Abstract
Purpose
The position of the wrist during cast immobilisation following closed reduction of distal radius fractures is disputed. A systematic review was initiated to assess if there was any relation between wrist position in the cast and outcome in adult patients with non-operatively treated distal radius fractures.
Methods
A comprehensive search was performed in the bibliographic databases Medline, Embase and Wiley/Cochrane Library from inception up to 27 November 2020. Eligible studies were: randomised controlled trials, prospective and retrospective comparative cohort studies, analysing different positions of the wrist in cast-immobilisation following closed reduction. Primary outcome of the study was functional outcome measured by range of motion. Secondary outcomes were functional outcomes measured by grip strength, patient-reported outcome, radiological outcome and complications such as secondary dislocation and pain.
Results
The initial search yielded 2733 studies. Five trials, with 519 patients, were included in this systematic review. Range of motion and radiological outcome was significantly better in patients who were immobilised in dorsiflexion compared to palmar flexion or neutral position, although no clinical important difference was found. There were no significant differences in patient-reported outcome, pain, grip strength or complications. Due to heterogeneity of the included studies, data were unsuitable for a meta-analysis.
Conclusion
This systematic review showed statistically significant better results in favour of cast immobilisation in dorsiflexion, although this small difference does not seem to be relevant in patients daily activities.
Systematic review registration number
Systematic review registration number: PROSPERO 2018 CRD42018085546.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nearly 20% of all fractures are distal radius fractures (DRFs) [1]. Most of these fractures are treated non-operatively with closed reduction and cast immobilisation.
Previous studies have shown no superiority of above-elbow casts compared to lower forearm casts [2,3,4]. However, the best position of the wrist in lower forearm casts, remains controversial. Some authors believe that dorsiflexion (DF) of the wrist prevents fracture displacement since DF balances the forces of the radial extensors and flexors best [5,6,7]. Some conclude that pronation is more effective in retaining the reduction, others state that supination prevents fracture displacement [8,9,10,11].
The Cochrane review “Conservative interventions for treating distal radial fractures in adults” [12], analysed six articles comparing different wrist positions during cast immobilisation and showed no significant difference in clinical, functional or anatomical outcome [7, 11, 13]. Since then, three new trials were published that compared DF to palmar flexion (PF) or neutral position (NP) [6, 14, 15]. No new trials on supination were published after 1990.
The aim of this systematic review was to assess if there is any relation between wrist position in the cast and outcome in adult patients with non-operatively treated DRFs.
Materials and methods
A review protocol (PROSPERO 2018 CRD42018085546) was developed based on the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” statement [16].
A comprehensive search was performed in the bibliographic databases Medline, Embase and Wiley/Cochrane Library from inception up to 27 November 2020, in collaboration with a medical librarian. The following terms were used (including synonyms and closely related words) as index terms or free-text words: “Conservative Treatment”, “Non-operative”, “Casts”, “Radius Fractures”, “Adults”. The search was performed without date or language restriction. After deduplication all titles were screened and appropriate abstracts reviewed. Also, a manual reference check of the identified systematic reviews and meta-analyses was executed. The full search strategies for all databases can be found in the supplementary Information. After deduplication, all titles and abstracts were screened independently by two reviewers (ED, TG).
Eligible criteria
Randomised controlled trials, prospective and retrospective comparative cohort studies comparing different positions of the wrist during cast immobilisation of displaced and reduced DRFs in adults were included in this study. Studies had to report on patient-reported, functional or radiological outcome. Studies were included if they compared wrist immobilisation in DF versus PF or NP and had to define the position of the wrist during cast-immobilisation, which had to be at least 15° of DF or PF. If studies contained other fractures than DRFs, or if the studies concerned paediatric fractures or open fractures, they were excluded. All prospective and randomized studies comparing supination, pronation and ulnar deviation (UD) have been published before 1990 and were discussed in the Cochrane review published in 2003, in which it was concluded that these positions had no influence on outcome [12]. Therefore these studies were excluded from this systematic review and only studies comparing DF to PF or NP were included in the present study. Data extracted from the studies included patient demographics, fracture classifications, duration of wrist immobilisation and the number and type of complications. Restrictions on language of publication were not imposed. In case of disagreements, independent judgement of a third author (FB) was initiated.
Outcome measures
Primary outcome of the study was functional outcome measured by range of motion. Secondary outcomes were functional outcomes measured by grip strength, patient-reported outcome, radiological outcome and complications such as pain and secondary dislocation.
Functional outcome included range of motion or loss of range of motion, measured in degrees. Grip strength was defined by pressure measured with a dynamometer and expressed in kilograms, mmHg or as a percentage value of the uninjured side.
Patient-reported outcome measures had to be presented in validated questionnaires. Appropriate questionnaires were the Disability of Arm, Shoulder and Hand score (DASH), the Patient Reporting Wrist Evaluation score (PRWE) and the SF-12 Healthy Survey. The PRWE and DASH questionnaires both result in a score between 0 and 100, bases on solely subjective outcomes; 0 is the best possible outcome and 100 is the worst [17, 18]. The SF-12 is a short version of the SF-36 Health Survey, reporting on physical and mental health on a 12-point scale [19, 20]. The Modified Demerit Score and the Sarmiento Score were also qualified. These are scoring systems combining both objective and subjective patient factors as disability, pain, stiffness, range of motion, grip strength and complications as arthritis and nerve dysfunction. The patient-reported outcome is expressed as poor, fair, good or excellent [21].
Radiological outcome was assessed by measuring radial height or radial shortening, dorsal tilt, volar tilt and ulnar variance. Additionally, the Lidström-score was used to determine displacement in a severe, moderate, small or insignificant rating based on the severity of radial shortening, dorsal tilt, and loss of radial inclination [22].
Statistical significance will be analysed, as well as the minimal clinically important difference (MCID). This is the smallest change in outcome that could be identified by an individual patient during daily activities and exercise [23,24,25].
Risk of bias assessment and quality scoring
The Cochrane Risk of Bias Tool was used to assess the Risk of Bias (RoB). This tool reflects on seven types of bias. A judgement is made whether the article is at ‘Low’ risk, ‘High’ risk, or ‘Unclear’ risk of bias. If a study fulfilled four or more criteria it was considered as low RoB. Analysis of performance bias was disregarded in this systematic review, because blinding for position of the cast was inapplicable. To give authors the opportunity to provide feedback, attempt was made to contact the authors with the RoB assessment. Although, no attempt was made to contact authors for publications before the year 2000.
Statistical methods
Review Manager software, version 5.3, Cochrane Collaboration, London, UK, was used to carry out the statistical analysis. Population and study protocol were reviewed to determine clinical homogeneity. Statistical homogeneity was determined by use of the I2 test, visual inspection of forest plots and by use of the Q-test. An I2 test with values less than 40% and a Q-test with p < 0.05 was considered to present no significant heterogeneity. Whenever possible, data will be pooled to perform a quantitative analysis.
Results
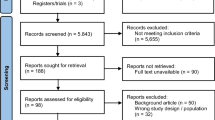
The primary selection of articles resulted in 146 eligible articles. 141 Articles were excluded, as shown in Fig. 1 [16]. Five articles comparing DF to PF or NP were analysed in this systematic review, including 519 patients (Table 1). There were 348 females, mean age: 56 years. 209 patients were treated in DF, 195 in PF and 115 in NP.
Primary outcome
Functional outcome measured by range of motion was analysed in three studies (Table 2) [6, 8, 15]. All three studies showed statistically significant differences in range of motion in favour of patients immobilised in DF.
Secondary outcome
Four studies compared grip strength (Table 3) [6, 8, 14, 15]. Grip strength was significant better in one study favouring DF [15].
The patient-reported outcome was measured in only two studies (Table 4) [6, 14]. The study of Grle reported significant better SF-12 scores in favor of immobilisation in DF [6].
Three studies determined outcome by use of a combination of patient-reported and functional outcome: the Modified Demerit Score and the Sarmiento Score, of which two reported significant better outcome in favor of immobilisation in DF (Table 5) [7, 8, 15].
All five studies reported on radiological outcome [6,7,8, 14, 15]. The studies of Grafstein and Gupta did not report significant difference in radiological outcome [7, 14]. Three studies reported an overall statistically significantly better radiological outcome in patients treated in DF (Table 6) [6, 8, 15].
Complications were reported in three studies [6, 14, 15]. Only 1 study described an overall rate of secondary displacement of 22% (n = 22), of which 17 were treated operatively. The difference in secondary displacement between DF (n = 5), PF (n = 8) and NP (n = 9) was not significant (p = 0.17) [14].
Pain was described in two studies [6, 14]. One study reported significant decrease in pain in the patients treated in DF compared with immobilisation in PF [6]. Persistent pain at 6-month follow-up was reported in one patient in each group [14].
One study described carpal tunnel syndrome in two patients, one in the DF group, one in the NP group [14]. Another study described an increased rate of Complex Regional Pain Syndrome (Morbus Sudeck) in the DF group comparing to the PF group, however the number of patients suffering from complications, neither the significance was reported [6]. The third study reported three patients with complaints of stiffness in the PF group, yet none of the patients showed complaints at the final follow-up [15].
Risk of bias within studies
Using the Cochrane Risk of Bias Tool, one study was qualified as low-risk study, one as high-risk study and in three of the studies the risk of bias was unclear (Table 1; Fig. 2).
Discussion
A systematic review was initiated to assess the optimal position of the wrist during cast immobilisation in patients with non-operatively treated DRFs.
Our review showed that patients treated with cast immobilisation in DF had a range of motion or radiological outcome that was statistically significantly better according to patients who were immobilised in PF or NP. Nevertheless, the clinical relevance of this statistical difference is limited. Grip strength, patient-reported outcome, or rate of complications were not statistically different between the different positions of cast-immobilisation.
Differences found in our study were small, and despite significant results were found, the results were too small to reach minimal clinically important difference (MCID). This is the smallest change in outcome that could be identified by an individual patient during daily activities and exercise [26,27,28]. Unlike patient-reported outcome measures as the DASH and PRWE, and grip strength, the MCID could not be determined for radiological parameters or range of motion. Nevertheless, differences in radiological outcome and range of motion found in this study were that small that clinical importance is assumed to be negligible.
The results of this review were limited by the risk of bias in studies and the strength of available evidence. Studies used non-validated measurements to report their outcome. Grip strength should be reported as a percentage of the unaffected side [29]. Also, the Modified Demerit Score and Sarmiento score are, in contrast to the DASH and PRWE, not validated instruments. To report pain, by example, not all studies used the validated VAS-score [30, 31]. Most of the included studies presented their results without describing mean values or standard deviations, resulting in data that could not be pooled to perform a quantitative analysis by meta-analysis.
Also, studies did not use a standardized follow-up period. The follow-up period in the study of Grle was only 2 months. Plausibly, grip strength and range of motion will improve further after this period of time [6].
Besides the use of different, non-validated, measuring tools, there was no homogeneity in fracture types too. The studies included in this review analysed both intra and extra articular DRF. No subgroup analysis bases on fracture type were performed in any of the studies. One can presume that patients with a more comminuted fracture will have a worse anatomical and functional outcome compared to a simple fracture.
To draw clear conclusions on the best position of immobilisation in DRFs, future studies should use homogeneous patient data and validated outcome measures and report standard deviations to enable quantitative analysis.
This systematic review showed statistically significant better results in favour of cast immobilisation in dorsiflexion, although these differences are too small to be noticed for patients during their daily activities.
References
Court-Brown CM, Ceasar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–7.
Bong MR, Egol KA, Leibman M, Koval KJ. A comparison of immediate postreduction splinting constructs for controlling initial displacement of fractures of the distal radius: a prospective randomized study of long-arm versus short-arm splinting. J Hand Surg Am. 2006;31(5):766–70.
Diaz-Garcia RJ, Chung KC. Common myths and evidence in the management of distal radius fractures. Hand Clin. 2012;28(2):127–33.
Pool C. Colles’s fracture. A prospective study of treatment. J Bone Jt Surg Br. 1973;55(3):540–4.
Baruah RK, Islam M, Haque R. Immobilisation of extra-articular distal radius fractures (Colles type) in dorsiflexion: the functional and anatomical outcome. J Clin Orthop Trauma. 2015;6(3):167–72.
Grle M, Miljko M, Grle I, Hodžić F, Kapidžić T. Early results of the conservative treatment of distal radius fractures-immobilization of the wrist in dorsal versus palmar flexion. Med Glas. 2017;14(2):236–43.
Gupta A. The treatment of Colles’ fracture. Immobilisation with the wrist dorsiflexed. J Bone Jt Surg Br. 1991;73(2):312–5.
Blatter G, Papp P, Magerl F. Comparative study of two methods of plaster cast fixation in the treatment of Colles’ fracture. A prospective randomized study. Unfallchirurg. 1994;97(10):534–40.
Gibson AGF, Bannister GC. Bracing or plaster for Colles’ fractures? A randomised prospective controlled trial. J Bone Jt Surg Br. 1983;65(2):221.
van der Linden W, Ericson R. Colles’ fracture. How should its displacement be measured and how should it be immobilized? J Bone Jt Surg Am. 1981;63(8):1285–8.
Wahlström O. Treatment of Colles’ fracture. A prospective comparison of three different positions of immobilization. Acta Orthop Scand. 1982;53(2):225–8.
Handoll HHG, Madhok R. Conservative interventions for treating distal radial fractures in adults (review). Cochrane Database Syst Rev. 2003;2:CD000314.
Wilson C, Venner RM. Colles’ fracture. Immobilisation in pronation or supination? J R Coll Surg Edinb. 1984;29(2):109–11.
Grafstein E, Stenstrom R, Christenson J, Innes G, MacCormack R, Jackson C, Stothers K, Goetz T. A prospective randomized controlled trial comparing circumferential casting and splinting in displaced Colles fractures. Can J Emerg Med. 2010;12(3):192–200.
Rajan S, Jain S, Ray A, Bhargava P. Radiological and functional outcome in extra-articular fractures of lower end radius treated conservatively with respect to its position of immobilization. Indian J Orthop. 2008;42(2):201–7.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4(11):1–6.
MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577–86.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). Med Care. 1992;30(6):473–83.
Ware JE Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Sarmiento A, Pratt GW, Berry NC, Sinclair WF. Colles’ fractures: functional bracing in supination. J Bone Jt Surg Am. 1975;57(3):311–7.
Lidström A. Fractures of the distal end of the radius: a clinical and statistical study of end results. Acta Orthop Scand. 1959;30:1–118.
Calfee RP, Adams AA. Clinical research and patient-rated outcome measures in hand surgery. J Hand Surg Am. 2012;37:851–5.
Jaeschke R, Singer J, Guyatt GH. Measurement of health status: ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–15.
Smith MV, Calfee RP, Baumgarten KM, Brophy RH, Wright RW. Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Jt Surg Am. 2012;94:277–85.
Walenkamp MM, de Muinck Keizer RJ, Goslings JC, Vos LM, Rosenwasser MP, Schep NWL. The minimum clinically important difference of the patient-rated wrist evaluation score for patients with distal radius fractures. Clin Orthop Relat Res. 2015;473(10):3235–41.
Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther. 2014;44(1):30–9.
Bohannon RW. Minimal clinically important difference for grip strength: a systematic review. J Phys Ther Sci. 2019;1:75–8.
Wadsten MÅ, Sjödén GO, Buttazzoni GG, Buttazzoni C, Englund E, Sayed-Noor AS. The influence of late displacement in distal radius fractures on function, grip strength, range of motion and quality of life. J Hand Surg EU. 2018;43(2):131–6.
Bijur PE, Silver W, Gallagher J. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. 2001;8(12):1153–7.
Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37(4):378–81.
Acknowledgements
The authors would like to thank Mr. Ralph de Vries for his help during the bibliographic literature search. This research was conducted as part of the research program of Amsterdam Movement Sciences.
Funding
No funding was received to perform this study.
Author information
Authors and Affiliations
Contributions
All authors participated in the design of the study and the drafting of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Ethical approval
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Delft, E.A.K., van Gelder, T.G., Vermeulen, J. et al. Does position of the wrist during cast immobilisation in patients with distal radius fractures affect outcome?. Eur J Trauma Emerg Surg 48, 1751–1757 (2022). https://doi.org/10.1007/s00068-021-01751-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01751-8