg. 2023;66:E282–8. https://doi.org/10.1503/cjs.022521.
Shack M, Davis AL, Zhang EWj, Rosenfield D. Bicycle injuries presenting to the emergency department during COVID-19 lockdown. J Paediatr Child Health. 2022;58:600–3. https://doi.org/10.1111/jpc.15775.
Hancock GE, Baxter I, Balachandar V, Flowers MJ, Evans OG. What can we learn from COVID-19 protocols with regard to management of nonoperative pediatric orthopaedic injuries? J Pediatr Orthop. 2021;41:e600–4. https://doi.org/10.1097/BPO.0000000000001885.
Bottari G, Stellacci G, Ferorelli D, Dell’Erba A, Aricò M, Benevento M, et al. Imaging appropriateness in pediatric radiology during COVID-19 pandemic: a retrospective comparison with no COVID-19 period. Children. 2021. https://doi.org/10.3390/children8060463. (Basel).
Fink BE, Pinjala MT, Gomes KP, Mason WT. Early management of paediatric wrist and forearm fractures in a busy district general hospital emergency department: a retrospective cohort comparison study and audit of BOAST guidelines. Cureus. 2023;15:e41325. https://doi.org/10.7759/cureus.41325.
Zhu Z, Zheng Y, Zhu D. Douyin as a source of information and education on humeral supracondylar fracture of children during the COVID-19 pandemic in Chinese Mainland: an observational study. Medicine. 2023;102:e34104. https://doi.org/10.1097/MD.0000000000034104. (Baltimore).
Lee Y-S, Lee S-U, Hong TM, Joo SY. Prevalence of Vitamin D deficiency in children with fractures: before and during the COVID-19 outbreak. Int J Clin Pract. 2022;2022:4410032. https://doi.org/10.1155/2022/4410032.
Köksal A, Öner A, Çimen O, Akgün H, Kocaoğlu A, Yapıcı F. Adolescent tibial tubercle fractures in the time of the COVID 19: a single orthopedic trauma center experience. J Orthop Sci. 2022;27:1114–9. https://doi.org/10.1016/j.jos.2021.06.002.
RKI. (2023). 4. QUARTALSBERICHT - KINDERGESUNDHEIT IN DEUTSCHLAND AKTUELL (KIDA). https://www.rki.de/DE/Content/Gesundheitsmonitoring/Studien/Kida/4-Quartalsbericht-KIDA.pdf. Accessed 13 Oct 2023.
Carkci E, Polat B, Polat A, Peker B, Öztürkmen Y. The effect of the coronavirus 2019 (COVID-19) pandemic on the number and characteristics of orthopedic trauma patients in a tertiary care hospital in Istanbul. Cureus. 2021;13:e12569. https://doi.org/10.7759/cureus.12569.
Kalem M, Kocaoğlu H, Merter A, Karaca MO, Özbek EA, Kınık HH. Effects of COVID-19 pandemic curfew on orthopedic trauma in a tertiary care hospital in Turkey. Acta Orthop Traumatol Turc. 2021;55:191–5. https://doi.org/10.5152/j.aott.2021.20263.
Karia M, Gupta V, Zahra W, Dixon J, Tayton E. The effect of COVID-19 on the trauma burden, theatre efficiency and training opportunities in a district general hospital: planning for a future outbreak. Bone Jt Open. 2020;1:494–9. https://doi.org/10.1302/2633-1462.18.BJO-2020-0074.R1.
Murphy T, Akehurst H, Mutimer J. Impact of the 2020 COVID-19 pandemic on the workload of the orthopaedic service in a busy UK district general hospital. Injury. 2020;51:2142–7. https://doi.org/10.1016/j.injury.2020.07.001.
Choi A, Bae W, Kim K, Kim S. Impact of Covid-19 on the visits of pediatric patients with injuries to the emergency department in Korea. Children. 2021. https://doi.org/10.3390/children8070568. (Basel).
Dhillon MS, Kumar D, Saini UC, Bhayana H, Gopinathan NR, Aggarwal S. Changing pattern of orthopaedic trauma admissions during COVID-19 pandemic: experience at a tertiary trauma centre in India. Indian J Orthop. 2020;54:374–9. https://doi.org/10.1007/s43465-020-00241-0.
Greenhalgh M, Dupley L, Unsworth R, Boden R. Where did all the trauma go? A rapid review of the demands on orthopaedic services at a UK Major Trauma Centre during the COVID-19 pandemic. Int J Clin Pract. 2021;75:e13690. https://doi.org/10.1111/ijcp.13690.
Hashmi PM, Zahid M, Ali A, Naqi H, Pidani AS, Hashmi AP, Noordin S. Change in the spectrum of orthopedic trauma: effects of COVID-19 pandemic in a developing nation during the upsurge; a cross-sectional study. Ann Med Surg. 2020;60:504–8. https://doi.org/10.1016/j.amsu.2020.11.044. (Lond).
Lv H, Zhang X, Wang J, Hou Z, Wang H, Li C, et al. Short-term effects of COVID-19 on the risk of traumatic fractures in China cities. Sci Rep. 2022;12:6528. https://doi.org/10.1038/s41598-022-10531-2.
Qian C, Zheng Y, Meng J, Li H, Wang D. A cross-sectional study on the impact of the prevention and control response of the COVID-19 pandemic on minor’s orthopedic trauma in Shanghai. Arch Public Health. 2021;79:145. https://doi.org/10.1186/s13690-021-00672-7.
Toy S, Polat O, Özbay H. Coronavirus disease 2019 pandemic, restriction, and orthopedic trauma: retrospective observational study. Medicine. 2021;100:e27166. https://doi.org/10.1097/MD.0000000000027166. (Baltimore).
Albright JA, Rebello E, Kosinski LR, Patel DD, Spears JR, Gil JA, Katarincic JA. Characterization of the epidemiology and risk factors for hand fractures in patients aged 1 to 19 presenting to United States emergency departments: a retrospective study of 21,031 cases. J Pediatr Orthop. 2022;42:335–40. https://doi.org/10.1097/BPO.0000000000002164.
Benmassaoud Z, Balde FB, Oudghiri Z, Charki MT, Abdellaoui H, Atarraf K, Afifi MA. Impact of the COVID-19 lockdown on the epidemiologic and clinic profiles of domestic accidents in children. Afr J Paediatr Surg. 2022;19:65–7. https://doi.org/10.4103/ajps.AJPS_49_21.
Gupta R, Singhal A, Kapoor A, Dhillon M, Masih GD. Effect of COVID-19 on surgical management of open fractures and infection rates: a tertiary care experience in Indian set-up. J Clin Orthop Trauma. 2021;12:16–21. https://doi.org/10.1016/j.jcot.2020.10.050.
Klepacki K, Tomczyk Ł, Miękisiak G, Morasiewicz P. The effect of the Covid-19 pandemic on the epidemiology of ankle joint injuries in adults and children. Ortop Traumatol Rehabil. 2022;24:363–73. https://doi.org/10.5604/01.3001.0016.2318.
Schultz JD, Windmueller R, Rees AB, Wollenman LC, Lempert NL, Schoenecker JG, Moore-Lotridge SN. Impact of the COVID-19 pandemic on pediatric elbow fractures: marked change in management and resource utilization, without a change in incidence. J Pediatr Orthop. 2022;42:401–7. https://doi.org/10.1097/BPO.0000000000002205.
Springthorpe T, Pearce M, Nowicka M, Niazi N, Pillai A. The relationship of the COVID-19 pandemic with the incidence and management of upper limb fractures: double-centre study. Arch Bone Jt Surg. 2022;10:871–6. https://doi.org/10.22038/ABJS.2022.59285.2929.
Walker LC, Hamad F, Wilson C, O’Connor D, Richards SW, Southgate JJ. Types, management and complications in paediatric distal radial fractures sustained during COVID-19 lockdown. J Hand Surg Eur. 2022;47:605–9. https://doi.org/10.1177/1753193422107430.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
HD conceptualisation; methodology; supervision of data collection, data evaluation, and statistical analysis; comprehensive literature review; writing; EL comprehensive data collection and evaluation, statistical analysis; FM early conceptualisation and methodology, review; NB review; FH supervision; writing and review.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Delbrück, H., Lambertz, E., Migliorini, F. et al. Influence of COVID-19 pandemic on hospitalisations at a paediatric traumatology department during 2020: a single-centre observational study and comprehensive literature review. Eur J Trauma Emerg Surg 50, 591–601 (2024). https://doi.org/10.1007/s00068-024-02453-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-024-02453-7