Abstract
Purpose
To evaluate whether the 24-weeks postoperative fracture union rate for the investigational TFNA intramedullary nail was non-inferior compared to the control product PFNA-II.
Methods
The study was a prospective, randomized, single-blind, noninferiority dual-arm study drawing from 9 trauma centers across China, between November 2018 and September 2020, with follow-up measurements at 24 weeks after internal fixation. The full analysis data set (FAS [Intent-to-Treat]) was analyzed and is summarized here. The primary outcome was fracture union rate, a composite score combining clinical and radiographic assessment. Secondary endpoints comprised (a) clinical outcomes including (1) SF-12, (2) Harris Hip, and (3) EQ-5D Scores, (b) radiographic incidence of complications such as loosening or cut-out requiring revision, (c) revision rates, (d) reoperation rates, and (e) adverse events, including 24-weeks revision and reoperation rates.
Results
Both TFNA and PFNA-II group fracture healing rates were 100% at 24 weeks; TFNA was therefore shown to be non-inferior to PFNA-II. With baseline data matched in all parameters except age in both the TFNA and PFNA-II groups, comparisons of union rates, SF-12, Harris Hip, and EQ-5D Scores yielded p values > 0.05 indicating no significant difference between the two groups, further supporting the noninferiority of TFNA. In both groups, revision and re-operation rates were 0, and the incidences of serious adverse events were 19.4% and 17.4%, respectively.
Conclusion
In terms of fracture union rate at 24 weeks, the DePuy Synthes Trochanteric Fixation Nail Advanced (TFNA) was not inferior to the marketed Proximal Femoral Nail Antirotation (PFNA-II) device produced by the same manufacturer. Secondary and safety outcomes showed no significant differences between the two groups.
Registration
Registration was completed at ClinicalTrials.gov NCT03635320.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several types of cephalomedullary nails are commercially available. The Proximal Femoral Nailing Antirotation (PFNA; DePuy Synthes, Oberdorf, Switzerland) manufactured from a titanium alloy (Ti-6Al-7Nb) is an advanced version of the previous PFN nail featuring an anti-rotation helical blade and currently available for clinical use in China. The PFNA-II, also available in China, is a smaller version of the PFNA designed for the reduced femur size of typical Asian populations [1].
The TFN-AdvancedTM Proximal Femoral Nailing System (TFNA, DePuy Synthes, Oberdorf, Switzerland) was introduced in 2015 with a number of updated design features: (a) a reduced proximal nail diameter, (b) a reduced radius of curvature, (c) an oblique cut of the lateral end of the helical blade or screw, (d) provision of a higher strength titanium alloy T-15Mo (TiMo), (e) the introduction of static, dynamic or oblique locking options, and (f) a variety of features to increase procedural efficiency. These design features were intended to address unmet needs, offering the possibilities of (a) reducing cut-out by facilitating the compaction of cancellous bone surrounding the implant [2], (b) reducing anterior impingement, (c) preventing lateral protrusion, (d) reducing nail breakage, (e) preventing distal impingement (due to curvature misalignment), and (f) facilitating surgical procedures with the possibility of abbreviating operating time.
The PFNA-II was selected as the comparator device for this study. The PFNA-II is an appropriate reference product for the TFNA, as its intended use as well as clinical, technical, and biological parameters are similar. The intended uses of PFNA-II and TFNA are the treatment of proximal femur fractures and combination proximal and shaft fractures of the femur.
This study was undertaken to collect pre-market data on TFNA to support a marketing application in China. The goal was to compare the effectiveness and safety of the TFNA system with the commercially available PFNA-II for the treatment of proximal femoral trochanteric fractures. The primary objective was to evaluate fracture union at 24 weeks postoperatively with secondary measures pertaining to the quality of life and safety. In terms of convenience and presumed time and cost savings, the noninferiority trial was designed according to specific, established protocols [3, 4] in recognition that its use has increased in recent years [5, 6]. The assumption was that matching outcomes of the TFNA and PFNA-II products, using the latter as a standard of care, represented a desirable demonstration of noninferiority.
Methods
Study design
One hundred eighty-eight participants were enrolled, beginning November 2018 and concluding September 2019 across nine sites in China. The last patient visit occurred May 2020, and the database was locked September 2020. The ethics committees approved the protocol and informed consent at each participating site. The study was registered on ClinicalTrials.gov (identifier: NCT03635320). Eligible men and women were aged 18 years or older and had sustained a unilateral proximal femur fracture (AO 31-A1, 31-A2, 31-A3), or trochanteric fracture with diaphyseal extension. Key exclusion criteria included fractures where the operative treatment occurred 3 weeks after surgery, femoral head and neck fractures (AO 31-B and 31-C), pathologic fracture, revision surgeries, serious soft tissue injury, and multiple systemic injuries. The complete list of inclusion and exclusion criteria is found in Table 1. All patients were followed for 6 months after time of surgery.
Patients enrolled at each study site were informed in advance that they would be randomized in a 1:1 ratio to either the investigational group (TFNA) or the control group (PFNA-II) using a separate block group randomized schedule at each study site, ensuring the consistent distribution of patients in the treatment group and control group. Eligible patients were randomly assigned to the TFNA, or PFNA-II study group using a centralized computer-generated randomization system (Medidata Balance, Dassault Systèmes, Shanghai). Patients were blinded to the treatment they had received until study completion; study personnel were not blinded. Patients and investigators were unaware of block sizes.
The study’s null and alternative hypotheses were as follows:
where PPFNA-II represents the fracture union rate among those receiving the PFNA-II implant, PTFNA represents the fracture union rate among those receiving the TFNA implant, and 10% is the pre-specified non-inferiority margin [7].
Radiographic assessments
Radiographic film review was conducted by two independent reviewers with a third reviewer involved to resolve discrepancies and render a final decision. At the preoperative visit, the investigator documented the fracture type according to the AO classification system [8]. Based on postoperative x-rays, the independent radiologist determined whether there was radiographic evidence of a secondary surgical procedure (for example, head element removal). The radiologist also provided assessment of the implant status and whether the device was in good condition or if any mechanical complications had occurred, including the qualitative assessment of the fracture line and callus.
Sample size
In order to achieve 80% power for a non-inferiority evaluation, the assumption was that there was no difference between the fracture union rate of the two groups; anticipated fracture union rates were assumed to be 95%, and the non-inferiority margin was 10% by using the one-sided significance level of 0.025 [9]. One hundred fifty patients (75 in each group) were required for analysis. Considering a 20% drop-out caused by unexpected circumstances (patient deaths, withdrawals from the study, loss to follow-up) and further strengthening the safety evaluation of the study, 188 patients (94 patients in each group) were targeted for enrollment.
Surgical procedure
Surgeons recruited in the study had previous experience with cephalomedullary nailing. The surgical procedure was a closed reduction (and/or open reduction if needed) under fluoroscopy. The implantation of both nail systems is similar involving opening of the medullary cavity, insertion of the nails and head assembly, distal locking, and insertion of the end cap (if desired). While the TFNA is available with both screw and blade head elements, the PFNA II is only available with a helical blade head element.
Primary endpoint
The primary endpoint was fracture union at 24 weeks postoperatively. Successful fracture union was a composite end point. For individual patients, the treatment was considered successful if all of the following conditions were met 24 weeks after surgery: (a) no focal tenderness or lengthwise percussion pain, or abnormal movement; (b) the frontal/lateral X-ray examination showed vague or no fracture gap, or continuous callus passing across the fracture line; and (c) no deformation or breakage was found in the implants. Representative case examples of AO/OTA 31A1-3 fractures with uneventful healing with PFNA-II or TFNA are shown in Fig. 2.
Secondary endpoints
Secondary endpoints included (a) clinical outcomes: SF-12, Harris Hip Score, and EQ-5D, (b) adverse events (type and frequency) compared between investigational and control groups, (c) 24-weeks revision rate (removal of any component for any reason), and (d) 24-weeks reoperation rate (secondary surgery at the fracture site[s] performed for any reason). In addition, assessments were collected on the surgeon’s evaluation of product operability during the index procedure.
SF-12 scores were summarized for both treatment groups at baseline, and at the 12- and 24-weeks follow-up visits. In addition, SF-12 scores were summarized for change from baseline. An ANCOVA model was used with the change from baseline as the outcome variable. The treatment group was an independent variable, and the baseline value was the concomitant variable. The Harris Hip Score was only collected at the 12- and 24-weeks follow-up visits. The 12- and 24-weeks scores were summarized and compared between groups using the t test. Qualitative outcomes were compared between groups using either a Chi-square test or Fisher’s exact probability test. The EQ-5D Health Index (HI) was based upon Japanese population coefficients.
Safety
In this study, adverse events (AEs) were defined as any untoward medical occurrence, unintended disease or injury, or untoward clinical signs (including abnormal laboratory findings) in patient, users, or other persons, whether or not related to the investigational medical device. Serious adverse events (SAEs) were defined as any AE that (a) led to death; (b) led to serious deterioration in the health of the patient that either resulted in (1) a life-threatening illness or injury, or (2) a permanent impairment of a body structure or a body function, or (3) in-patient or prolonged hospitalization, or (4) medical or surgical intervention to prevent life-threatening illness or injury or permanent impairment to a body structure or body function; (c) led to fetal distress, fetal death or a congenital abnormality or birth defect. At each evaluation of the patient enrolled in the clinical investigation, the investigator determined whether any AE or SAE occurred and determined its possible relationship to the study devices or procedure. Adverse events were coded and summarized by MedDRA system organ class (SOC) and preferred term (PT). Causal relationships of AEs to the device were rated as unrelated, unlikely, possible, probable, or related. Adverse events were collected regardless of the relationship to the procedure or the device.
Baseline variables
Baseline variables were ascertained after randomization with self-reported questionnaires and with a physical examination performed by a trained research assistant.
Statistical analysis
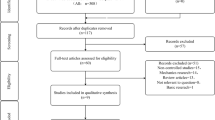
The analysis populations consisted of a full analysis set (FAS) in which the data set constituted all patients who were consented and received an implant, and a Per Protocol Set (PPS), which comprised a set of patients that completed the trial but excluded those with a serious protocol violation affecting the primary efficacy endpoint (Fig. 1). The results from the FAS are presented, as utilization of the FAS is appropriate for all of the outcome comparisons evaluated here.
Patient demographics and baseline variables were provided for the FAS population. Descriptive statistics for continuous variables included the number of patients, mean, and standard deviation. Descriptive statistics for dichotomous/categorical variables included number and percent of patients. A two-sided alpha of 0.05 was used for statistical testing and confidence intervals unless otherwise noted.
For calculating the confidence interval when both treatment and control groups were binomial extremes (0% and 100%, fractured and resolved), the Newcombe–Wilson method was applied [10].
Results
Eligibility
One hundred ninety-two patients were screened, and 188 patients were included and randomly assigned to a group; enrolment included 94 in the investigational group and 94 in the control group. Three patients were not implanted with a device, resulting in 185 patients in the FAS. Accounting for drop-outs, there were 164 patients in the PPS, including 81 in the TFNA group and 83 in the PFNA-II group. Reasons for exclusion prior to final assignments to the FAS and PPS groups are shown in Fig. 1. With all outcomes closely matched between the PPS and FAS populations, the FAS data are presented for the remainder of the report.
Baseline condition
There were no significant baseline differences in demographic data or fracture characteristics except age (p=0.0274) of patients between the study group and the control group. There were no crossovers (patients assigned to one group who received a device from the other). For the TFNA group, the average age was 77.8 ± 10.80 including 29 males and 64 females, while for the PFNA-II group, the average age was 74.1 ± 11.80 including 33 males and 59 females. Statistical differences regarding gender, and BMI were not significant (Table 2).
Surgery and fracture details
All fractures were closed, and the reason for fracture was low energy in 96.8% of cases for TFNA and 94.6% of cases for PFNA-II. Most fractures in both groups were either 31-A1 or 31-A2 (Table 2). Closed reduction was used for all fractures in the TFNA group and for all but one fracture in the PFNA-II group. Reaming was used in 5 (5.4%) cases in the TFNA group and in 9 (9.8%) cases in the PFNA-II group (Table 3); this difference was not significant (p=0.254). The difference in intraoperative blood loss between the study (131.0 mL ± 97.4 mL) and control (130.9 mL ± 126.3 mL) groups was insignificant (p=0.9953), as was surgery time (1.22 h ± 0.49 hr and 1.08 h ± 0.56 h) for the respective groups (p=0.0610) (Table 3).
Regarding the ease of operability of the two nail systems, there were no significant differences in the difficulties of determining nail position, nail insertion, proximal or distal locking, or placement of end caps. In addition, the impact of nail placement on maintenance of the reduction and surgeon satisfaction with the instruments available in the sets did not show a significant difference between groups (Table 3).
As discussed above, the TFNA is available with both screw and blade head elements, and the PFNA II is only available with a helical blade head element. With regard to the proximal head element, 80 patients received blades and 13 patients received screw head elements in the TFNA group. All patients in the PFNA-II group received helical blade head elements, since that was the only available head element type for that implant.
Primary endpoint
The primary endpoint was fracture union at 24 weeks postoperatively. In the FAS, there were a total of 93 patients in the TFNA group, of which 11 (11.8%) did not have an assessment for the measurement of fracture union at 24 weeks after surgery; there were a total of 92 patients in the PFNA-II group, of which 7 (7.6%) did not have an assessment for the measurement of fracture union at 24 weeks after surgery.
Based on analysis of the actual data collected from patients (non-missing data), all 82 patients in the TFNA group had fracture union, and all 85 patients in the PFNA-II group had fracture union, resulting in a fracture union rate of 100% at 24 weeks after surgery in both groups. When the Newcombe–Wilson scoring method was used, the fracture union rate difference between the TFNA group and the PFNA-II group was 0. The two-sided 95% CI [− 4.48%; 4.32%] was within the 10% threshold of non-inferiority, indicating that the TFNA group was not inferior to the PFNA-II group.
Examples of each of the fracture classes and implantations of the TFNA and PFNA-II devices with comparable union are shown in Fig. 2.
Secondary endpoints
Results from the Harris Hip Score, SF-12 (physical and mental components), and EQ-5D Health Index score are summarized in Table 4. There was a slight variation in sample size for each assessment due to missing data for some outcomes. The p-values represent a comparison of study vs. control groups, with some comparisons being the change from baseline, where indicated.
Harris Hip Score results for the 83 patients in the TFNA group with data showed a mean (SD) score at 12 weeks after surgery of 77.71±10.94 and a mean score for the 85 patients in the PFNA-II group at 12 weeks after surgery of 80.62±11.06. A Group t test was adopted for comparison of the TFNA and PFNA-II groups; the p value was 0.0882, indicating no statistically significant difference. The mean Harris Hip Score for the 82 patients in the TFNA group with data at 24 weeks after surgery was 86.03±10.42, and for the 85 patients in the PFNA-II group was 86.47±11.24. The p value was 0.7938, indicating no statistically significant difference. The score for both groups improved between 12 and 24 weeks (Table 4).
SF-12 total physical score results for the 84 patients in the TFNA group with data showed a mean (SD) total physical score at 12 weeks after surgery of 37.59±6.62; the mean total physical health score of the 84 patients in the PFNA-II group was 38.69±6.71. The p value was 0.2948, indicating no statistical significance between the two groups. At 12 weeks after surgery, the total mental health score of the 84 patients in the TFNA group with data was 54.93±9.82; the total mental health score of the 84 patients in the PFNA-II group was 55.10±9.64. The p value was 0.6672, indicating no statistical significance between the two groups.
At 24 weeks after surgery, the mean total physical health score of the 81 patients in the TFNA group with data was 41.41±7.66; the mean total physical health score of the 84 patients in the PFNA-II group was 41.20±6.93. The p value was 0.8110, indicating no statistical significance between the two groups. At 24 weeks after surgery, the total mental health score of the 81 patients in the TFNA group with data was 56.00±9.26; the total mental health score of the 84 patients in the PFNA-II group was 55.09±9.90. The p value was 0.6032, indicating no statistical significance between the two groups.
EQ-5D Health Index scores are also summarized in Table 4. At 12 weeks after surgery, the mean (SD) change in health index of 84 patients in the TFNA group with data was 0.63±0.16; the change of health index of 84 patients in the PFNA-II group was 0.66±0.13. The p value was 0.1817, indicating no statistical significance between the two groups. At 24 weeks after surgery, the mean (SD) change in health index of 81 patients in the TFNA group with data was 0.73±0.17; the change in health index of 84 patient in the PFNA-II group was 0.72±0.15. The p value was 0.5865 indicating no statistical significance between the two groups.
Safety
There were no revisions (component removal for any reason) or re-operations (secondary reoperation of the fractures site for any reason) during the post-operative period at 24 weeks in either study cohort. Adverse events were collected regardless of relationship to the device or procedure. A total of 22 serious adverse events occurred in 18 patients (19.4%) in the TFNA group, and a total of 21 serious adverse events occurred in 16 patients (17.4%) in the PFNA-II group. When classified according to relationship, there were no SAEs related to the device in either group. The SAE rate difference between the two groups was 1.96% (p=0.7302) (Table 5). In the TFNA group, there was one SAE assessed as unlikely to be related to the procedure and one SAE assessed as possibly related to the procedure. In the PFNA-II group, there was one SAE assessed as unlikely to be related to the procedure (Table 6). Regarding severity of SAEs, among the 18 patients in the TFNA group, five were mild, (27.8%), eight were moderate (44.4%), and five were severe (27.8%). Among the 16 patients in the PFNA-II group, 3 were mild (18.8%), 7 were moderate (43.8%), and 6 were severe (37.5%) (Table 6).
One patient had a TFNA helical blade cut-out 63 days after implant due to a fall, reported as an SAE with causation related to the fall and not the device. The investigator had suggested a revision, but the patient refused, and surgery was not performed. There were no revisions or reoperations in either group.
Discussion
In terms of the primary outcome, it was found that the healing rate based on the collected patient data (non-missing data) was 100% in both the TFNA group and the PFNA-II group. We believe that our high degree of fracture union was at least partly attributable to the stringent exclusion criteria shown in Table 1, which was designed to reduce cofounding factors.
Regarding secondary outcomes, information was collected for the revision and reoperation rates at 24 weeks after surgery, as well as the SF-12, Harris Hip, and EQ-5D Scores. There were not revisions or reoperations in either group. Clinical outcome scores were statistically indistinguishable, indicating no signification differences between either implant. In addition to these clinical outcomes, the apparent equivalence of surgical markers such as blood loss and surgery time supported the non-inferiority of the TFNA compared to the PFNA-II.
During the study, all intra- and post-operative AEs were recorded and evaluated for relationship to the device or procedure. With a total of 18 and 16 SAEs occurring in the TFNA and PFNA-II groups, respectively, it was shown that the safety profile of TFNA demonstrated no significant difference from the PFNA-II. No device-related adverse events were identified in the clinical study.
Regarding the operability of both the TFNA and PFNA-II devices, surgeons’ assessments of the two products across various stages of handling were found to be virtually identical. Because differences in healing rates and Harris scores and safety between blades and screws were found to be insignificant, the selection of blades or screws depended upon the preference of surgeons. The static locking option was not collected because the surgeons only used that option when the AO classification of the fracture was A3 or if there were other unstable fractures, less than 10% of the patients studied (Table 2). While not statistically significant, possible improvement was observed in the TFNA group with regard to the parameters including “determine nail application position,” “inserting the nail,” “proximal locking,” “distal locking,” and “placing end cap.” This evaluation provided substantial support for the ability of surgeons familiar with the PFNA-II system to adapt to the TFNA device. While not statistically significant, it also suggested a potential enhancement of the surgical experience, presumably due to the new design features introduced by the TFNA implant and instrumentation. With results from both the PPS and FAS analyses demonstrating non-inferiority, the FAS results were considered to be a sufficient representation of the apparent equivalence of the two nailing systems.
The average age of our patients was 77.8 years for the TFNA group and 74.1 years for the PFNA-II group, in excellent agreement with the average age of 77.1 of the 190,560 patients confirmed as having various classes of hip fracture obtained from the Urban Employee Basic Medical Insurance and Urban Resident Basic Medical Insurance databases, covering over 95% of the whole urban population of China [11]. Our follow-up period of 6 months was in agreement with the time span reported in other studies of the PFNA system (1,5), limiting number of drop-outs that could have occurred over a longer follow-up.
In agreement with our findings, Yoon et al. reported an excellent outcome for the TFNA concerning safety and the surgical treatment of proximal femur fractures in Korea. Specifically, 100% bone union was observed with no early postoperative complications, no implant failures, and no cases of revision surgery [12]. Matsumura et al. found that internal fixation using the TFNA and PFNA-II devices of similar size for Japanese patients with trochanteric hip fractures (even those with unstable conditions) resulted in a union rate of 98% with minimal blood loss and no cases of nail jamming [13]. Unsay et al. reported that early experience in India with the TFNA demonstrated that all fractures healed uneventfully with no distal anterior cortical impingement or perforation; this descriptive study suggested that this cephalomedullary nail was at least comparable to preceding proximal femur nail devices in terms of fixation [14].
Compared to outcome measures of the PFNA-II, PFNA, InterTAN, and Gamma intramedullary nails, the performance of the TFNA in several parameters appears to be equivalent to several values reported in the literature. Table 7 demonstrates a close matching of Harris Hip Scores, the physical and mental components of the SF-12 questionnaire, and revision surgeries and reoperations across all products. In these aspects, our experimental data have shown that the TFNA device is expected not to show significant differences from other cephalomedullary nails in the market place.
The absence of implant breakages in our findings may be related to the paucity of type A3 fractures included in our study groups. In contrast with our prospective study, Lambers et al. [15] reported 16 cases of TFNA nail breakage over a timeline of two years in their retrospective study. In the Lambers study, the initial fracture pattern in 75% of the cases was found to be reverse oblique fractures—precisely the kind that are challenging to reduce, such that the healing process can be delayed. This possibility was supported by the finding in a retrospective study of 176 Asian patients in which individuals with a type A3 fracture were 2.9 times more likely to experience a fracture fixation complication than patients with an A2 fracture. In just a third of the incidents attributable to the fracture class, the complication relation to the implant device itself was deemed to be possible rather than probable or definite [16]. Finally, in Lambers et al., the total number of TFNAs implanted in the three trauma hospitals utilized was not indicated; therefore, an incidence rate could not be determined. No breakage in cases of simple pertrochanteric fracture patterns was seen [15].
Further support regarding the safety of the TFNA device was obtained through a study of retrieved data from a large US healthcare database containing inpatient discharges from geographically diverse hospitals in both urban and rural areas. Since 2012, the database has received contributions of data from over 700 hospitals. The study compared data from the TFNA to a comparison group, which included the Stryker Gamma3 and Zimmer Natural Nail (non-TFNA group). During the study period, implantations with 14,370 TFNA nails were identified and compared with implantations of 8260 non-TFNA nails. When the risk data were balanced, the risk of breakage in 18 months was equivalent in subgroup analyses involving pertrochanteric factures or subtrochanteric fractures [17].
This was the first randomized controlled trial demonstrating the noninferiority of fracture union rates for the TFNA system to an established device in China. The noninferiority approach to benchmarking offers an immediate comparison of implanted devices using a reference standard, featuring advantages compared to standard Kaplan–Meier analyses [18]. The possibility that there was a bias toward the null was unlikely due to the minimal numbers of missing data. The inclusion of both the FAS (intention-to-treat) and PPS (per protocol) analyses (latter data not shown) and the fact that their results were virtually identical avoids pitfalls associated with each method alone [19] and provides additional rigor to our conclusion that the TFNA device was not inferior [19, 20]. Furthermore, our comparison of outcomes of the TFNA against what could be deemed as a standard of care with the PFNA-II product is yet another measure to reduce the risk of bias [6]. Reporting of both the absolute and relative effect measures could be considered to be yet another strength of the study, based on the criteria for equivalence reported elsewhere [21]. Finally, the importance of demonstrating both statistical and clinical equivalence to validate a noninferiority has been described in the literature [22] and is included in our data.
Limitations
The drawing from 9 major trauma centers involving multiple surgeons in a broad range of clinical settings suggests a greater external validity (generalizability) than more confined clinical trials, yet our investigation was designed to address regional regulatory requirements and therefore was restricted to an Asian population in a single country. In our study, 96% of the TFNAs and 98% of the PFNA II products were short nails, respectively. Although studies have compared the outcomes of short versus long nails applied to intertrochanteric femur fractures, results have shown no statistically significant difference in facture union23 as well as insignificant differences in reoperations or complication rates [23,24,25]. Our study group was relatively small, and the follow-up time of 24 weeks was limited, although the nearly identical outcomes in both experimental groups bode well for the study’s validity. Furthermore, the types of lesions studied were restricted with the exclusion of osteoporotic and combination bone fractures (indications for the TFNA), although our extended list of exclusions allowed our study group to be more homogenous with more clearcut classifications of bone fractures—a welcoming feature for more rigorous randomized clinical trials.
Conclusions
In a randomized, blinded, and controlled noninferiority clinical trial, we have found that there was no significant difference in the safety and performance outcomes between the TFNA and PFNA-II devices investigated in this study. It can therefore be concluded that the TFNA is as efficacious and safe as the PFNA-II product to treat fractures of the proximal femur and femoral shaft.
Data availability
The data that support the findings of this study are available from Johnson & Johnson Medical (Shanghai) Ltd., but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Johnson & Johnson Medical (Shanghai) Ltd.
Abbreviations
- AE:
-
Adverse event
- AO:
-
Arbeitsgemeinschaft fur Osteosynthesefragen
- CI:
-
Confidence interval
- EQ-5D:
-
EuroQuol Quality of Life Index
- FAS:
-
Full analysis set
- HI:
-
Health Index
- Hr:
-
Hour
- mL:
-
Milliliter
- OTA:
-
Orthopedic Trauma Association
- PFNA-II:
-
Proximal Femoral Nailing Antirotation
- PPS:
-
Per Protocol Set
- PT:
-
Preferred term
- SAE:
-
Serious adverse event
- SD:
-
Standard deviation
- SF:
-
Short form
- SOC:
-
System organ class
- TFNA:
-
Trochanteric Fixation Nail Advanced
- Ti-6 l-7Nb:
-
Titanium-Aluminum-Niobium
- TiMo:
-
Titanium-Molybdenum
References
Loo W, Loh S, Lee H. Review of Proximal Nail Antirotation (PFNA) and PFNA-2–our local experience. Malaysian Orthop J. 2011;5:1–5.
Windolf M, Muths R, Braunstein V, Gueorguiev B, Hanni M, Schwieger K. Quantification of cancellous bone-compaction due to DHS Blade insertion and influence upon cut-out resistance. Clin Biomech (Bristol, Avon). 2009;24:53–8.
Gøtzsche PC. Lessons from and cautions about noninferiority and equivalence randomized trials. JAMA. 2006;295:1172–4.
Tunes da Silva G, Logan BR, Klein JP. Methods for equivalence and noninferiority testing. Biol Blood Marrow Transplant. 2009;15:120–7.
Suda KJ, Hurley AM, McKibbin T, Motl Moroney SE. Publication of noninferiority clinical trials: changes over a 20-year interval. Pharmacotherapy. 2011;31:833–9.
Bikdeli B, Welsh JW, Akram Y, Punnanithinont N, Lee I, Desai NR, et al. Noninferiority designed cardiovascular trials in highest-impact journals. Circulation. 2019;140:379–89.
Snapinn SM. Noninferiority trials. Curr Control Trials Cardiovasc Med. 2000;1:19–21.
Raaymakers F, Schatzker H, Hensen M, Pesantez RF. AO surgery reference. 2nd ed. AO; 2010.
Wellek S. Testing statistical hypotheses of equivalence and noninferiority. 2nd ed. London: Chapman & Hall/CRC; 2010.
Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17:857–72.
Zhang C, Feng J, Wang S, Gao P, Xu L, Zhu J, et al. Incidence of and trends in hip fracture among adults in urban China: a nationwide retrospective cohort study. PLoS Med. 2020;17: e1003180.
Yoon JY, Kim JW. Treatment of proximal femur fracture with a newly designed nail: trochanteric fixation nail-advanced (TFNA). J Korean Fract Soc. 2020;33:189–95.
Matsumura T, Takahashi T, Nakashima M, Nibe Y, Takeshita K. Clinical outcome of mid-length proximal femoral nail for patients with trochanteric hip fractures: preliminary investigation in a Japanese cohort of patients more than 70 years old. Geriatr Orthop Surg Rehabil. 2020;11:1–7.
Unsay JDC, Huat ICT, Kee EKB. Early experience with the trochanteric fixation nail-advanced (TFN-A): a descriptive review of thirty-four cases from a single center. Indian J Orthop. 2020;54:246–53.
Lambers A, Rieger B, Kop A, D’Alessandro P, Yates P. Implant fracture analysis of the TFNA Proximal Femoral Nail. J Bone Joint Surg Am. 2019;101:804–11.
Sawaguchi T, Sakagoshi D, Shima Y, Ito T, Goldhahn S. Do design adaptations of a trochanteric nail make sense for Asian patients? Results of a multicenter study of the PFNA-II in Japan. Injury. 2014;45:1624–31.
Wallace A, Amis J, Cafri G, Coplan P, Wood J. Comparative safety of the TFN-ADVANCED Proximal Femoral Nailing System: findings from a U.S. Health-Care Database. J Bone Joint Surg Am. 2021;103(17):1637–45.
Deere KC, Whitehouse MR, Porter M, Blom AW, Sayers A. Assessing the non-inferiority of prosthesis constructs used in hip replacement using data from the National Joint Registry of England, Wales, Northern Ireland and the Isle of Man: a benchmarking study. BMJ Open. 2019;9: e026685.
Christensen E. Methodology of superiority vs. equivalence trials and non-inferiority trials. J Hepatol. 2007;46:947–54.
Committee for Proprietary Medicinal Products. Points to consider on switching between superiority and non-inferiority. Br J Clin Pharmacol. 2001;52:223–8.
Assessment of the Safety, Efficacy of a New Thrombolytic Investigators, Van De Werf F, Adgey J, Ardissino D, Armstrong PW, et al. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double- blind randomised trial. Lancet. 1999;354:716–22.
Ganju J, Rom D. Non-inferiority versus superiority drug claims: the (not so) subtle distinction. Trials. 2017;18:278.
Dunn J, Kusnezov N, Bader J, Waterman BR, Orr J, Belmont PJ. Long versus short cephalomedullary nail for trochanteric femur fractures (OTA 31–A1, A2 and A3): a systematic review. J Orthop Traumatol. 2016;17:361–7.
Zhang Y, Zhang S, Wang S, Zhang H, Zhang W, Liu P, et al. Long and short intramedullary nails for fixation of intertrochanteric femur fractures (OTA 31–A1, A2 and A3): a systematic review and meta-analysis. Orthop Traumatol Surg Res. 2017;103:685–90.
Shannon SF, Yuan BJ, Cross WW, Barlow JD, Torchia ME, Holte PK, Sens SA. Short versus long cephalomedullary nails for pertrochanteric hip fractures: a randomized prospective study. J Orthop Trauma. 2019;33(10):480–6.
Acknowledgements
The authors wish to acknowledge the services of the radiologists Zhenghan Yang, Qing He, and Xinmeng Hou, the statisticians Kai Zou and Yun Chen, and the JJMS clinical research team members Jie Zhou, Dandan Ding, Yinni Zhang, and Huimin Dai.
Funding
This research was supported by Johnson & Johnson Medical (Shanghai) Ltd (Grant DPS-201502).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we except for employees of Johnson&Johnson do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Ethical approval
The study was approved on 11th April, 2016 in the leading site, and it was also approved in all other sites.
Informed consent
All subjects have agreed to join the study and they have signed on the informed consent.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, L., Pan, Z., Zheng, X. et al. Prospective randomized multicenter noninferiority clinical trial evaluating the use of TFN-advancedTM proximal femoral nailing system (TFNA) for the treatment of proximal femur fracture in a Chinese population. Eur J Trauma Emerg Surg 49, 1561–1575 (2023). https://doi.org/10.1007/s00068-023-02231-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02231-x