Abstract
Purpose
The study aimed to investigate the association between out-of-hours surgery and postoperative mortality in hip fracture patients. Furthermore, internal fixation and arthroplasty were compared to determine if a difference could be observed in patients operated with these techniques at different times during the day.
Methods
All patients above 18 of age years in Sweden who underwent hip fracture surgery between 2008 and 2017 were eligible for inclusion. Pathological fractures, non-operatively managed fractures, or cases whose time of surgery was missing were excluded. The cohort was subdivided into on-hour (08:00–17:00) and out-of-hours surgery (17:00–08:00). Poisson regression with adjustments for confounders was used to evaluate the association between out-of-hours surgery and both 30-day and 90-day postoperative mortality.
Results
Out-of-hours surgery was associated with a 5% increase in the risk of both 30-day [adj. IRR (95% CI) 1.05 (1.00–1.10), p = 0.040] and 90-day [adj. IRR (95% CI) 1.05 (1.01–1.09), p = 0.005] mortality after hip fracture surgery compared to on-hour surgery. There was no statistically significant association between out-of-hours surgery and postoperative mortality among patients who received an internal fixation. Arthroplasties performed out-of-hours were associated with a 13% increase in 30-day postoperative mortality [adj. IRR (95% CI) 1.13 (1.04–1.23), p = 0.005] and an 8% increase in 90-day postoperative mortality [adj. IRR (95% CI) 1.08 (1.01–1.15), p = 0.022] compared to on-hour surgery.
Conclusion
Out-of-hours surgical intervention is associated with an increase in both 30- and 90-day postoperative mortality among hip fracture patients who received an arthroplasty, but not among patients who underwent internal fixation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical controversy remains regarding the optimal timing of hip fracture surgery [1,2,3,4,5]. A recent randomized control trial (RCT), the HIP ATTACK study, failed to demonstrate an overall association between expedited surgery (within 6 h of hip fracture diagnosis) and the abrogation of the risk of postoperative complications or death [6]. However, granular analysis suggests specific patient populations, such as those in need of internal fixation of displaced femoral neck fractures may benefit from earlier operative intervention [7,8,9]. In contrast, those requiring formal arthroplasty may be hypothesized to accrue a more considerable benefit from preoperative optimization [10, 11].
There is great global heterogeneity in unscheduled access to the operating room, limited by philosophy, logistics, and resources. In some health care systems (such as the United Kingdom), out-of-hours surgery is sanctioned only for true threats to life or limb [12, 13], while in others, orthopedic trauma surgical practice patterns, including hip fracture surgery, facilitate and encourage out-of-hours intervention [14]. As the global population ages and this injury pattern becomes more prevalent, an evidence base for the optimal timing of the surgical treatment of hip fractures will become even more relevant [15,16,17]. This vulnerable, highly comorbid patient population places a heavy burden on health care systems [18,19,20,21,22,23,24]. It is, therefore, vital that all avenues are explored to achieve a reduction in mortality, which has hitherto remained relatively constant despite efforts taken to reduce this during the past decades [18, 25]. Previous studies investigating the effect of time-of-day on postoperative mortality have observed varying outcomes. A large study including all orthopedic trauma was able to find an association between out-of-hours surgery and increased postoperative mortality [26]. To date, studies that specifically focused on hip fracture surgery were unable to detect a similar association [27,28,29,30,31,32,33,34]. Interpretation of these studies, however, is limited by relatively small sample populations [27,28,29,30,31,32,33].
In this study, we aimed to investigate the association between out-of-hours surgery and postoperative mortality in hip fracture patients, using the largest sample population to date, and to determine if a difference could be observed in patients operated with internal fixation compared to those who received an arthroplasty. We hypothesized that out-of-hours surgery is associated with an increased risk of mortality.
Patients and methods
The study was approved by the Swedish Ethical Review Authority (ref: 2020-03257) and adhered to the STROBE guidelines and the Declaration of Helsinki [35]. Data were primarily retrieved from Rikshoft, the prospectively collected Swedish National Quality Registry for Hip Fracture Patients [36]. All adult patients (18 years or older) in Sweden who underwent hip fracture surgery between January 1, 2008, and December 31, 2017, were eligible for inclusion. Cases where the fracture was pathological, non-operatively managed, or whose time of surgery was missing were excluded from further analysis. Patient data from Rikshoft was cross-referenced with patients’ preoperative comorbidities and time of death in the Swedish National Board of Health and Welfare’s Patient and Cause of Death Registers. Comorbidities were used to calculate the Charlson Comorbidity Index (CCI) [37].
Statistical analysis
Cases were divided into two cohorts based on if the surgery was initiated on-hours (08:00–17:00) or out-of-hours (17:00–08:00). The timespans are based on the working hours for the overwhelming majority of healthcare providers in Sweden, where the “on-call” schedule starts at 17:00. Subsequently, patient demographics, clinical characteristics, and crude outcomes were compared between these two shifts using the appropriate statistical tests. Continuous, normally distributed variables were presented as a mean and standard deviation (SD), with the Student’s t test being used to evaluate the statistical significance of differences between the groups. Non-normally distributed, continuous variables were presented as a median and interquartile range (IQR); the Mann–Whitney U test was employed to determine the statistical significance of differences. Counts and percentages summarize categorical variables, while Pearson’s Chi-squared test was used to test for independence between the groups.
The primary outcome was 30-day postoperative mortality, with 90-day postoperative mortality being the secondary outcome of interest. We applied two time-bound Poisson regression models with robust standard errors to the data (with 30- and 90-day postoperative mortality as the response variable, respectively) to investigate the association between out-of-hours surgery and mortality. Both models were adjusted for age, sex, American Society of Anesthesiologists (ASA) classification, type of fracture, type of surgery, time to surgery, myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic obstructive pulmonary disease, connective tissue disease, liver disease, diabetes, chronic kidney disease, local cancer, and metastatic carcinoma. These analyses were repeated on a subset of patients who were operated on using internal fixation (pins/screws, pins/screws with side-plate, or intramedullary nail) or arthroplasty (hemiarthroplasty or total hip replacement) since the latter surgical procedures are considered technically more demanding and time-consuming as well as more physiologically traumatic for the patients. Results are presented as incidence rate ratios (IRRs) with 95% confidence intervals (CIs). Statistical significance was defined as a two-sided p value less than 0.05. Analyses were performed using the statistical programming language R (R Foundation for Statistical Computing, Vienna, Austria) [38].
Results
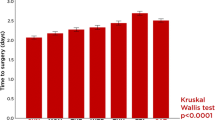
Based on the inclusion and exclusion criteria, a total of 130,407 hip fracture cases were available for further analysis. A total of 87,253 (67%) received an internal fixation while 43,092 (33%) underwent an arthroplasty. Irrespective of the type of surgery, most patients were operated on-hours (Fig. 1). There was no statistically significant difference in the age or sex of patients in either cohort, as well as no clinically significant difference in the fitness for surgery based on their ASA classification. In general, patients who were operated out-of-hours had a slightly lower comorbidity burden (CCI ≥ 7: 17.7% vs. 19.2%, p < 0.001); all comorbidities were less prevalent among patients undergoing out-of-hours surgery, except for hemiplegia, liver disease, and peptic ulcer disease. Patients who were operated out-of-hours were more likely to undergo internal fixation (74.2% vs. 63.9%, p < 0.001), and to undergo surgery within 24 h of admission (69.6% vs. 68.5%, p < 0.001). This was reflected in an overall shorter length of stay (7 vs. 8 days, p < 0.001), but crude 90-day postoperative mortality was slightly higher (13.6% vs. 13.1%, p = 0.008) (Table 1).
When comparing the cohorts in the subset of patients operated with internal fixation, differences between the cohorts were relatively unchanged compared to the entire patient population. The primary change was that there was no statistically significant difference in the proportion of patients who underwent surgery within 24 h (72.0% vs. 71.4%, p = 0.060). Length of stay was still shorter among patients who were operated out-of-hours (7 vs. 8 days, p < 0.001), but there was no statistically significant difference in crude 30- or 90-day postoperative mortality (Table 2).
Patients undergoing arthroplasty exhibited similar demographics to the entire patient population. There was no clinically significant difference in age and no statistically significant difference in sex, type of fracture, time to surgery, fitness for surgery according to ASA classification, or comorbidity burden based on CCI. The only differences in comorbidity prevalence were seen in hypertension, arrhythmia, chronic obstructive pulmonary disease, connective tissue disease, and local tumors, all of which were less prevalent among patients who underwent surgery out-of-hours. Both crude 30-day (8.6% vs. 7.2%, p < 0.001) and 90-day (13.9% vs. 12.0%, p < 0.001) postoperative mortality was higher among patients who were operated out-of-hours (Table 3).
After adjusting for potential confounders, out-of-hours surgery was associated with a 5% increase in the risk of both 30-day [adj. IRR (95% CI) 1.05 (1.00–1.10), p = 0.040] and 90-day [adj. IRR (95% CI) 1.05 (1.01–1.09), p = 0.005] mortality after hip fracture surgery compared to on-hour surgery. There was no statistically significant association between out-of-hours surgery and postoperative mortality among patients who received an internal fixation. Arthroplasties performed out-of-hours were associated with a 13% increase in 30-day postoperative mortality [adj. IRR (95% CI) 1.13 (1.04–1.23), p = 0.005] and an 8% increase in 90-day postoperative mortality [adj. IRR (95% CI) 1.08 (1.01–1.15), p = 0.022] compared to on-hour surgery (Table 4).
Discussion
This is the most extensive study to investigate the association between out-of-hours surgery and postoperative mortality in hip fracture patients and the first that compares outcomes following emergency internal fixation and arthroplasty. Poisson regression analysis initially indicated that out-of-hours surgery (17:00–08:00) was associated with a 5% increase in both 30- and 90-day mortality in all hip fracture patients. However, subgroup analyses indicated that there was no association present among patients who received an internal fixation. On the other hand, arthroplasty was associated with a 13% increase in 30-day postoperative mortality and an 8% increase in 90-day postoperative mortality.
The effect of out-of-hours procedures has been previously investigated in orthopedic surgery, with conflicting results [26,27,28,29,30,31,32,33,34]. Orthopedic trauma surgery performed during the afternoon and at night is associated with an increase in mortality [26]. However, none of the studies that specifically focused on hip fracture surgery could detect a statistically significant association between out-of-hours surgery and postoperative mortality [27,28,29,30,31,32,33,34]. A straightforward explanation for this could be a lack of statistical power, as most of these studies were only 1/100th the size of the current study [27,28,29,30,31,32,33]. Furthermore, just two of the hip fracture studies appear to have performed adjustments for significant covariates such as comorbidities and ASA classification in their analyses of out-of-hours surgery [33, 34], which increases the risk that their results are affected by residual confounding [27,28,29,30,31,32].
Any association between out-of-hours operating and increased postoperative mortality, while much studied, is likely to be multifactorial and not simply a sequel of surgeon fatigue. The current literature has yet to provide conclusive evidence that fatigue results in a decline in surgical performance [39,40,41,42,43,44]. Moreover, as can be seen in Fig. 1, the majority of out-of-hours operations are performed before midnight, with the peak lying between 19:00 and 20:00; this skewing of the procedures to the early portion of the out-of-hours shift minimizes the risk of surgeon fatigue playing a significant role in the observed increase in postoperative mortality out-of-hours. Another explanation that might be proposed is surgical experience. In general, the out-of-hours tend to be staffed by senior residents or junior specialists, with less access to more experienced surgeons than regular work hours; however, this also seems unlikely to be the cause of the discrepancy. According to the literature, except in rare circumstances, hip fracture surgery itself does not kill patients; they die due to cardiovascular, respiratory, or cerebrovascular events, among other causes [21, 45,46,47,48]. At most, these events can be attributable to the strain induced by the anesthesia, but even the time spent under anesthesia does not appear to be increased out-of-hours [49].
The effect of the type of fracture being operated on also bears consideration, as arthroplasty is primarily performed on displaced cervical hip fractures, which are intracapsular fractures. As it stands, there is no consensus regarding the effect of intra- versus extracapsular fractures on postoperative mortality [50,51,52,53,54]. However, among the studies that observed a difference, extracapsular fractures were the type of fracture that was associated with an increased risk of mortality [50,51,52]. Consequently, this makes it unlikely that the type of fracture can explain the difference observed between internal fixation and arthroplasty.
A more likely cause, in the authors’ opinion, could be the resources available out-of-hours in the hospital setting. During the day, a patient’s vitals may be controlled several times, and the patient will be checked upon many times more. Out-of-hours, these kinds of controls are significantly reduced, both due to a reduction in staff on the wards and to allow patients to recuperate after surgery. This makes it more challenging to both discover complications as well as detect changes in the patient’s status which would allow surgeons to preempt the development of complications. For example, if a surgical wound starts bleeding during the night, it might go unnoticed until the surgeon rounds the patient the following morning, when the patient already has developed anemia. This could also explain why only arthroplasty was associated with increased postoperative mortality if performed out-of-hours. Arthroplasties are generally more complex and time-consuming procedures with larger blood losses, compared to internal fixation procedures, which might increase the risk of early acute postoperative complications [55].
This study has several significant strengths, such as the large longitudinal sample size, including 10 consecutive years of data from the Swedish National Quality Registry for Hip Fracture Patients, with a high case coverage between 80 and 90% [56], as well as the ability to adjust for a multitude of confounding factors. Nevertheless, the usual limitations of a retrospective administrative dataset apply. We were therefore unable adjust for the type of anesthesia used or other intraoperative variables. We also did not have any access to data regarding the duration of the surgical procedures, the rationale for patient-level decisions regarding operative timing, or the individual surgeon’s experience; however, these are unlikely significant cofounders [21, 45,46,47,48,49].
Conclusion
Out-of-hours surgical intervention is associated with an increase in both 30- and 90-day postoperative mortality among hip fracture patients who received an arthroplasty, while no such association could be detected among patients who underwent internal fixation. Accordingly, procedures involving arthroplasty should likely be avoided out-of-hours, while internal fixation can be considered and performed around the clock if not contraindicated by patient characteristics and when adequate resources exist.
Availability of data and material
All data are available for retrieval upon reasonable request.
Code availability
Codes are available for retrieval upon reasonable request.
References
Nyholm AM, Gromov K, Palm H, Brix M, Kallemose T, Troelsen A, et al. Time to surgery is associated with thirty-day and ninety-day mortality after proximal femoral fracture: a retrospective observational study on prospectively collected data from the Danish fracture database collaborators. J Bone Jt Surg Am. 2015;97:1333–9.
Bretherton CP, Parker MJ. Early surgery for patients with a fracture of the hip decreases 30-day mortality. Bone Jt J. 2015;97-B:104–8.
Colais P, Di Martino M, Fusco D, Perucci CA, Davoli M. The effect of early surgery after hip fracture on 1-year mortality. BMC Geriatr. 2015;15:141.
Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, Debeer J, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ Can Med Assoc J J Assoc Medicale Can. 2010;182:1609–16.
Choi HJ, Kim E, Shin YJ, Choi BY, Kim YH, Lim TH. The timing of surgery and mortality in elderly hip fractures: a retrospective, multicenteric cohort study. Indian J Orthop. 2014;48:599–604.
HIP Attack Investigators. Accelerated surgery versus standard care in hip fracture (HIP ATTACK): an international, randomised, controlled trial. Lancet Lond Engl. 2020;395:698–708.
Ly TV, Swiontkowski MF. Management of femoral neck fractures in young adults. Indian J Orthop. 2008;42:3–12.
Dedrick DK, Mackenzie JR, Burney RE. Complications of femoral neck fracture in young adults. J Trauma. 1986;26:932–7.
Sendtner E, Renkawitz T, Kramny P, Wenzl M, Grifka J. Fractured neck of femur—internal fixation versus arthroplasty. Dtsch Ärztebl Int. 2010;107:401–7.
Ikpeze TC, Mohney S, Elfar JC. Initial preoperative management of geriatric hip fractures. Geriatr Orthop Surg Rehabil. 2017;8:64–6.
Greve K, Modig K, Talbäck M, Bartha E, Hedström M. No association between waiting time to surgery and mortality for healthier patients with hip fracture: a nationwide Swedish cohort of 59,675 patients. Acta Orthop. 2020;91:396–400.
NCEPOD—who operates when? II (2003) [Internet]. [cited 2021 Apr 29]. https://www.ncepod.org.uk/2003wow.html.
Separating Emergency and Elective Surgical Care: Recommendations for practice [Internet]. R. Coll. Surg. [cited 2021 Apr 29]. https://www.rcseng.ac.uk/library-and-publications/rcs-publications/docs/seperating-emergency-and-elective/.
Lans A, Janssen SJ, Ring D. Off-hour surgery among orthopedic subspecialties at an urban, quaternary-care, level 1 trauma center. J Hand Surg. 2016;41:1153–8.
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2012;23:2239–56.
Lancet T. Ageing well: a global priority. Lancet. 2012;379:1274.
Rikshoft Arsrapport 2018 [Internet]. Lund, Sweden: Rikshoft; 2018. Report No.: 18. https://www.xn--rikshft-e1a.se/forsking-och-utv%C3%A4rdering.
Gundel O, Thygesen LC, Gögenur I, Ekeloef S. Postoperative mortality after a hip fracture over a 15-year period in Denmark: a national register study. Acta Orthop. 2020;91:58–62.
Williamson S, Landeiro F, McConnell T, Fulford-Smith L, Javaid MK, Judge A, et al. Costs of fragility hip fractures globally: a systematic review and meta-regression analysis. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2017;28:2791–800.
Choi HG, Lee YB, Rhyu SH, Kwon BC, Lee JK. Mortality and cause of death postoperatively in patients with a hip fracture: a national cohort longitudinal follow-up study. Bone Jt J. 2018;100-B:436–42.
Ahl R, Mohammad Ismail A, Borg T, Sjölin G, Forssten MP, Cao Y, et al. A nationwide observational cohort study of the relationship between beta-blockade and survival after hip fracture surgery. Eur J Trauma Emerg Surg Off Publ Eur Trauma Soc. 2021.https://doi.org/10.1007/s00068-020-01588-7
deMeireles AJ, Gerhardinger L, Oliphant BW, Jenkins PC, Cain-Nielsen AH, Scott JW, et al. Factors associated with optimal patient outcomes after operative repair of isolated hip fractures in the elderly. Trauma Surg Acute Care Open [Internet]. 2020 [cited 2021 Apr 20];5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7757513/.
Forssten MP, Mohammad Ismail A, Sjolin G, Ahl R, Wretenberg P, Borg T, et al. The association between the Revised Cardiac Risk Index and short-term mortality after hip fracture surgery. Eur J Trauma Emerg Surg Off Publ Eur Trauma Soc. 2020.https://doi.org/10.1007/s00068-020-01488-w
Forssten MP, Ismail AM, Borg T, Ahl R, Wretenberg P, Cao Y, et al. Postoperative mortality in hip fracture patients stratified by the Revised Cardiac Risk Index: a Swedish nationwide retrospective cohort study. Trauma Surg Acute Care Open. 2021;6:e000778.
Kates SL. Hip fracture programs: are they effective? Injury. 2016;47(Suppl 1):S25-27.
Halvachizadeh S, Teuber H, Cinelli P, Allemann F, Pape H-C, Neuhaus V. Does the time of day in orthopedic trauma surgery affect mortality and complication rates? Patient Saf Surg [Internet]. 2019 [cited 2021 Apr 15];13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6362600/.
Rashid RH, Zubairi AJ, Slote MU, Noordin S. Hip fracture surgery: does time of the day matter? A case-controlled study Int J Surg. 2013;11:923–5.
Chacko AT, Ramirez MA, Ramappa AJ, Richardson LC, Appleton PT, Rodriguez EK. Does late night hip surgery affect outcome? J Trauma. 2011;71:447–53 (discussion 453).
Switzer JA, Bennett RE, Wright DM, Vang S, Anderson CP, Vlasak AJ, et al. Surgical time of day does not affect outcome following hip fracture fixation. Geriatr Orthop Surg Rehabil. 2013;4:109–16.
Barinaga G, Wright E, Cagle PJJ, Anoushiravani AA, Sayeed Z, Chambers MC, et al. Effect of time of operation on hip fracture outcomes: a retrospective analysis. JAAOS J Am Acad Orthop Surg. 2017;25:55–60.
Nijland LMG, Karres J, Simons AE, Ultee JM, Kerkhoffs GMMJ, Vrouenraets BC. The weekend effect for hip fracture surgery. Injury. 2017;48:1536–41.
Chan YM, Tang N, Chow SK. Surgical outcome of daytime and out-of-hours surgery for elderly patients with hip fracture. Hong Kong Med J Xianggang Yi Xue Za Zhi. 2018;24:32–7.
Bosma E, de Jongh MAC, Verhofstad MHJ. Operative treatment of patients with pertrochanteric femoral fractures outside working hours is not associated with a higher incidence of complications or higher mortality. J Bone Jt Surg Br. 2010;92:110–5.
Pincus D, Desai SJ, Wasserstein D, Ravi B, Paterson JM, Henry P, et al. Outcomes of after-hours hip fracture surgery. JBJS. 2017;99:914–22.
WMA - The World Medical Association-WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects [Internet]. [cited 2020 Sep 21]. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/.
Om Rikshöft – RIKSHÖFT [Internet]. [cited 2021 Apr 20]. https://www.xn--rikshft-e1a.se/om-oss.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
R Development Core Team. R: A Language and Environment for Statistical Computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2008. http://www.R-project.org/.
Olasky J, Chellali A, Sankaranarayanan G, Zhang L, Miller A, De S, et al. Effects of sleep hours and fatigue on performance in laparoscopic surgery simulators. Surg Endosc. 2014;28:2564–8.
Reijmerink I, Thé A-F, Gloudemans B, Klaassen A, Cnossen F, van der Laan M. The effects of mental fatigue on surgical performance: a systematic review. Eur J Vasc Endovasc Surg. 2019;58:e801–2.
Sturm L, Dawson D, Vaughan R, Hewett P, Hill AG, Graham JC, et al. Effects of fatigue on surgeon performance and surgical outcomes: a systematic review. ANZ J Surg. 2011;81:502–9.
Yaghoubian A, Kaji AH, Putnam B, de Virgilio C. Trauma surgery performed by “sleep deprived” residents: are outcomes affected? J Surg Educ. 2010;67:449–51.
McCormick F, Kadzielski J, Landrigan CP, Evans B, Herndon JH, Rubash HE. Surgeon fatigue: a prospective analysis of the incidence, risk, and intervals of predicted fatigue-related impairment in residents. Arch Surg Chic Ill. 1960;2012(147):430–5.
Rothschild JM, Keohane CA, Rogers S, Gardner R, Lipsitz SR, Salzberg CA, et al. Risks of complications by attending physicians after performing nighttime procedures. JAMA. 2009;302:1565–72.
Ioannidis I, Mohammad Ismail A, Forssten MP, Ahl R, Cao Y, Borg T, et al. The mortality burden in patients with hip fractures and dementia. Eur J Trauma Emerg Surg Off Publ Eur Trauma Soc. 2021.https://doi.org/10.1007/s00068-021-01612-4
Groff H, Kheir MM, George J, Azboy I, Higuera CA, Parvizi J. Causes of in-hospital mortality after hip fractures in the elderly. Hip Int J Clin Exp Res Hip Pathol Ther. 2020;30:204–9.
Foss NB, Kehlet H. Mortality analysis in hip fracture patients: implications for design of future outcome trials. BJA Br J Anaesth. 2005;94:24–9.
Sheikh HQ, Hossain FS, Aqil A, Akinbamijo B, Mushtaq V, Kapoor H. A comprehensive analysis of the causes and predictors of 30-day mortality following hip fracture surgery. Clin Orthop Surg. 2017;9:10–8.
Guan G, Cheng Z, Yin J, Hu Q, Zhang W, Liu X, et al. Daytime versus after-hours surgery outcomes in hip fracture patients: a systematic review and meta-analysis. Aging Clin Exp Res. 2020;32:2427–38.
Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. BMJ. 1993;307:1248–50.
Fox KM, Magaziner J, Hebel JR, Kenzora JE, Kashnei TM. Intertrochanteric versus femoral neck hip fractures: differential characteristics, treatment, and sequelae. J Gerontol Ser A. 1999;54:M635–40.
Karagiannis A, Papakitsou E, Dretakis K, Galanos A, Megas P, Lambiris E, et al. Mortality rates of patients with a hip fracture in a southwestern district of Greece: ten-year follow-up with reference to the type of fracture. Calcif Tissue Int. 2006;78:72–7.
Meunier A, Maczynski A, Asgassou S, Baulot E, Manckoundia P, Martz P. Mortality and functional independence one year after hip fracture surgery: extracapsular fracture versus intracapsular fracture]. Geriatr Psychol Neuropsychiatr Vieil. 2019;17:153–62.
Sund R, Riihimäki J, Mäkelä M, Vehtari A, Lüthje P, Huusko T, et al. Modeling the length of the care episode after hip fracture: does the type of fracture matter? Scand J Surg. 2009;98:169–74.
Parker MJ, Pryor GA. Internal fixation or arthroplasty for displaced cervical hip fractures in the elderly: a randomised controlled trial of 208 patients. Acta Orthop Scand. 2000;71:440–6.
Meyer AC, Hedström M, Modig K. The Swedish Hip Fracture Register and National Patient Register were valuable for research on hip fractures: comparison of two registers. J Clin Epidemiol. 2020;125:91–9.
Funding
Open access funding provided by Örebro University. The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was approved by the Swedish Ethical Review Authority (ref: 2020-03257).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Forssten, M.P., Mohammad Ismail, A., Borg, T. et al. The consequences of out-of-hours hip fracture surgery: insights from a retrospective nationwide study. Eur J Trauma Emerg Surg 48, 709–719 (2022). https://doi.org/10.1007/s00068-021-01804-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01804-y