Abstract
Purpose
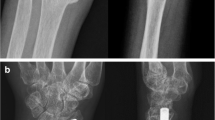
In this study, we retrospectively evaluated patients with isolated diaphyseal radius fractures treated with plates or IMNs and compared their radiological and functional results.
Methods
49 patients who met the criteria were included in the study. Of these, 22 were treated with plate osteosynthesis and 27 with IMNs. The mean age of plate group was 36.8 (range 17–68), IMN group was 34.3 (range 18–74). 39 (79.6%) of the patients were males and 10 (20.4%) were females. The mean follow-up period was 26 (range 12–48) months.
Results
The mean union time was 12.1 ± 0.9 weeks in the IMN group and 12.2 ± 1.2 weeks in the plate group. Union was achieved in all patients in the IMN group (100%) and in 21 of 22 patients in the plate group (95.4%). The mean operation time was 21 (range 15–35) min in the IMN group and 46 (range 40–110) min in the plate group. There was no statistically significant difference between groups according to DASH scores, Grace–Eversmann evaluations, grip strength, forearm pronation and supination degrees, type of fracture, length of hospital stay, and time between injury and surgery (p > 0.05). Complete elbow and wrist range of motion was achieved in all patients.
Conclusions
With similar union rates, functional results, and shorter operating times, locked IMNs are a suitable alternative to plate osteosynthesis in adult isolated diaphyseal radius fractures.



Similar content being viewed by others
References
Reilly TJ. Isolated and combined fractures of the diaphysis of the radius and ulna. Hand Clin. 2002;18(1):179–94.
Dodge HS, Cady GW. Treatment of fractures of radius and ulna with compression plates. J Bone Jt Surg Am. 1972;54(6):1167–76.
Chapman MW, Gordon JE, Zissimos AG. Compression-plate fixation of acute fractures of the diaphyses of the radius and ulna. J Bone Jt Surg Am. 1989;71(2):159–69.
Moss JP, Bynum DK. Diaphyseal fractures of the radius and ulna in adults. Hand Clin. 2007;23(2):143–51.
Saka G, Saglam N, Kurtulmuş T, Avcı CC, Akpinar F, Kovaci H, et al. New interlocking intramedullary radius and ulna nails for treating forearm diaphyseal fractures in adults: a retrospective study. Injury. 2014;45(1):16–23.
Kose A, Aydın A, Ezirmik N, Topal M, Can CE, Yılar S. Intramedullary nailing of adult isolated diaphyseal radius fractures. Ulus Travma Acil Cerrahi Derg. 2016;22(2):184–91.
Müller ME, Algöwer M, Schneider R, Willenegger H. Manuel of internal fixation. 3rd ed. Berlin: Springer; 1991. p. 132–3.
Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Jt Surg Am. 1976;58(4):453–8.
Anderson LD, Sisk D, Tooms RE, Park WI 3rd. Compression-plate fixation in acute diaphyseal fractures of the radius and ulna. J Bone Jt Surg Am. 1975;57(3):287–97.
Ring D, Rhim R, Carpenter C, Jupiter JB. Isolated radial shaft fractures are more common than Galeazzi fractures. J Hand Surg Am. 2006;31(1):17–21.
Mares O. Distal radioulnar joint instability. Hand Surg Rehabil. 2017;36(5):305–13.
Grace TG, Eversmann WW Jr. Forearm fractures: treatment by rigid fixation with early motion. J Bone Jt Surg Am. 1980;62(3):433–8.
Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29(6):602–8.
Mikic ZD. Galeazzi fracture-dislocation. J Bone Jt Surg Am. 1975;57(8):1071–80.
Reckling FW. Unstable fracture-dislocations of the forearm (Monteggia and Galeazzi lesions). J Bone Jt Surg Am. 1982;64(6):857–63.
Moore TM, Klein JP, Patzakis MJ, Harvey JP Jr. Result of compression-plating of closed Galeazzi fractures. J Bone Jt Surg Am. 1985;67(7):1015–21.
Rettig ME, Raskin KB. Galeazzi fracture-dislocation: a new treatment-oriented classification. J Hand Surg Am. 2001;26(2):228–35.
Duijvenbode DC, Guitton TG, Raaymakers EL, Kloen P, Ring D. Long-term outcome of isolated diaphyseal radius fractures with and without dislocation of the distal radioulnar joint. J Hand Surg Am. 2012;37(3):523–7.
Schemitsch EH, Richards RR. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. J Bone Jt Surg Am. 1992;74(7):1068–78.
Sage FP. Medullary fixation of fractures of the forearm. A study of the medullary canal of the radius and a report of fifty fractures of the radius treated with a prebend triangular nail. J Bone Jt Surg Am. 1959;41:1489–516.
Matthews LS, Kaufer H, Garver DF, Sonstegard DA. The effect on supination-pronation of angular malalignment of fractures of both bones of the forearm. J Bone Jt Surg Am. 1982;64(1):14–7.
Lee SK, Kim KJ, Lee JW, Choy WS. Plate osteosynthesis versus intramedullary nailing for both forearm bones fractures. Eur J Orthop Surg Traumatol. 2014;24(5):769–76.
Jones DB Jr, Kakar S. Adult diaphyseal forearm fractures: intramedullary nail versus plate fixation. J Hand Surg Am. 2011;36(7):1216–9.
Deluca PA, Lindsey RW, Ruwe PA. Refracture of bones of the forearm after the removal of compression plates. J Bone Jt Surg Am. 1988;70(9):1372–6.
Knight RA, Purvis GD. Fractures of both bones of the forearm in adults. J Bone Jt Surg Am. 1949;31(4):755–64.
Fanuele J, Blazar P. Extensor pollicis tendon rupture in an adult after intramedullary nailing of a radius fracture: case report. J Hand Surg Am. 2009;34(4):627–9.
Funding
The authors declare that this research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
BK and TH contributed to the design and development of the study and the collection, interpretation, and analysis of the data; the document was written by BK.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Kibar, B., Kurtulmuş, T. Comparison of new design locked intramedullary nails and plate osteosynthesis in adult isolated diaphyseal radius fractures. Eur J Trauma Emerg Surg 46, 1429–1435 (2020). https://doi.org/10.1007/s00068-019-01131-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01131-3