Abstract
Purpose
The role of classification systems for the choice of surgical approach and the management of tibial plateau fractures remains unclear. The purpose of this study was to investigate the potential of classification systems to choose the appropriate operative approach. Current surgical management strategies were investigated in a large multicenter assessment.
Methods
In this study, we retrospectively analyzed all patients with tibial plateau fractures that have received surgical treatment in one of the five Level I trauma facilities between 2012 and 2015. Fractures were classified in each center by a senior orthopedic surgeon using the AO/OTA and the Luo classification. Demographics, trauma mechanism, as well as the surgical approach were recorded.
Results
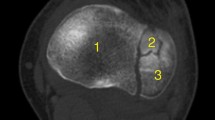
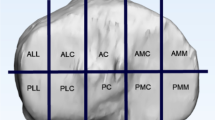
538 patients (46.1% male, 53.9% female) were included. The anterolateral approach was used most frequently with 54.8% of all single approaches; 76.2% of all combined approaches used anterolateral as part of the approach. Combined approaches were used in 22.5% of the cases; a combination of the anterolateral and medial (10%), anterolateral, and posteromedial approach (5.8%) were used most frequently. The lowest number was found for the posterolateral (1.3%) and the combined approaches dorsal/anterolateral and medial/dorsal (1.7%, 1.1%). The AO/OTA classification showed a peak for 41.B2 (21.9%) and B3 (35.5%) fractures. Regarding the Luo classification, the dorsal column was involved in 45.7%. In contrast, only 14.7% of the surgical approaches used were able to address the dorsal tibial plateau potentially.
Conclusion
The use of dorsal approach seems to be of minor importance than expected in daily clinical practice in this multicenter study. It was not possible to specify whether the AO/OTA or the Luo classification can reliably predict the choice of surgical approach. The operative treatment strategy of tibial plateau fractures seems to rather rely on the surgeons' experience, education, and preferences.






Similar content being viewed by others
References
Kokkalis ZT, Iliopoulos ID, Pantazis C, Panagiotopoulos E. What's new in the management of complex tibial plateau fractures? Injury. 2016;47:1162–9.
Jacofsky D. Haidukerwych G Tibia plateau fractures. In: Scott W, editor. Insall & Scott surgery of the knee. Philadelphia: Churchill Livingstone; 2006. p. 1133–1146.
Wang Y, Luo C, Zhu Y, Zhai Q, Zhan Y, Qiu W, Xu Y. Updated three-column concept in surgical treatment for tibial plateau fractures—a prospective cohort study of 287 patients. Injury. 2016;47:1488–96.
Millar SC, Arnold JB, Thewlis D, Fraysse F, Solomon L. A systematic literature review of tibial plateau fractures: what classifications are used and how reliable and useful are they? Injury. 2018;49:473–90.
Castiglia MT, Nogueira-Barbosa MH, Messias AMV, Salim R, Fogagnolo F, Schatzker J, Kfuri M. The impact of computed tomography on decision making in tibial plateau fractures. J Knee Surg. 2018;31:1007–144.
Taşkesen A, Demirkale İ, Okkaoğlu MC, Özdemir M, Bilgili MG, Altay M. Intraobserver, and interobserver reliability assessment of tibial plateau fracture classification systems. Eklem Hastalik Cerrahisi. 2017;28:177–81.
Krause M, Preiss A, Müller G, Madert J, Fehske K, Neumann MV, Domnick C, Raschke M, Südkamp N, Frosch KH. Intra-articular tibial plateau fracture characteristics according to the "Ten segment classification". Injury. 2016;47:2551–7.
Yang G, Zhai Q, Zhu Y, Sun H, Putnis S, Luo C. The incidence of posterior tibial plateau fracture: an investigation of 525 fractures by using a CT-based classification system. Arch Orthop Trauma Surg. 2013;133:929–34.
Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24:683–92.
Gicquel T, Najihi N, Vendeuvre T, Teyssedou S, Gayet LE, Huten D. Tibial plateau fractures: reproducibility of three classifications (Schatzker, AO, Duparc) and a revised Duparc classification. Orthop Traumatol Surg Res. 2013;99:805–16.
Maripuri SN, Rao P, Manoj-Thomas A, Mohanty K. The classification systems for tibial plateau fractures: how reliable are they? Injury. 2008;39:1216–21.
Millán-Billi A, Gómez-Masdeu M, Ramírez-Bermejo E, Ibañez M, Gelber PE. What is the most reproducible classification system to assess tibial plateau fractures? Int Orthop. 2017;41:1251–6.
Zhu Y, Hu CF, Yang G, Cheng D, Luo CF. Inter-observer reliability assessment of the Schatzker, AO/OTA, and three-column classification of tibial plateau fractures. J Trauma Manag Outcomes. 2013;7:7.
Charalambous CP, Tryfonidis M, Alvi F, Moran M, Fang C, Samarji R, Hirst P. Inter- and intra-observer variation of the Schatzker and AOOTA classifications of tibial plateau fractures. Ann R Coll Surg Engl. 2007;89:478.
Mellema JJ, Doornberg JN, Molenaars RJ, Ring D, Kloen P. Traumaplatform study collaborative & science of variation. Interobserver reliability of the Schatzker and Luo classification systems for tibial plateau fractures. Injury. 2016;47:944–9.
Doornberg JN, Rademakers MV, van den Bekerom MP, Kerkhoffs GM, Ahn J, Steller EP, Kloen P. Two-dimensional and three-dimensional computed tomography for the classification and characterisation of tibial plateau fractures. Injury. 2011;42:1416–25.
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audige L. Fracture and dislocation classification compendium—2007: orthopaedic trauma association classification, database, and outcomes committee. J Orthop Trauma. 2007;21:1–133.
Zhu Y, Yang G, Luo CF, Smith WR, Hu CF, Gao H, Zhong B, Zeng BF. Computed tomography-based three-column classification in tibial plateau fractures: introduction of its utility and assessment of its reproducibility. J Trauma Acute Care Surg. 2012;73:731–7.
R Core Team. R: A language and environment for statistical computing 2018. https://www.r-project.org/ (Version 3.5.1).
Kim CW, Lee CR, An KC, Gwak HC, Kim JH, Wang L, Yoon DG. Predictors of reduction loss in tibial plateau fracture surgery: focusing on posterior coronal fractures. Injury. 2016;47:1483–7.
Menghi A, Mazzitelli G, Marzetti E, Barberio F, D'Angelo E, Maccauro G. Complex tibial plateau fractures: a retrospective study and proposal of the treatment algorithm. Injury. 2017;48:1–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest concerning this article.
Ethical approval
The project was approved by the local ethics committee.
Rights and permissions
About this article
Cite this article
Rossmann, M., Fensky, F., Ozga, AK. et al. Tibial plateau fracture: does fracture classification influence the choice of surgical approach? A retrospective multicenter analysis. Eur J Trauma Emerg Surg 48, 3635–3641 (2022). https://doi.org/10.1007/s00068-020-01388-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-020-01388-z