Abstract
Background
Both dementia and frailty have been associated with worse outcomes in patients with hip fractures. However, the interrelation and predictive value of these two entities has yet to be clarified. The current study aimed to investigate the predictive relationship between dementia, frailty, and in-hospital mortality after hip fracture surgery.
Methods
All patients registered in the 2019 National Inpatient Sample Database who were 50 years or older and underwent emergency hip fracture surgery following a traumatic fall were eligible for inclusion. Logistic regression (LR) models were constructed with in-hospital mortality as the response variables. One model was constructed including markers of frailty and one model was constructed excluding markers of frailty [Orthopedic Frailty Score (OFS) and weight loss]. The feature importance of all variables was determined using the permutation importance method. New LR models were then fitted using the top ten most important variables. The area under the receiver-operating characteristic curve (AUC) was used to compare the predictive ability of these models.
Results
An estimated total of 216,395 patients were included. Dementia was the 7th most important variable for predicting in-hospital mortality. When the OFS and weight loss were included, they replaced dementia in importance. There was no significant difference in the predictive ability of the models when comparing the model that included markers of frailty [AUC for in-hospital mortality (95% CI) 0.79 (0.77–0.81)] with the model that excluded markers of frailty [AUC for in-hospital mortality (95% CI) 0.79 (0.77–0.80)].
Conclusion
Dementia functions as a surrogate for frailty when predicting in-hospital mortality in hip fracture patients. This finding highlights the importance of early frailty screening for improvement of care pathways and discussions with patients and their families in regard to expected outcomes.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Background
The high risk of mortality and morbidity after hip fracture surgery remains a healthcare concern, with reported post-operative mortality as high as 10% and 27% at 30-days and 1-year, respectively [1, 2]. Up to 20% of patients with hip fracture have a dementia diagnosis, [3], and it has been established that this group is disproportionally at risk for postoperative adverse outcomes [4, 5]. Due to the global increase in life expectancy with an aging population, it is anticipated there will be an increase in patients suffering from both hip fractures and dementia [6].
A recent large study using data from the national Swedish Hip Fracture registry found that dementia was a surrogate for frailty when predicting postoperative mortality in hip fracture patients. Furthermore, the presence of dementia in a patient without frailty did not appreciably contribute to the prediction of postoperative mortality [7]. This finding is important for resource allocations, perioperative care management, discussions in regards to expected outcomes with patients and their relatives, as well as in outcome research investigations in this patient population. Using the United States National Inpatient Sample (NIS) database, the authors endeavor to validate these findings. The objective was to investigate whether dementia serves the same purpose as frailty when predicting in-hospital mortality following a traumatic hip fracture. The hypothesis was that dementia would function as a surrogate for frailty when predicting mortality.
Methods
The current study utilized data from the 2019 United States NIS, which is recognized as the largest all-payer inpatient database in the United States. The NIS is overseen by the Agency for Healthcare Research and Quality, and it surveys 20% of all hospitalizations in the country to ensure accurate national estimates for 97% of all inpatient hospitalizations in the United States through validated sampling algorithms with discharge and survey weight. [8]. To ensure adherence to rigorous scientific reporting standards, the study complied with the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines and principles of the Declaration of Helsinki [9]. Additionally, ethical approval for the study was obtained from the Swedish Ethical Review Authority (ref: 2022-03107-02).
The study included all adult patients 50 years or older who had undergone emergency hip fracture surgery following a traumatic fall and were managed surgically using internal fixation (open reduction internal fixation or intramedullary nailing) or arthroplasty (total hip arthroplasty or hemiarthroplasty). To mitigate heterogeneity in the dataset, patients with head, vascular, or truncal injuries were excluded. Patients missing data were also excluded in order to allow for a complete case analysis. The variables were identified through International Classification of Diseases 10th Revision (ICD-10) codes registered in the NIS [10]. The dataset included patient demographics, clinical characteristics, markers of frailty [Orthopedic Frailty Score (OFS) and weight loss], [11,12,13,14], as well as discharge disposition.
Statistical analysis
In order to provide a concise summary of the study population, patients were divided into those who survived the hospital stay, and those who died in-hospital. Age was presented as a median and interquartile range as it was not normally distributed; differences between the groups were subsequently assessed using the Mann-Whitney U test. Categorical variables were summarized using counts and percentages. Differences between categorical variables were determined using the Chi-squared test or Fisher’s exact test. The primary outcome was in-hospital mortality.
A logistic regression (LR) models was fitted with in-hospital mortality as the response variable [7]. The predictors included age, sex, race/ethnicity, median household income, markers of frailty, type of fracture, type of surgery, comorbidities, and administered medications. The markers of frailty were the OFS and weight loss [11,12,13,14]. Comorbidities included dementia, hypertension without complications, hypertension with complications, ischemic heart disease, angina pectoris, previous myocardial infarction, congestive heart failure, valvular disease, peripheral vascular disorder, diabetes mellitus without complications, diabetes mellitus with complications, chronic kidney disease, cerebrovascular disease, paralysis, other neurological disorder, pulmonary circulation disorder, chronic pulmonary disease, chronic obstructive pulmonary disease, peptic ulcer disease, liver disease, coagulopathy, connective tissue disease including rheumatoid arthritis, connective tissue disease excluding rheumatoid arthritis, chronic blood loss anemia, deficiency anemia, fluid/electrolyte disorder, obesity, osteoporosis, osteoporosis with previous fracture, previous deep vein thrombosis, AIDS, local cancer, leukemia, lymphoma, metastatic cancer, depression, psychosis, current smoker, alcohol abuse, drug abuse. Administered medications included insulin, antithrombotic medications, anticoagulants, and corticosteroids.
Two models were fitted, one including all variables except for the markers of frailty, and another including the markers of frailty. The relative importance of all variables in each model was determined using the permutation importance (PI) method. [15]. The PI was determined by estimating the effect of omitting a specific variable on a predetermined value [1 - Area under the receiver-operating characteristic curve (AUC)]. The PI method masks the information of a variable during evaluation by replacing it with noise from other cases. To account for the uncertainty related to the use of permutations, this process was repeated 10 times for each model. The relative importance of each variable in the model was then presented as the average increase in 1-AUC relative to the AUC in a model including all variables without masking.
As a final step, two new LR models were fitted using the top ten most important variables according to their relative importance. [7]. The AUC for each model was calculated and used to compare the predictive ability of the two models, one with and one without markers of frailty, for each outcome. This was done to determine whether the markers of frailty improved the predictive ability of the models, or whether they served as a replacement for dementia.
Statistical significance was defined as a two-sided p-value <0.05. The analyses were performed using the statistical programming language R (R Foundation for Statistical Computing, Vienna, Austria), with the tidyverse, DALEX, haven, survey, cowplot, pROC, and parallel packages [16].
Results
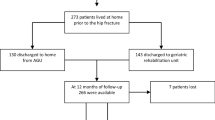
This analysis included an estimated total of 216,395 patients; 1.3% (N = 2,820) died in the hospital. Those that died in the hospital were generally older [86 vs 81 years old, p <0.001] and a larger proportion was male [44.9% vs 30.5%, p <0.001]. There was no significant difference in race/ethnicity and median household income by zip code. Patients who died in the hospital were much more likely to be classified as frail according to their OFS [OFS ≥2: 34.9% vs 13.8%, p <0.001], suffer from unintentional weight loss [16.1% vs 7.6%, p <0.001], and dementia [34.6% vs 25.8%, p <0.001]. Those who died were also less likely to have suffered a cervical hip fracture [37.6% vs 47.4%, p <0.001]; however, there was no difference in the overall use of internal fixation and arthroplasty to manage the fractures. A generally higher comorbidity burden was also observed among patients who died in the hospital (Table 1).
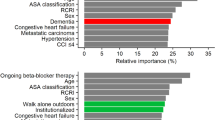
When ranking the relative importance of variables for predicting in-hospital mortality, excluding markers of frailty, dementia was the 7th most important variable. When markers of frailty were included, dementia was replaced in rank by the OFS and weight loss. The top ten most important variables for predicting in-hospital mortality and their relative ranks are presented in Figure 1. There was no significant difference in the predictive ability of the LR models built using the top ten most important variables when comparing those that included [AUC (95% CI): 0.79 (0.77–0.81)] and excluded [AUC (95% CI): 0.79 (0.77–0.80)] markers of frailty. When all 52 variables were used to build the LR models, the predictive ability of the model remained relatively unchanged [AUC (95% CI): 0.81 (0.79–0.83)] (Table 2).
Discussion
In the current analysis, dementia is replaced in predictive importance by the OFS and weight loss when predicting in-hospital mortality. Both of the model excluding and the model including markers of frailty performed at the same level when predicting in-hospital mortality. Dementia consequently appears to function as a surrogate for frailty when predicting in-hospital mortality.
These results are in accordance with a previous investigation utilizing the National Swedish Hip Fracture Register, which studied the role of dementia and frailty in predicting mortality up to 1 year postoperatively in patients with hip fractures. This study incorporated several markers of frailty, including functional status, institutionalization, walking ability, and the use of walking aids. Notably, the results demonstrated that these markers of frailty replaced dementia in terms of predictive importance at all investigated time points. This further indicates that the frailty measured by OFS and weight loss, as well as markers of frailty included in the previous study, adequately capture the concept of frailty. Finally, both the current models and those from the previous investigation, using a large Swedish cohort, for 30-day mortality exhibited an AUC around 0.8, demonstrating a robust predictive capability. Moreover, all models surpassed an AUC threshold of 0.7, signifying that a significant proportion of the important predictors of mortality were captured by the datasets [7, 17].
Given the high mortality rate observed in frail hip fracture patients, [11, 12, 18], and in particular those with dementia, [3], identifying potential avenues for mitigating this adverse outcome is essential. One potential approach is the orthogeriatric care model. This model emphasizes the collaborative efforts between orthopedic surgeons and geriatricians to provide specialized care that addresses the unique medical, cognitive, and functional challenges faced by this population. Studies have consistently demonstrated the advantages of the orthogeriatric care model in terms of improved outcomes and reduced healthcare resource utilization, cost, hospital stay, as well as a reduction in morbidity and mortality [19,20,21,22,23,24]. Another potential intervention worth considering is beta-blocker therapy, which has been proposed as a means to reduce the posttraumatic hyperadrenergic response. [25,26,27,28]. Previous investigations have found an association between preadmission beta-blocker therapy and a reduction in postoperative mortality in hip fracture patients with dementia, a reduction which has also been observed to be larger the more frail a patient was. [29, 30]. Nevertheless, future studies will be required to determine if there is any advantage to the initiation of beta-blocker therapy in hip fracture patients.
This investigation included almost 220,000 estimated patients with hip fractures from the NIS, the largest all-payer inpatient database in the United States, raising both the external and internal validity of the results [8]. By leveraging this dataset, a wide range of potential predictors could be included in the regression models. Furthermore, the study design limited the population to patients with surgically managed hip fractures without significant additional injuries, thus reducing the overall heterogeneity in the study population. However, it is important to acknowledge that the retrospective nature of the study poses certain limitations. Potential predictors that were not captured by the dataset, such as time to surgery, preoperative optimization, admission vitals, and ongoing pharmacotherapies, could not be included in the analysis. The analyses conducted in this study were also confined to the outcomes available within the dataset, thereby precluding assessments of post discharge mortality, functional status, or quality of life. While the analyses validated that dementia serves as a surrogate for frailty when predicting mortality in hip fracture patients, it is important to note that this does not necessarily mean that all patients with dementia are inherently frail. Nevertheless, there remains a significant correlation between dementia and frailty. It should also be emphasized that this study assumes that the OFS and weight loss are markers of frailty, as established by previous research; [11, 14, 18, 30]; however, it should be acknowledge that these variables indicate the presence of frailty rather than encompassing the concept of frailty itself. Finally, we were only able to establish the association between dementia, frailty and mortality for in-hospital mortality, whereas former studies used up to 1-year mortality [7, 11, 18, 30]. Despite the different timepoints for mortality, the results of the current investigation are consistent with previous studies, confirming the robust nature of these results.
Conclusion
Dementia functions as a surrogate for frailty for predicting in-hospital mortality in patients who have undergone hip fracture surgery. This finding highlights the importance of early frailty screening for improvement of care pathways and discussion with patients and their families in regard to expected outcomes.
Conflict of interest
The authors have no conflicts of interest to disclose.
References
NHFD 2019 annual report [Internet]. [Cited 2020 Oct 18]. Available from: https://www.nhfd.co.uk/20/hipfractureR.nsf/docs/2019Report
Gundel O, Thygesen LC, Gögenur I, Ekeloef S. Postoperative mortality after a hip fracture over a 15-year period in Denmark: a national register study. Acta Orthop. 2020;91(1):58–62.
Ioannidis I, Mohammad Ismail A, Forssten MP, Ahl R, Cao Y, Borg T, et al. The mortality burden in patients with hip fractures and dementia. Eur J Trauma Emerg Surg. 2022;48(4):2919–25.
Hou M, Zhang Y, Chen AC, Liu T, Yang H, Zhu X, et al. The effects of dementia on the prognosis and mortality of hip fracture surgery: a systematic review and meta-analysis. Aging Clin Exp Res. 2021;33(12):3161–72.
Bai J, Zhang P, Liang X, Wu Z, Wang J, Liang Y. Association between dementia and mortality in the elderly patients undergoing hip fracture surgery: a meta-analysis. J Orthop Surg Res. 2018;13(1):298.
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23(9):2239–56.
Forssten MP, Ioannidis I, Mohammad Ismail A, Bass GA, Borg T, Cao Y, et al. Dementia is a surrogate for frailty in hip fracture mortality prediction. Eur J Trauma Emerg Surg. 2022;48(5):4157–67.
Agency for healthcare research and quality. HCUP-US Methods Series [Internet]. Healthcare Cost and Utilization Project (HCUP). [Cited 2023 Jan 28]. Available from: https://www.hcup-us.ahrq.gov/reports/methods/methods.jsp
WMA The World Medical Association-WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects [Internet]. [Cited 2020 Sep 21]. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
Tran Z, Hsiue PP, Pan C, Verma A, Rahimtoola R, Stavrakis A, et al. Impact of delayed intervention on clinical outcomes following traumatic hip fracture in the elderly: a national analysis. J Orthop. 2021;14(27):74–8.
Forssten MP, Cao Y, Trivedi DJ, Ekestubbe L, Borg T, Bass GA, et al. Developing and validating a scoring system for measuring frailty in patients with hip fracture: a novel model for predicting short-term postoperative mortality. Trauma Surg Acute Care Open. 2022;7(1): e000962.
Forssten MP, Cao Y, MohammadIsmail A, Ioannidis I, Tennakoon L, Spain DA, et al. Validation of the orthopedic frailty score for measuring frailty in hip fracture patients: a cohort study based on the United States National inpatient sample. Eur J Trauma Emerg Surg. 2023. https://doi.org/10.1007/s00068-023-02308-7.
Agency for Healthcare Research and Quality. Elixhauser Comorbidity Software Refined for ICD-10-CM [Internet]. Healthcare Cost and Utilization Project (HCUP). [Cited 2023 Feb 2]. Available from: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10.jsp
ACG System version 11.0 Technical reference guide [Internet]. Johns Hopkins ACG® System. [Cited 2023 May 14]. Available from: https://www.hopkinsacg.org/document/acg-system-version-11-technical-reference-guide/
Altmann A, Toloşi L, Sander O, Lengauer T. Permutation importance: a corrected feature importance measure. Bioinformatics. 2010;26(10):1340–7.
R Development Core Team. R: a language and environment for statistical computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2008. Available from: http://www.R-project.org/
Hosmer DW Jr, Lemeshow S, Sturdivant RX. Applied logistic regression. New York: John Wiley & Sons; 2013. p. 528.
Forssten MP, Mohammad Ismail A, Ioannidis I, Wretenberg P, Borg T, Cao Y, et al. The mortality burden of frailty in hip fracture patients: a nationwide retrospective study of cause-specific mortality. Eur J Trauma Emerg Surg. 2022. https://doi.org/10.1007/s00068-022-02204-6.
Moyet J, Deschasse G, Marquant B, Mertl P, Bloch F. Which is the optimal orthogeriatric care model to prevent mortality of elderly subjects post hip fractures? A systematic review and meta-analysis based on current clinical practice. Int Orthop. 2019;43(6):1449–54.
Van Heghe A, Mordant G, Dupont J, Dejaeger M, Laurent MR, Gielen E. Effects of orthogeriatric care models on outcomes of hip fracture patients: a systematic review and meta-analysis. Calcif Tissue Int. 2022;110(2):162–84.
Grigoryan KV, Javedan H, Rudolph JL. Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma. 2014;28(3):e49-55.
Leal J, Gray AM, Hawley S, Prieto-Alhambra D, Delmestri A, Arden NK, et al. Cost-effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: a population-based study. J Bone Miner Res. 2017;32(2):203–11.
Ginsberg G, Adunsky A, Rasooly I. A cost-utility analysis of a comprehensive orthogeriatric care for hip fracture patients, compared with standard of care treatment. Hip Int. 2013;23(6):570–5.
Abrahamsen C, Nørgaard B, Draborg E, Nielsen MF. The impact of an orthogeriatric intervention in patients with fragility fractures: a cohort study. BMC Geriatr. 2019;19(1):268.
Moor D, Aggarwal G, Quiney N. Systemic response to surgery. Surgery Oxford Int Ed. 2017;35(4):220–3.
Loftus TJ, Efron PA, Moldawer LL, Mohr AM. β-blockade use for traumatic injuries and immunomodulation: a review of proposed mechanisms and clinical evidence. Shock. 2016;46(4):341–51.
Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85(1):109–17.
Mohseni S, Joseph B, Peden CJ. Mitigating the stress response to improve outcomes for older patients undergoing emergency surgery with the addition of beta-adrenergic blockade. Eur J Trauma Emerg Surg. 2022;48(2):799–810.
Ioannidis I, Mohammad Ismail A, Forssten MP, Cao Y, Bass GA, Borg T, et al. β-Adrenergic blockade in patients with dementia and hip fracture is associated with decreased postoperative mortality. Eur J Trauma Emerg Surg. 2022;48(2):1463–9.
Forssten MP, Mohammad Ismail A, Ioannidis I, Wretenberg P, Borg T, Cao Y, et al. A nationwide analysis on the interaction between frailty and beta-blocker therapy in hip fracture patients. Eur J Trauma Emerg Surg. 2023. https://doi.org/10.1007/s00068-023-02219-7.
Funding
Open access funding provided by Örebro University. No financial support or funding was received for the presented work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ioannidis, I., Forssten, M.P., Mohammad Ismail, A. et al. The relationship and predictive value of dementia and frailty for mortality in patients with surgically managed hip fractures. Eur J Trauma Emerg Surg 50, 339–345 (2024). https://doi.org/10.1007/s00068-023-02356-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02356-z