Abstract
Background
Patients undergoing major open emergency abdominal surgery experience high morbidity and mortality rates and often have sepsis at admission. The purpose of this study was to evaluate the association between antibiotic timing and in-hospital outcomes such as complications, need for reoperation, length of stay, and 30-day mortality.
Methods
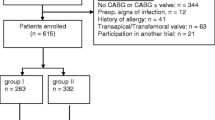
This retrospective observational cohort study was conducted between January 2010 and December 2015 including patients that were triaged through the emergency department for subsequent major open abdominal surgery. All relevant perioperative data were extracted from medical records. The outcomes of interest were development of in-hospital postoperative complications, reoperations, length of stay, and 30-day mortality, all in association with antibiotic timing, categorized according to 0–6, 6–12, or > 12 h from triage. Multivariate logistic regression was performed to evaluate adjusted outcomes associated with antibiotic timing.
Results
A total of 408 patients were included, of whom 107 (26.2%) underwent at least one reoperation and 55.4% had at least one postoperative complication. These complications consisted of 26% surgical complications and 74% medical complications. Of the surgical complications, 73% were Clavien–Dindo ≥ 3. The median length of stay was 9 days and the overall 30-day mortality was 17.9%. The data showed that the development of complications, need for reoperation, 30-day mortality, and the length of stay were significantly correlated to delayed antibiotic administration of more than 12 h from admission.
Conclusions
Antibiotic administration more than 12 h from triage was associated with a significantly increased risk of postoperative complications, need for reoperation, 30-day mortality, and a prolonged length of stay, when compared to patients that received antibiotic treatment 0–6 h and 6–12 h after triage. Our data suggest that prophylactic antibiotics should be administered to all patients undergoing major open emergency abdominal surgery; however, the dose and duration cannot be concluded on the basis of our data and should be further examined.
Similar content being viewed by others
References
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–55.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA Netw. 2016;315(8):801–10.
Deutschman CS, Tracey KJ. Sepsis: current dogma and new perspectives. Immunity. 2014;40(4):463–75.
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive care Med. 2008;34(1):17–60.
Torio CM, Andrews RM. National Inpatient Hospital Costs. The Most Expensive Conditions by Payer, 2011: Statistical Brief #160. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville: Agency for Healthcare Research and Quality (US); 2006.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637.
Soong J, Soni N. Sepsis: recognition and treatment. Clin Med (Lond, Engl). 2012;12(3):276–80.
Marik PE. Early management of severe sepsis: concepts and controversies. Chest J Am Coll Chest Physicians. 2014;145(6):1407–18.
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589–96.
Hecker A, Uhle F, Schwandner T, Padberg W, Weigand MA. Diagnostics, therapy and outcome prediction in abdominal sepsis: current standards and future perspectives. Langenbeck’s Arch Surg. 2014;399(1):11–22.
Smith M, Hussain A, Xiao J, Scheidler W, Reddy H, Olugbade K Jr, Cummings D, Terjimanian M, Krapohl G, Waits SA, et al. The importance of improving the quality of emergency surgery for a regional quality collaborative. Ann Surg. 2013;257(4):596–602.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, Sørensen HT, von Elm E, Langan SM. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med. 2015;12(10):e1001885.
Khuri SF, Daley J, Henderson W, Hur K, Demakis J, Aust JB, Chong V, Fabri PJ, Gibbs JO, Grover F, et al. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg. 1998;228(4):491–507.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Sutton R, Bann S, Brooks M, Sarin S. The Surgical Risk Scale as an improved tool for risk-adjusted analysis in comparative surgical audit. Br J Surg. 2002;89(6):763–8.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Nelson RL, Glenny AM, Song F. Antimicrobial prophylaxis for colorectal surgery. The Cochrane Database Syst Rev. 2009;1:Cd001181.
Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J, Schorr C, Artigas A, Ramsay G, Beale R, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010;36(2):222–31.
Moore LJ, Moore FA. Early diagnosis and evidence-based care of surgical sepsis. J Intensive Care Med. 2013;28(2):107–17.
Fitousis K, Moore LJ, Hall J, Moore FA, Pass S. Evaluation of empiric antibiotic use in surgical sepsis. Am J Surg. 2010;200(6):776–82 (discussion 82).
Sterling SA, Miller WR, Pryor J, Puskarich MA, Jones AE. The impact of timing of antibiotics on outcomes in severe sepsis and septic shock: a systematic review and meta-analysis. Crit Care Med. 2015;43(9):1907–15.
Hagel S, Pletz MW, Brunkhorst FM, Seifert H, Kern WV. Bacteremia and sepsis. Der Internist. 2013;54(4):399–407.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mücahit Harmankaya, Jakob Ohm Oreskov, Jakob Burcharth, and Ismail Gögenur declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Harmankaya, M., Oreskov, J.O., Burcharth, J. et al. The impact of timing of antibiotics on in-hospital outcomes after major emergency abdominal surgery. Eur J Trauma Emerg Surg 46, 221–227 (2020). https://doi.org/10.1007/s00068-018-1026-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-1026-4