Abstract
Background
The effects of immediate operation on hip fracture (HF) are unclear. Therefore, we investigated the influence of time to operation within 12 h vs. > 12–24 h on survival and adverse events.
Methods
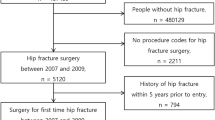
This retrospective study was based on our database from 2006 to 2019. Patients ≥ 20 years of age with operations for HF were included. A total of 40 characteristics were analyzed for operations within 12 h (group 1) and > 12–24 h (group 2) after admission. The primary endpoint was survival at 1 year after operation. Secondary endpoints were revision surgery for any reason, infection, and serious adverse events.
Results
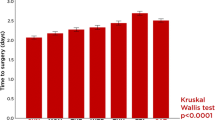
A total of 1015 patients received operations within 12 h (group 1), and 985 patients received operations > 12–24 h (group 2) after admission. The mean age of the patients was 78.8 ± 12.3 years. Patients in group 1 were younger and had better health status and shorter hospitalizations than those in group 2. However, no differences were found for revision surgery, infection or adverse events. The mortality rates at 30 days, 90 days, 6 months, and 1 year were 6.2, 11.8, 15.9, and 21.0%, respectively. The mortality rate at day 30 was significantly better (p = 0.04) in group 1, but no further differences in survival were observed (hazard ratio 1.071; 95% confidence interval 0.864–1.328; log rank 0.179). A subgroup analysis of geriatric patients ≥ 65 years assessed no differences according the primary and secondary endpoints.
Conclusions
Within the limits of single-center analysis, the patients receiving treatment for HF within 12 h were younger and healthier and had the benefits of shorter hospitalizations and a higher 30-day survival rate than patients treated > 12–24 h after admission. At the endpoint 1 year after operation, no differences were observed in adverse events or survival rates.



Similar content being viewed by others
References
No authors listed. Hip fractures in adults. Timing of surgery. National Institute for Health and Care Excellence (NICE). Last updated May 2017. www.nice.org.uk.
No authors listed. Canadian Institute for Health Information. Wait times for priority procedures in Canada. Last updated March 2020. www.waittimes.chih.ca.
Bonnaire F, Weber A. Hip fractures in adults. S2 Guideline. German Society for Trauma Surgery e.V. (DGU). Last updated October 2015. www.awmf.org.
Leer-Salvesen S, Engesæter LB, Dybvik E, Furnes O, Kristensen TB, Gjertsen JE. Does time from fracture to surgery affect mortality and intraoperative medical complications for hip fracture patients? An observational study of 73557 patients reported to the Norwegian Hip Fracture register. Bone Joint J. 2019;101:1129–37. https://doi.org/10.1302/0301-620X.101B9.BJJ-2019-0295.R1.
Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–54. https://doi.org/10.1007/BF03016088.
Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JN, Nathens AB, Kreder HJ, Jenkinson RJ, Wodchis WP. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318:1994–2003. https://doi.org/10.1001/jama.2017.17606.
Pollmann CT, Røtterud JH, Gjertsen JE, Dahl FA, Lenvik O, Årøen A. Fast track hip fracture care and mortality—an observational study of 2230 patients. BMC. 2019;20:248. https://doi.org/10.1186/s12891-019-2637-6.
Aldrete JA, Hamilton SD, Hingson RA. Anesthesia factors in the surgical management of hip fractures. J Trauma. 1976;7:818–26. https://doi.org/10.1097/00005373-196711000-00003.
Bretherton CP, Parker MJ. Early surgery for patients with a fracture of the hip decrease 30-day mortality. Bone Joint J. 2015;97:104–8. https://doi.org/10.1302/0301/620X.97B1.35041.
American Society of Anesthesiologists. New classification of physical status. Anesthesiology. 1963;24:111–4.
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and dislocation classification compendium—2007: orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(Suppl 10):S1–133. https://doi.org/10.1097/00005131-200711101-00001.
Workgroup Convened by the Musculoskeletal Infection Society. New definition for periprosthetic joint infection. J Arthroplasty. 2011;2011(26):1136–8. https://doi.org/10.1016/j.arth.2011.09.026.
No authors listed. Center for Disease Control and Prevention. Hip fractures among older adults. Last updated September 2016. www.cdc.gov.
Müller-Mai CM, Schulze Raestrup US, Kostuj T, Dahlhoff G, Günster C, Smektala R. One-year outcomes for proximal femoral fractures: posthospital analysis of mortality and care levels based on health insurance data. Unfallchirurg. 2015;118:780–94. https://doi.org/10.1007/s00113-013-2534-7.
Bredahl C, Nyholm B, Hindsholm KB, Mortensen JS, Olesen AS. Mortality after hip fracture: results of operation within 12 h of admission. Injury. 1992;23:83–6. https://doi.org/10.1016/0020-1383(92)90037-s.
Dorotka R, Schoechtner H, Buchinger W. The influence of immediate surgical treatment of proximal femoral fractures on mortality and quality of life. Operation within six hours of the fracture versus later than six hours. J Bone Joint Surg Br. 2003;85:1107–13. https://doi.org/10.1302/0302/0301-620x.85b8.14282.
Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44:726–9. https://doi.org/10.1016/j.injury.2012.08.025.
Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87:1123–6. https://doi.org/10.1302/0301-620X.87B8.16357.
Hongisto MT, Nuotio MS, Luukkaala T, Väistö O, Pihlajamäki HK. Delay to surgery of less than 12 hours is associated with improved short- and long-term survival in moderate- to high-risk hip fracture patients. Geriatr Orthop Surg Rehabil. 2019. https://doi.org/10.1177/2151459319853142.
Weller I, Wai EK, Jaglal S, Kreder HJ. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005;87:361–6. https://doi.org/10.1302/0301-620x.87b3.15300.
Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M, McLaughlin M, Halm EA, Wang JJ, Litke A, Silberzweig SB, Siu AL. Association of timing of surgery for hip fracture and patient outcome. JAMA. 2004;291:1738–43. https://doi.org/10.1001/jama.291.14.1738.
Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important. J Bone Joint Surg Am. 2005;87:483–9. https://doi.org/10.2106/JBJS.D.01796.
Verbeek DOF, Ponsen KJ, Goslings JC, Heetveld MJ. Effect of surgical delay on outcome in hip fracture patients: a retrospective multivariate analysis of 192 patients. Int Orthop. 2008;32:13–8. https://doi.org/10.1007/s00264-006-0290-9.
Funding
The research did not receive any specific Grant from funding agencies in the public, commercial or no-profit sectors.
Author information
Authors and Affiliations
Contributions
We would like to thank Dr. med. Tanja Kottmann, Medical Statistics, Beverstr. 64, 59,077 Hamm, Germany, for doing the statistical analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval was obtained by the institutional review board.
Consent to participate
All patients or their next relatives gave consent to participate in this study.
Rights and permissions
About this article
Cite this article
Müller, F., Proske, A., Eckstein, C. et al. Two-thousand hip fractures treated within 12 h and > 12–24 h after admission: Are survival and adverse events affected?. Eur J Trauma Emerg Surg 48, 1817–1825 (2022). https://doi.org/10.1007/s00068-021-01697-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01697-x