Abstract
Introduction
Arterial blood gas (ABG) sampling is routinely performed in major trauma patients to assess the severity of hemorrhagic shock. Compared to venous blood gas (VBG), ABG is an additional procedure with risks of hematoma and pain. We aim to determine if pH, base deficit (BD), and lactate from VBG and ABG in trauma patients are clinically equivalent. If proven, the need for ABG and its associated risks can be eliminated.
Methods
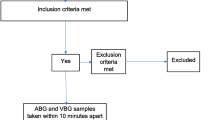
This prospective observational study was conducted in the Emergency Department of National University Hospital, Singapore, between February and October 2016. We correlated paired ABG and VBG results in adult trauma patients. VBG and ABG were obtained within 10 min and processed within 5 min using a point-of-care blood gas analyzer. Bland–Altman plot analysis was used to evaluate the agreement between peripheral VBG and ABG in terms of pH, base deficit and lactate.
Results
There were 102 patients included, with a median age of 34 (interquartile range 28–46) years and male predominance (90.2%). Majority of patients sustained blunt trauma (96.1%), and had injuries of Tier 1 and Tier 2 severity (60/102, 58.8%). Bland–Altman plot analyses demonstrated that only 72.6% of venous pH and 76.5% of venous BD lie within the pre-defined clinically acceptable limits of agreement, whereas 96.0% of venous lactate was within these limits.
Conclusion
Venous and arterial pH and BD are not within clinically acceptable limits of agreement, and ABG should be obtained for accurate acid–base status. However, venous lactate may be an acceptable substitute for arterial lactate.

Similar content being viewed by others
References
WHO Injuries. WHO. https://www.who.int/topics/injuries/en/. Accessed 25 Jan 2016.
Sauaia A, Moore FA, Moore EE, et al. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38:185–93.
Davis JW, Parks SN, Kaups KL, et al. Admission base deficit predicts transfusion requirements and risk of complications. J Trauma. 1996;41:769–74.
Moomey CB, Melton SM, Croce MA, et al. Prognostic value of blood lactate, base deficit, and oxygen-derived variables in an LD50 model of penetrating trauma. Crit Care Med. 1999;27:154–61.
Husain FA, Martin MJ, Mullenix PS, et al. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg. 2003;185:485–91.
Mortensen J. Clinical sequelae from arterial needle puncture, cannulation, and incision. Circulation. 1967;35:1118–23.
McGillivray D, Ducharme FM, Charron Y, et al. Clinical decisionmaking based on venous versus capillary blood gas values in the well-perfused child. Ann Emerg Med. 1999;34:58–63.
Brandenburg MA, Dire DJ. Comparison of arterial and venous blood gas values in the initial emergency department evaluation of patients with diabetic ketoacidosis. Ymem. 1998;31:459–65.
Arnold TDW, Miller M, Van Wessem KJP, et al. Base deficit from the first peripheral venous sample: a surrogate for arterial base deficit in the trauma bay. J Trauma. 2011;71:793–7.
Rudkin SE, Kahn CA, Oman JA, et al. Prospective correlation of arterial vs venous blood gas measurements in trauma patients. Am J Emerg Med. 2012;30:1371–7.
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Equator Network. http://www.equator-network.org/reporting-guidelines/strobe/. Accessed 25 Jan 2016.
Baker SP, O’Neill B, Haddon W, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96.
Rang LCF, Murray HE, Wells GA, et al. Can peripheral venous blood gases replace arterial blood gases in emergency department patients? CJEM. 2002;4:7–15.
Mikkelsen ME, Miltiades AN, Gaieski DF, et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009;37:1670–7.
Lavery RF, Livingston DH, Tortella BJ, et al. The utility of venous lactate to triage injured patients in the trauma center. J Am Coll Surg. 2000;190:656–64.
Davis JW, Mackersie RC, Holbrook TL, et al. Base deficit as an indicator of significant abdominal injury. Ann Emerg Med. 1991;20:842–4.
Aslar AK, Kuzu MA, Elhan AH, et al. Admission lactate level and the APACHE II score are the most useful predictors of prognosis following torso trauma. Injury. 2004;35:746–52.
van Rein EAJ, Houwert RM, Gunning AC, et al. Accuracy of prehospital triage protocols in selecting major trauma patients. J Trauma Acute Care Surg. 2017;1:328–39.
Liu NT, Holcomb JB, Wade CE, et al. Inefficacy of standard vital signs for predicting mortality and the need for prehospital life-saving interventions in blunt trauma patients transported via helicopter. J Trauma Acute Care Surg. 2017;1:S98–103.
Lechleuthner A, Lefering R, Bouillon B, et al. Prehospital detection of uncontrolled haemorrhage in blunt trauma. Eur J Emerg Med. 1994;1:13–8.
Demetriades D, Chan LS, Bhasin P, et al. Relative bradycardia in patients with traumatic hypotension. J Trauma. 1998;45:534–9.
Parks JK, Elliott AC, Gentilello LM, et al. Systemic hypotension is a late marker of shock after trauma: a validation study of Advanced Trauma Life Support principles in a large national sample. Am J Surg. 2006;192:727–31.
Squires JE. Risks of Transfusion. South Med J. 2011;104:762–9.
Schmelzer TM, Perron AD, Thomason MH, et al. A comparison of central venous and arterial base deficit as a predictor of survival in acute trauma. Am J Emerg Med. 2008;26:119–23.
Malinoski DJ, Todd SR, Slone DS, et al. Correlation of central venous and arterial blood gas measurements in mechanically ventilated trauma patients. Arch Surg. 2005;140:1122–5.
Malatesha G, Singh NK, Bharija A, et al. Comparison of arterial and venous pH, bicarbonate, PCO2 and PO2 in initial emergency department assessment. Emerg Med J. 2007;24:569–71.
Byrne AL, Bennett M, Chatterji R, et al. Peripheral venous and arterial blood gas analysis in adults: are they comparable? A systematic review and meta-analysis. Respirology. 2014;19:168–75.
Davis JW, Shackford SR, Mackersie RC, et al. Base deficit as a guide to volume resuscitation. J Trauma. 1988;28:1464–7.
Gustafson ML, Hollosi S, Chumbe JT, et al. The effect of ethanol on lactate and base deficit as predictors of morbidity and mortality in trauma. Am J Emerg Med. 2015;33:607–13.
Pascoe S, Lynch J. Management of hypovolaemic shock in the trauma patient. In: Sisson G, Parr M, Sugrue M, editors. Committee NICPG. Sydney: ITIM (Institute of Trauma and Injury Management) NSW Health; 2007.
Davis JW, Kaups KL, Parks SN. Effect of alcohol on the utility of base deficit in trauma. J Trauma. 1997;43:507–10.
McAuliffe JJ, Lind LJ, Leith DE, et al. Hypoproteinemic alkalosis. Am J Med. 1986;81:86–90.
Ohmori T, Kitamura T, Ishihara J, et al. Early predictors for massive transfusion in older adult severe trauma patients. Injury. 2016;48:1006–12.
Martin MJ, FitzSullivan E, Salim A, et al. Discordance between lactate and base deficit in the surgical intensive care unit: which one do you trust? Am J Surg. 2006;191:625–30.
Wilson RF, Sibbald WJ. Approach to acid–base problems in the critically ill and injured. JACEP. 1976;5:515–22.
Acknowledgements
We thank our colleagues at the Emergency Medicine Department, National University Hospital, Singapore, for their contributions to image acquisition, data collection and patient recruitment.
Funding
Junior Pitch for Funds, National University Hospital (Grant No. JPFF-15-2-BYR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from patients who have mental capacity before study recruitment. For patients who were unable to provide consent, we obtained waiver of consent at time of enrolment with delayed written informed consent after the patient regained mental capacity. The study protocol was approved by the Domain Specific Review Board, National Healthcare Group, Singapore (DSRB 2015/00904).
Rights and permissions
About this article
Cite this article
Boon, Y., Kuan, W.S., Chan, Y.H. et al. Agreement between arterial and venous blood gases in trauma resuscitation in emergency department (AGREE). Eur J Trauma Emerg Surg 47, 365–372 (2021). https://doi.org/10.1007/s00068-019-01190-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01190-6