Abstract
Purpose
Thoracic trauma accounts for 25–50% of posttraumatic mortality. Data on epidemiology of thoracic trauma in Scandinavia and risk factors for mortality are scarce. This study aims to provide an overview of epidemiology, clinical events and risk factors for mortality of patients with severe thoracic injuries.
Methods
A retrospective study including adult thoracic trauma patients with abbreviated injury scale ≥ 3, between 2009 and 2018 at Haukeland University Hospital was performed. Subgroup analyses were performed for specific patient groups: (1) isolated thoracic trauma, (2) polytrauma without Traumatic Brain Injury (TBI) and (3) polytrauma with TBI. Logistic regression analyses were applied to find risk factors for 30-days mortality. Age, sex, comorbidity polypharmacy score (CPS), trauma and injury severity score (TRISS) and comprehensive complication index (CI) were included in the final model.
Results
Data of 514 patients were analyzed, of which 60 (12%) patients died. Median (IQR) injury severity score (ISS) was 17 (13–27). Data of 463 patients, of which 39 patients died (8%), were included in multivariate analyses. Female sex odds ratio (OR) (2.7, p = 0.04), CPS > 9 (OR 4.8; p = 0.01), TRISS ≤ 50% (OR 44; p < 0.001) and CI ≥ 30 (OR 12.5, p < 0.001) were significant risk factors for mortality. Subgroup analyses did not demonstrate other risk factors.
Conclusion
Comorbidities and associated pharmacotherapies, TRISS, female sex, and complications during admission predict in-hospital mortality after thoracic trauma. Current findings might help to recognize patients at risk of an adverse outcome, and thereby prevent complications.
Trial registration: retrospectively registered
The regional committees for medical and health research ethics file number is 2017/293.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The thorax is a body region that is frequently and severely injured. Around two thirds of patients with multiple injuries have severe thoracic injury abbreviated injury scale (AIS) ≥ 3 [1]. Mortality after trauma can be as high as 30% in patients with severe thoracic injury [2]. Although frequency and mortality are high, epidemiological studies are limited in the Nordic countries and without recent update, especially when evaluating risk factors for mortality following thoracic trauma.
When treating patients with multiple injuries, the evaluation of severity of thoracic trauma influences decision making in terms of first treatment and further clinical course [3]. Although there is plenty of literature on risk factors for mortality after trauma in general, little has been published on thoracic trauma specifically. Most thoracic trauma studies are analyses from trauma registries without supplementation from patient files, which makes the analysis of all relevant comorbidities and complications challenging [4,5,6].
One of the risk factors influencing mortality is injury severity, which is difficult to estimate due to a wide variety of scoring systems [7]. The scoring systems combining anatomical and physiological parameters seem to be the most suitable for severity assessment [7]. Next to injury severity, several other risk factors are thought to influence the clinical course of patients with thoracic trauma, such as age, sex, anticoagulant use, comorbidities and complications. An increase in the number of elderly patients with multiple trauma has been observed over the last years [8]. Hence it has been established that an age of 65 years and older is a predictive factor for mortality in patients with thoracic trauma [9, 10]. This is mainly due to diminished physiological reserves, inferior pre-injury functional capacities and age-related comorbidities [11].
Comorbidities influence mortality in thoracic trauma patients with odds ratios (OR) reported ranging from 1.2 in peripheral artery disease to as high as 6.6 in patients with metastatic cancer [5, 12, 13]. A systematic review about the influence of comorbidities on mortality is however lacking, and scoring systems of comorbidities have mostly been avoided.
Finally, complications may significantly alter the clinical course of thoracic trauma patients. Common complications as pneumonia and adult respiratory distress syndrome, are known causes of mortality following thoracic trauma [14]. There is limited literature on posttraumatic complications and mortality interaction in thoracic trauma. Additionally, to the best of our knowledge, no standardized scoring system for complications in thoracic trauma have been used yet. It has been shown that different injury mechanisms lead to different injury patterns [15]. Isolated thoracic injury, polytrauma with Injury Severity Score (ISS) ≥ 16 without Traumatic Brain Injury (TBI) and polytrauma with TBI as specific patient groups have differences in injury characteristics and could therefore theoretically demonstrate different predictive factors for mortality [16]. Therefore the aim of this study was to describe epidemiology and predictive factors for mortality following severe thoracic trauma in general and in relevant patient groups.
Methods
Study design
A retrospective study was performed on patients admitted to Haukeland University Hospital (HUS), a level one trauma center, between January 2009 and December 2018. Until December 2014, the patients were registered in the local hospital trauma registry and after that, in the Norwegian National Trauma Registry (NTR) [17]. The project was approved by the Regional Medical Ethics Committee in Norway under registration number 2017/293-8 [18]. Inclusion criteria were thoracic trauma with an AIS chest score of ≥ 3 and an age of 18 years or older at the day of the trauma. Patients not admitted directly to HUS and patients dead on arrival were excluded.
Baseline demographic information and clinical data were extracted from the HUS trauma registry and the NTR. The HUS trauma registry was prospectively maintained by dedicated trauma registrars which screen emergency patient admissions fulfilling predefined criteria in the local trauma registry until 2015. Thereafter, registration continued in the web-based NTR. In both registries, patients were labeled according to the AIS score (2005 version, update 2008) [19]. Patients were identified in the databases by selecting for thoracic injury AIS codes. Patient data was collected using a standardized case report form. Data on comorbidities, medication use and complications were supplemented by additional retrospective data collection. Patients with no record of comorbidities or medication use were distinguished from the cases where the absence of comorbidities was explicitly recorded. ISS, Glasgow Coma Scale (GCS), revised trauma score (RTS) and the trauma and injury severity Score (TRISS) were calculated at patient admission [16, 20, 21]. ISS ≥ 16 was applied as cutoff for polytrauma patients. Comorbidity data were scored according to the American Society of Anesthesiologists (ASA) score, Charlson comorbidity index (CCI) and comorbidity polypharmacy score (CPS) [22,23,24]. Complications were scored with the trauma adapted Clavien–Dindo scale (CDS) which classifies complications upon the most intensive therapy required complication treatment [25, 26]. To give an overview of all complications to a patient, the comprehensive complication index (CI) was calculated and analyzed [27].
Statistical analyses
Primary end-point was 30-days mortality. The following factors and variables were analyzed for their contribution as a risk factor for in-hospital mortality. Age was categorized in four groups: 0–39, 40–59, 60–74 and 75 years and older. Comorbidities scored with CCI were categorized as 0, 1 and ≥ 2, according to common practice [28]. CPS was categorized as 0–9 and > 9 as appropriate [29] and also analyzed continuously. ISS was divided into three categories: minor 0–9, moderate 10–15, and severe with 16 and higher. RTS was stratified by odds of survival: low risk of death < 5% RTS ≥ 7.2, an intermediate risk of death ≥ 5% < 50% RTS ≥ 3.4 < 7.2, and a high risk of death ≥ 50% RTS < 3.4 [30]. TRISS was analyzed as a categorical variable in three categories with probability of survival (PS) 0–50, 51–75 and 76–100. ASA, Intensive care unit (ICU) and use of anticoagulants were regarded dichotomously. CDS was categorized in two groups, no or minor complications and severe CDS ≥ 3. Complications scored with CI were categorized as no or minor complications CI < 30, and severe CI ≥ 30 as previously reported [31]. The cut-off value for the CI was set at 30 to differentiate between major and minor complications based on the calculation of all possible comprehensive complication indices considering the worst complication as CDS grade two.
Categorical variables were presented using frequencies and percentages and tested using Pearson’s chi square test or Fischer exact test depending on the expected count > 5: Pearson, < 5: Fischer. Normally distributed variables were presented using means and standard deviations and tested using t tests and repeated measures ANOVAs. Non-Gaussian variables were presented as median and inter quartile range (IQR) and tested with the Kruskal–Wallis test.
Separate analyses for specific patient groups were conducted: (1) isolated thoracic injury with ISS < 16, (2) polytrauma without TBI which was defined as no AIS ≥ 3 head injury, and (3) polytrauma with AIS ≥ 3 head injury (TBI). Logistic regression analyses were executed with stepwise backward selection to identify risk factors for mortality following thoracic trauma. The p-value for inclusion of a variable in the logistic models was set at 0.157. As there were several variables that were used as a measure of the same factor, several different models were made to test each variable. To investigate a potential confounding influence of penetrating trauma, models with and without penetrating thoracic injuries were analyzed. The number of events (deaths, n = 4) in the isolated thoracic trauma patient group was too small to conduct a meaningful risk factor for mortality analysis with multivariate logistic regression. For each model, Hosmer–Lemeshow goodness of fit tests and areas under the Receiver Operating Characteristic (ROC) curve were calculated [32]. The best model was selected after calculating all the models, based on the Hosmer–Lemeshow test and the area under the ROC curve of the respective models. All statistical analyses were performed using StataCorp 2017 Stata Statistical Software: Release 15.
Results
Patient demographics
In total, 4042 patients were admitted during the inclusion period, of which 514 patients with thoracic injuries were included for analyses (Fig. 1). The mean annual incidence rate of severe thoracic trauma per 100,000 inhabitants remained the same during the study period, with a ten-year average of 13.3 cases (Fig. 2). Mean (SD) age was 51 [18] years and 78% were male (Table 1). Severe comorbidities according to CCI were present in 190 (40%) patients. Median (IQR) CPS was 0 (0–4). Most patients were in normal health status according to ASA classification (55%). Anticoagulants were used by 85 (17%) patients.
Mechanism of injury
Most frequent mechanism of injury was road traffic accident (RTA) (Table 2). Overall, RTAs made up for 49% of mechanisms of injury with car crashes being the most frequent cause among RTAs (26%) followed by motorcycle crashes (9%), cycling accidents (7%) and injured pedestrians (3%). Falls made up for most of the remaining injuries (35%).
Injury characteristics, treatment and complications
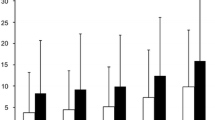
Median ISS was 17 (13–27) and median RTS was 7.8 (7.1–7.8) (Table 1). Most commonly co-occurring injuries were head and abdominal injuries. Rib fractures were the most prevalent thoracic injury, occurring in 426 (83%) patients (Table 3). In 19 (4%) patients an emergency thoracotomy was performed. In 126 (25%) patients a chest tube was placed. Complications occurred in 189 (37%) patients (Table 4, Fig. 3). Most common severe complication (CDS ≥ 3) was respiratory failure in 70 (14%) patients. Within the first 24 h after the accident 24 (5%) patients died (Fig. 4). Sixty patients (12%) died within 30 days after the accident. Three hundred thirteen (61%) patients were polytrauma casualties.
Risk factors for mortality following thoracic trauma
The analyses showed that female sex, more than nine comorbidities and medication use combined, a TRISS with a PS of lower than 50% and all the complications of a patient with a CI ≥ 30 were associated with an adverse outcome after trauma (Table 5). The final model (Hosmer–Lemeshow goodness of fit test (p = 0.4), area under ROC curve (0.93) consisted of the predictors mentioned above. Females had a 2.7 times higher risk of dying compared to male victims (OR 2.7, p = 0.04). Having more than nine comorbidities and medication use combined lead to nearly five times higher risk of dying (OR 4.8, p = 0.01). TRISS was also a strong risk factor for mortality where patients with a PS of 0 to 50%, having a 44 times higher risk of dying (OR 44, p < 0.001). Finally, patients with severe complications measured by CI, resembling a minimal complication of CDS grade ≥ 3, were 12.5 times more likely to die compared to those having a mild or no complication (OR 12.5, p < 0.001). Anticoagulants were no risk factors for mortality in this study. No confounding effect of penetrating thoracic injuries was observed. The analyses with penetrating thoracic trauma excluded showed the same significant results (online resource supplementary Table 1). Characteristics of the patients included and excluded in the risk factor for mortality analyses are given in Table 6.
Analyses of specific patient groups
Subgroup analyses were conducted for three specific groups: 201 isolated thoracic trauma patients, 215 polytrauma without TBI and 98 polytrauma with TBI patients (Table 2). Mean age (SD) of polytrauma patients with TBI was significantly lower (47, 19) than polytrauma without TBI patients (52, 19) and isolated thoracic trauma patients (53, 18), (p < 0.001). There were no differences in sex distribution or comorbidities between subgroups. Low-energy falls < 3 m were relatively frequent (15%) in isolated thoracic trauma compared to the other patient groups. High energy falls > 3 m were more often the causative mechanism in both polytrauma groups. Median (IQR) ISS was significantly higher in polytrauma without TBI (22, 17–29) and polytrauma with TBI (29, 22–41) than in isolated thoracic injury (11, 9–13), (p < 0.001). In the polytrauma without TBI group the highest number of AIS ≥ 3 thoracic injuries were observed with 102 (48%) patients with two or more AIS ≥ 3 thoracic injuries. There were 44 (45%) patients with severe complications in the polytrauma with TBI group. This was significantly higher than the 60 (28%) patients in the polytrauma without TBI group and the 19 (10%) patients in the isolated thoracic trauma group (p < 0.001). The highest mortality was observed in the polytrauma with TBI group with 25 (25%) deaths. In polytrauma without TBI the highest number of fatalities occurred within 24 h after trauma with 18 (58%) deaths, while the majority of deaths in polytrauma with TBI occurred on the second day with 11 (45%) deaths (Fig. 4). Main cause of death in the polytrauma without TBI group was exsanguination. In the polytrauma with TBI group main cause of death was brain injury. Risk factor for mortality analyses for specific subgroups did not reveal other risk factors for mortality than in the total thoracic trauma cohort in this study. Female sex was no risk factor for mortality in polytrauma without TBI (online resource supplementary Tables 2, 3).
Data quality
Data was missing in the following variables: injury mechanism (5.3%), nature of the trauma mechanism (2.0%), GCS (3.3%), RTS (2.3%), TRISS (4.3%) ASA (11.5%) CCI (4.7%) CPS (5.8%) anticoagulants (6.4%), first emergency procedure (1.0%), chest tube (4.1%) complications (2.3%). Missing data were likely not to be random; mortality was significantly higher in the group of patients with missing data on any of the variables.
Discussion
The present study aimed to clarify epidemiological data, injury characteristics, in-hospital outcomes and risk factors for mortality following severe thoracic trauma at a level one trauma center. Based upon a cohort of 514 adult patients, this study demonstrated that more than nine comorbidities and medication use combined, TRISS, female sex, as well as severe complications, were significant risk factors for mortality following severe thoracic trauma. Analyses of specific patient groups did not demonstrate other risk factors.
Epidemiology of thoracic trauma in Western Norway and mortality
The average of 51 treated patients with severe thoracic injury at HUS per year is roughly comparable to other hospitals that have studied thoracic trauma patients [6, 9]. The incidence rate of polytraumatized patients with severe thoracic trauma in Western Norway (8/100,000 inhabitants) was comparable to that of the Netherlands (9/100,000 inhabitants). The percentage of car accidents as cause of severe thoracic trauma with polytrauma in HUS (50%), was relatively low compared to the university hospital of Helsinki (58%) and German hospitals (64%) [6]. It is known that Norway is one of the safest countries with regards to traffic and has one of the lowest traffic accident mortality rates in the world [33]. Mortality after severe thoracic trauma in polytrauma varies within the current literature, ranging from 10 to 18%, with no cohorts exactly matching this study [4,5,6, 9, 34]. In this study, overall mortality in the polytrauma group, a cohort similar with the aforementioned literature, was relatively high with 18%. There were no general trends in different age, ISS or comorbidities if reported in those studies compared to HUS. Future studies are required to determine the cause of this difference in mortality.
Mortality in this study was not according to the classical trimodal pattern of trauma deaths by Trunkey et al. [35]. The classical model describes deaths on scene, these were not included in this study, early deaths within 6 h after trauma, and a third peak of late deaths three to 4 weeks after trauma. This late peak was not observed in this study. As shown before, it is hypothesized that the late peak of deaths due to sepsis and respiratory insufficiency does not occur due to improvements in health care systems [36]. In this study mortality in polytrauma without TBI was the highest in the first 24-h after trauma due to exsanguination. In polytrauma with TBI the highest mortality was later than 24-h after trauma, and the main reason for death in this subgroup was brain injury. Deaths due to exsanguination in this study show the second peak of early deaths of the classical trimodal pattern of trauma deaths, and primary brain injury deaths do not, with most of brain injury deaths occurring later than 24-h after trauma. This is in line with current literature [36,37,38].
Comorbidity as risk factor for mortality
Comorbidities that have been shown to predict mortality after trauma are: hepatic and renal disease, congestive heart failure, hypertension, pulmonary disease, diabetes, malignancy, obesity, peripheral artery disease and neurologic disorders [5, 39,40,41,42,43]. This study demonstrates patients having more than nine comorbidities and medication use combined measured by CPS, to have a considerably higher mortality risk compared to patients with relatively few or no comorbidities (OR 4.8, p = 0.011). This was demonstrated using a relatively novel, standardized instrument for quantifying comorbidities. A (geriatric) trauma study by Nossaman et al. in 2018 reported CPS to be a risk factor for mortality, although patients with a higher CPS demonstrated lower mortality risk [44]. The authors hypothesized that patients with known comorbidities and the respective medication use may have returned to a better physiologic conditions than their peers with unknown comorbidities and medication (a low measured CPS). These patients might have suffered from the same comorbidities but were not treated and therefore had a higher mortality risk. We hypothesize that the number of care avoiders in Norway is low due to a free health care system while as much as 45% of US citizens delays or avoids medical care due to costs [45]. Hence, Norwegian patients with a high CPS may be less healthy than Norwegian patients with a low CPS, they may thus have a higher mortality risk.
It has been debated whether higher mortality in older patients is caused by ageing itself or rather by more comorbidities in elderly patients [41, 46]. The present study demonstrates that comorbid conditions independently predict mortality. This is supported by Milzman et al. who showed that the effect of comorbidities on mortality in trauma patients proved consistent over all age and injury severity groups [40]. The main reason for adverse outcomes in patients with severe comorbidities is the reduced physiological reserve that is caused by comorbidities [11].
CPS as a predictor of mortality
In the present study, CPS as a measure of comorbidities, appeared to be the strongest predictor of mortality, even stronger than the CCI. The literature on this topic is contradicting, since both CPS and CCI have previously shown to predict mortality in trauma [47, 48]. However, to the best of our knowledge, CPS and CCI have not been compared. In our study, the number of comorbidities combined with medication use is a more accurate predictor of mortality than the comorbidities included in the CCI. This suggests that there are other relevant comorbidities influencing survival that are not included in the CCI. With this result, we would like to emphasize, that the number of comorbid conditions and medication use is a helpful tool to estimate mortality risk in thoracic trauma patients.
Injury severity
Several trauma outcomes and injury severity scores are related to injury severity. In the present study injury severity in thoracic trauma is best measured by TRISS. The TRISS value is based upon registered ISS and RTS as well as age and type of trauma, hence giving an estimation of probability of mortality following trauma. It is well known that the anatomical severity of the injury combined with the physiological burden to the body is the best measure of injury severity and therefore the strongest predictor for mortality after trauma [49, 50].
Complications
This is, to our knowledge, the first study that provides an overview of all complications that occur after severe thoracic trauma with a standardized method. We find the overall complication rate of thoracic trauma to be comparable with complication rates mentioned in recent studies on rib fractures in polytrauma patients, both in polytrauma patients in general as well as in geriatric [5, 8, 51]. This study emphasizes the high risk of pulmonary complications occurring after thoracic trauma, and the higher mortality in this patient group. Pneumonia and respiratory failure were frequently observed in our material. Also, patients with a CI ≥ 30, representing severe complications of CDS grade 3 and higher were more likely to die (OR 12.5, p < 0.001). Of CDS grade 3 and higher complications, 65% were pulmonary complications. It has been observed that respiratory complications are a frequent cause of death in older patients [8, 14]. The multivariate models with CI were marginally better than the models with CDS, both were therefore risk factors for mortality in this study. The number of severe complications was significantly higher in the polytrauma with TBI group than in isolated thoracic trauma and polytrauma without TBI subgroups. This result can be explained by polytrauma with TBI being the most severely injured patient group with the highest ISS, and deaths due to brain injury occur relatively late compared to exsanguination, therefore there is more time to develop complications.
Age and use of anticoagulants
An unexpected finding in the present study was that age and anticoagulants were no independent risk factors for mortality. In none of the analyzed models, age was an independent risk factor for mortality. Advancing age leads to a higher mortality and has been found to be a risk factor for mortality in a large number of previous studies [4, 9, 12, 43, 52, 53]. The exact relationship between mortality, age and comorbidities remains debated. The present and other studies suggest that comorbidities accompanying advanced age contribute to mortality, as opposed to age alone [54].
Anticoagulant use predicts mortality after head trauma [55]. However, anticoagulant use did not emerge as predictor of mortality among our patients. The sample size may have been too small to demonstrate an effect of higher bleeding tendency on mortality. In addition, anticoagulant use also means that the patient has comorbidities. The models with CPS included, appear to be a stronger predictor for mortality than anticoagulant use alone. These effects could have caused anticoagulants not to become a significant predictor in our material.
Potential limitations of the present study arise mostly from its retrospective character. Underestimation of effects could be caused due to missing data on comorbidities, medication use and complications in patients that die within the first 24 h after the accident. Patients who died on scene are excluded. In Hordaland county, of which HUS is both the local and level one trauma center, 72% of patients who die after trauma, die at the scene or before arrival at a hospital [56]. This may cause an underestimation of the contribution of the investigated factors on mortality. Subgroups were relatively small and this may be the reason that no other risk factors were found in the subgroup analyses. Complications were defined as all adverse events graded by CDS occurring on the ward or in the ICU in patients after the initial stabilization and treatment. This could be a limitation in the risk factor for mortality analyses in patients who died in the first 48 h after trauma. There is a partial similarity between injury severity and complications. The significant risk factor complications might have become significant partially by the mortality in the first 48 h after trauma due to the severity of the injury.
In this study severe complications CD ≥ 3 were a significant risk factor for mortality and these complications occurred in 23% of all patients. It is important to be aware of patients at risk of developing a severe complication. These patients should be monitored intensively and treated aggressively as soon as complications occur to prevent further health deterioration. To the best of our knowledge, only one study on risk factors for complications in thoracic trauma exists, focusing solely on pneumonia [13]. Future studies should focus on identifying risk factors for complications following thoracic trauma, with subgroup analyses of patients who survive the first 48 h, to gain insight in patients at risk and in need of active trauma level one treatment.
Conclusions
The present study demonstrates thoracic injury to be common within the Haukeland University Hospital catchment area, causing relatively high mortality. In a model with multiple known risk factors, more than nine comorbidities and medications combined, TRISS, female sex, and severe complications predict mortality after thoracic trauma. In analyses of patient groups with polytrauma and without TBI, and polytrauma with TBI, no significant other risk factors were found. This study highlights the importance of gathering information about the patient and the injury mechanism as early as possible in the trauma evaluation process and early care when severe thoracic injury is suspected. Current findings may help to recognize patients at risk of an adverse outcome and prevent complications.
Availability of data and materials
The data that support the findings of this study are available from the University of Bergen, Haukeland University Hospital, Western Norway Trauma Center, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Haukeland University Hospital.
Code availability
Not applicable.
Abbreviations
- AIS:
-
Abbreviated injury scale
- OR:
-
Odds ratio
- ISS:
-
Injury severity score
- TBI:
-
Traumatic brain injury
- HUS:
-
Haukeland University Hospital
- NTR:
-
National Trauma Registry
- GCS:
-
Glasgow coma scale
- RTS:
-
Revised trauma score
- TRISS:
-
Trauma and injury severity score
- ASA:
-
American Society of Anesthesiologists
- CCI:
-
Charlson comorbidity index
- CPS:
-
Comorbidity polypharmacy score
- CDS:
-
Clavien–Dindo scale
- CI:
-
Comprehensive complication index
- PS:
-
Probability of survival
- ICU:
-
Intensive care unit
- IQR:
-
Inter quartile range
- ROC:
-
Receiver operating characteristics
- RTA:
-
Road traffic accident
References
Vecsei V, Arbes S, Aldrian S, Nau T. Chest injuries in polytrauma. Eur J Trauma. 2005;31:239–43.
Bayer J, Lefering R, Reinhardt S, Kuhle J, Sudkamp NP, Hammer T, et al. Severity-dependent differences in early management of thoracic trauma in severely injured patients—analysis based on the TraumaRegister DGU(R). Scand J Trauma Resusc Emerg Med. 2017;25(1):10.
Trupka A, Kierse R, Waydhas C, Nast-Kolb D, Blahs U, Schweiberer L, et al. Shock room diagnosis in polytrauma Value of thoracic CT. Unfallchirurg. 1997;100(6):469–76.
Huber S, Biberthaler P, Delhey P, Trentzsch H, Winter H, van Griensven M, et al. Predictors of poor outcomes after significant chest trauma in multiply injured patients: a retrospective analysis from the German Trauma Registry (Trauma Register DGU(R)). Scand J Trauma Resusc Emerg Med. 2014;3(22):52–4.
Peek J, Ochen Y, Saillant N, Groenwold RHH, Leenen LPH, Uribe-Leitz T, et al. Traumatic rib fractures: a marker of severe injury. A nationwide study using the National Trauma Data Bank. Trauma Surg Acute Care Open. 2020. https://doi.org/10.1136/tsaco-2020-000441.
Heinanen M, Brinck T, Lefering R, Handolin L, Soderlund T. Resource use and clinical outcomes in blunt thoracic injury: a 10-year trauma registry comparison between southern Finland and Germany. Eur J Trauma Emerg Surg. 2018;45(4):585–95.
Mommsen P, Zeckey C, Andruszkow H, Weidemann J, Fromke C, Puljic P, et al. Comparison of different thoracic trauma scoring systems in regards to prediction of post-traumatic complications and outcome in blunt chest trauma. J Surg Res. 2012;176(1):239–47.
de Vries R, Reininga IHF, de Graaf MW, Heineman E, El Moumni M, Wendt KW. Older polytrauma: mortality and complications. Injury. 2019;50(8):1440–7.
Kjøs HO, Lande TM, Eriksson U, Nordhaug D, Karevold A, Haaverstad R. Thoracic injuries at a regional trauma centre. Tidsskr Nor Laegeforen. 2007;127(11):1496–9.
de Vries R, Reininga IHF, Pieske O, Lefering R, El MM, Wendt K. Injury mechanisms, patterns and outcomes of older polytrauma patients—an analysis of the Dutch trauma registry. PLoS One. 2018;13(1):1–10.
Atinga A, Shekkeris A, Fertleman M, Batrick N, Kashef E, Dick E. Trauma in the elderly patient. Br J Radiol. 2018;91(1087):20170739.
Battle CE, Hutchings H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury. 2012;43(1):8–17.
Brasel KJ, Guse CE, Layde P, Weigelt JA. Rib fractures: relationship with pneumonia and mortality. Crit Care Med. 2006;34(6):1642–6.
Marini CP, Petrone P, Soto-Sánchez A, García-Santos E, Stoller C, Verde J. Predictors of mortality in patients with rib fractures. Eur J Trauma Emerg Surg. 2019. https://doi.org/10.1007/s00068-019-01183-5 (0123456789).
Leijdesdorff HA, Gillissen S, Schipper IB, Krijnen P. Injury pattern and injury severity of in-hospital deceased road traffic accident victims in The Netherlands: Dutch road traffic accidents fatalities. World J Surg. 2020;44(5):1470–7.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96.
Ringdal KG, Hestnes M, Svege I, Røise O. Definisjonskatalog for Nasjonalt Traumeregister. Vol. 2019. 2017. Available from: http://www.ntr-definisjonskatalog.no/
Regional Committees for Medical and Health Research Ethics (REC). Vol. 2017. 2017. Available from: https://helseforskning.etikkom.no/?_ikbLanguageCode=us
medicine A for the advancement of automotive. Abbreviated Injury Scale © 2005 Update 2008. 2008. 1981–2000 p. Vol. 2019. 2015. Available from: https://www.aaam.org/abbreviated-injury-scale-ais/
Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the trauma score. J Trauma. 1989;29(5):623–9.
Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma. 1987;27(4):370–8.
Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941;2(3):281–4.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Justiniano CF, Evans DC, Cook CH, Eiferman DS, Gerlach AT, Beery PR 2nd, et al. Comorbidity-polypharmacy score: a novel adjunct in post-emergency department trauma triage. J Surg Res. 2013;181(1):16–9.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Naumann DN, Vincent LE, Pearson N, Beaven A, Smith IM, Smith K, et al. An adapted Clavien-Dindo scoring system in trauma as a clinically meaningful nonmortality endpoint. J Trauma Acute Care Surg. 2017;83(2):241–7.
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258(1):1–7.
Stavem K, Hoel H, Skjaker SA, Haagensen R. Charlson comorbidity index derived from chart review or administrative data: agreement and prediction of mortality in intensive care patients. Clin Epidemiol. 2017;2(9):311–20.
Guidet B, de Lange DW, Boumendil A, Leaver S, Watson X, Boulanger C, et al. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med. 2020;46(1):57–69.
Kondo Y, Abe T, Kohshi K, Tokuda Y, Cook EF, Kukita I. Revised trauma scoring system to predict in-hospital mortality in the emergency department: Glasgow Coma Scale, Age, and Systolic Blood Pressure score. Crit Care. 2011;15(4):R191.
Ray S, Mehta NN, Mangla V, Lalwani S, Mehrotra S, Chugh P, et al. A comparison between the comprehensive complication index and the Clavien-Dindo grading as a measure of postoperative outcome in patients undergoing gastrointestinal surgery-a prospective study. J Surg Res. 2019;244:417–24.
Hosmer D, Lemeshow S. No Title. In: Applied logistic regression. 2nd edn. New York: John Wiley and Sons; 2000. p. 160–4.
International Transport Forum. Road safety annual report 2020. Sustainability (Switzerland). 2020;4:1–9.
Peek J, Beks RB, Hietbrink F, De Jong MB, Heng M, Beeres FJP, et al. Epidemiology and outcome of rib fractures: a nationwide study in the Netherlands. Eur J Trauma Emerg Surg. 2022;48(1):265–71.
Trauma TDD. Accidental and intentional injuries account for more years of life lost in the U.S. than cancer and heart disease. Among the prescribed remedies are improved preventive efforts, speedier surgery and further research. Sci Am. 1983;249(2):28–35.
Gunst M, Ghaemmaghami V, Gruszecki A, Urban J, Frankel H, Shafi S. Changing epidemiology of trauma deaths leads to a bimodal distribution. Baylor Univ Med Cent Proc. 2010;23(4):349–54.
de Knegt C, Meylaerts SAG, Leenen LPH. Applicability of the trimodal distribution of trauma deaths in a Level I trauma centre in the Netherlands with a population of mainly blunt trauma. Injury. 2008;39(9):993–1000.
Lefering R, Paffrath T, Bouamra O, Coats TJ, Woodford M, Jenks T, et al. Epidemiology of in-hospital trauma deaths. Eur J Trauma Emerg Surg. 2012;38(1):3–9.
Grossman MD, Miller D, Scaff DW, Arcona S. When is an elder old? Effect of preexisting conditions on mortality in geriatric trauma. J Trauma. 2002;52(2):242–6.
Milzman DP, Boulanger BR, Rodriguez A, Soderstrom CA, Mitchell KA, Magnant CM. Pre-existing disease in trauma patients: a predictor of fate independent of age and injury severity score. J Trauma. 1992;32(2):234–6.
Wutzler S, Maegele M, Marzi I, Spanholtz T, Wafaisade A, Lefering R. Association of preexisting medical conditions with in-hospital mortality in multiple-trauma patients. J Am Coll Surg. 2009;209(1):75–81. https://doi.org/10.1016/j.jamcollsurg.2009.03.015.
Alexander JQ, Gutierrez CJ, Mariano MC, Vander Laan T, Gaspard DJ, Carpenter CL, et al. Blunt chest trauma in the elderly patient: how cardiopulmonary disease affects outcome. Am Surg. 2000;66(9):855–7.
Harrington DT, Phillips B, Machan J, Zacharias N, Velmahos GC, Rosenblatt MS, et al. Factors associated with survival following blunt chest trauma in older patients: results from a large regional trauma cooperative. Arch Surg. 2010;145(5):432–7.
Nossaman VE, Larsen BE, DiGiacomo JC, Manuelyan Z, Afram R, Shukry S, et al. Mortality is predicted by Comorbidity Polypharmacy score but not Charlson Comorbidity Index in geriatric trauma patients. Am J Surg. 2018;216(1):42–5.
Smith KT, Monti D, Mir N, Peters E, Tipirneni R, Politi MC. Access is necessary but not sufficient: factors influencing delay and avoidance of health care services. MDM Policy Pract. 2018;3(1):238146831876029.
Wutzler S, Lefering R, Laurer HL, Walcher F, Wyen H, Marzi I, et al. Changes in geriatric traumatology. An analysis of 14,869 patients from the German Trauma Registry. Unfallchirurg. 2008;111(8):592–8.
Evans DC, Cook CH, Christy JM, Murphy CV, Gerlach AT, Eiferman D, et al. Comorbidity-polypharmacy scoring facilitates outcome prediction in older trauma patients. J Am Geriatr Soc. 2012;60(8):1465–70.
Meagher AD, Lin A, Mandell SP, Bulger E, Newgard C. A comparison of scoring systems for predicting short- and long-term survival after trauma in older adults. Acad Emerg Med. 2019. https://doi.org/10.1111/acem.13727.
Serviá L, Badia M, Montserrat N, Trujillano J. Severity scores in trauma patients admitted to ICU. Physiological and anatomic models. Med Intensiva. 2019;43(1):26–34.
Laytin AD, Dicker RA, Gerdin M, Roy N, Sarang B, Kumar V, et al. Comparing traditional and novel injury scoring systems in a US level-I trauma center: an opportunity for improved injury surveillance in low- and middle-income countries. J Surg Res. 2017;215:60–6.
Saltzherr TP, Visser A, Ponsen KJ, Luitse JS, Goslings JC. Complications in multitrauma patients in a dutch Level 1 trauma center. J Trauma. 2010;69(5):1143–6.
Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma. 2000;48(6):1040–7.
Cuevas-Østrem M, Røise O, Wisborg T, Jeppesen E. Epidemiology of geriatric trauma patients in Norway: a nationwide analysis of Norwegian Trauma Registry data, 2015–2018. A retrospective cohort study. Injury. 2021;52(3):450–9.
Morris JA Jr, MacKenzie EJ, Edelstein SL. The effect of preexisting conditions on mortality in trauma patients. JAMA. 1990;263(14):1942–6.
Scotti P, Seguin C, Lo BWY, de Guise E, Troquet JM, Marcoux J. Antithrombotic agents and traumatic brain injury in the elderly population: hemorrhage patterns and outcomes. J Neurosurg. 2019;5:1–10.
Bakke HK, Hansen IS, Bendixen AB, Morild I, Lilleng PK, Wisborg T. Fatal injury as a function of rurality-a tale of two Norwegian counties. Scand J Trauma Resusc Emerg Med. 2013;21:14.
Acknowledgements
The authors would like to thank Geir Egil Eide for his help with the statistical analysis. We also would like to thank Vigdis-Giil Jensen for her help with retrieving missing data.
Funding
B.K. Johannesdottir received a grant from the Helga Jonsdottir and Sigurliði Kristjansson Memorial Fund and the Scientific Fund of Landspitali University Hospital in connection to this study.
Author information
Authors and Affiliations
Contributions
ATF contributed to this study by performing literature research, setting up the design, performing data collection, data analysis, data interpretation and writing of the manuscript. BKJ contributed to this study by data collection, in writing and critical revision. KW contributed by setting up the design, critical revision. RH contributed by critical revision. IHFR contributed in setting up the design, statistical analysis, critical revision, TG contributed by critical revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This research was registered and approved by the regional committees for medical and health research ethics in Norway under file number 2017/293.
Consent to participate
All participants were asked for consent and were given to opportunity to withdraw from the study.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fokkema, A.T., Johannesdottir, B.K., Wendt, K. et al. Comorbidities, injury severity and complications predict mortality in thoracic trauma. Eur J Trauma Emerg Surg 49, 1131–1143 (2023). https://doi.org/10.1007/s00068-022-02177-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02177-6