Abstract
Introduction
Fall from heights is high energy injuries and constitutes a fraction of all fall-related trauma evaluations while bearing an increase in morbidity and mortality. We hypothesize that despite advancements in trauma care, the overall survivability has not improved in this subset of trauma patients.
Methods
All adult trauma patients treated after sustaining a fall from heights during a 40-month period were retrospectively reviewed. Admission demographics, clinical data, fall height (ft), injury patterns, ISS, GCS, length of stay, and mortality were reviewed.
Results
116 patients sustained a fall from heights, 90.4% accidental. A mean age of 37± 14.7 years, 86% male, and a fall height of 19 ± 10 ft were encountered. Admission GCS was 13 ± 2 with ISS 10 ± 11. Overall LOS was 6.6 ± 14.9 days and an ICU LOS of 2.8 ± 8.9 days. Falls ≥ 25 ft.(16%) had lower GCS 10.4 ± 5.8, increased ISS 22.6 ± 13.8, a fall height 37.9 ± 13.1 ft and associated increased mortality (p < 0.001). Mortality was 5.2%, a mean distance fallen of 39 ± 22 ft. and an ISS of 31.5 ±16.5. Brain injury was the leading cause of death, 50% with open skull fractures.
Conclusion
Level of height fallen is a good predictor of overall outcome and survival. Despite advances in trauma care, death rates remain unchanged. Safety awareness and injury prevention programs are needed to reduce the risk of high-level falls.
Similar content being viewed by others
Introduction
Fall from heights is a familiar source of injury and not uncommonly is secondary to recreational, occupational, or intentional causes. Reported as the most frequent mechanism of self-inflicted trauma, these high-level falls compose a considerable portion of preventable morbidity and mortality [1]. The 50% mortality for deceleration injuries sustained from free falls is four stories (48 ft. or 14.6 m), and falls from greater than 60 ft. (18.3 m) almost uniformly are lethal [2].
In many urban cities, home or building-related falls are frequently encountered and unfortunately remain the most common cause of workplace fatalities among residential construction workers in the United States [3]. Historically in the late 1960s, 12% of all deaths under the age of 15 were the result of falls from heights in New York City [4]. An estimated 86,500 balcony fall-related injuries were treated in US hospital emergency departments from 1990 through 2006, equating to 1.3–2.4 injuries per 100,000 US resident population [5].
Universally, high-level falls are associated with a constitution of injuries of more than one body region. Not uncommonly these injuries are unintentional and remain a public health problem in many metropolitan areas regardless of the circumstances. Injury prevention and management programs are fundamental to risk reduction strategies for the community, despite variability in previous published reports and the correlation between height level and injury patterns.
The purpose of this study was to assess the association between height level and injury patterns with in-hospital mortality as we hypothesize that despite the evolution of trauma care, the overall survivability has not improved in this trauma population.
Methods
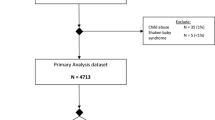
Following an independent Institutional Review Board (IRB) approval, a retrospective analysis of the trauma database was conducted during a 40-month period from 2011 to 2014. All high-level fall injuries greater than 17 years of age treated at Grand Strand Medical Center, a level II trauma center in Myrtle Beach, South Carolina, were evaluated by chart review and a single investigator. Fall from heights included building or home roofs, balconies, windows and other high-level falls. All falls from heights greater than one story level (~10.8 feet or 3.3 m) were identified; heights under 10 feet (ft) were not considered to be of significant mechanism or deceleration from a free fall and, thus, were excluded from this study. All other mechanisms of injury and individuals less than 17 years of age were also excluded.
Patients were divided into those who fell from a height of <25 ft. (7.6 m) and were admitted, those who fell from a height ≥25 ft. and admitted, and those who were discharged from the emergency room. Admission demographics, fall height (ft), injury patterns, and physiologic status on initial evaluation were retrospectively reviewed. Data collection also encompassed the Glascow coma scale (GCS) score, Injury Severity Score (ISS), length of stay (LOS), intensive care unit (ICU) LOS, blood product utilization, and surgical procedures. Collected outcome variables included complications and mortality. Descriptive statistics were calculated to determine data characteristics, with all parametric data reported as mean ± SD. This along with a range was provided in both the demographic table and results. Continuous variables were compared using a two-tailed t test while categorical variables were compared by performing a χ 2 or Fisher’s exact test, as appropriate. A Kruskal–Wallis test was used to compare three subgroup populations for variables including age, fall height, ISS, GCS, hemoglobin and systolic blood pressure. All statistical analyses were performed using QI Macros for Excel (KnowWare International, Inc., 2012, Denver, CO). All p values of less than 0.05 were considered significant.
Results
During the study period, there were 116 patients who had significant falls. Eighty-seven patients (74%) required hospital admission. Patients not admitted were found to have fallen from a height of 15.7 ± 6.7 with a mean ISS of 3.2 ± 3.4. The patient population was predominately male (86%). Mean age was 37 ± 14.7 years (range 18–83 years) with the most common age group being 20–29 years of age (31%). The overall mean fall height was 19.0 ± 10.4 ft. (range 10.8–70 ft). Accidental falls occurred in 90.4%, while 9.6% fell purposeful. More than one-third (35%) had positive blood alcohol levels, a mean of 0.205 mg/dL. Toxicology screen and positive opiate users were more likely to require surgical intervention (p = 0.007). Women were more likely to be intoxicated (p = 0.008), a fall height 18 ± 8 ft., and were 1.2 times more likely to require surgery than men.
A significant relationship was seen between the height of fall at 25 ft. and GCS, a need for a transfusion, and mortality among all comparison groups; with a significant relationship observed at a fall height of 25 ft. and ISS among admitted patients. Overall mean ISS was 10 ± 11 (range 1–57) and a GCS of 13 ± 2. Average ISS of falls ≥25 ft. was 22.6 ± 13.8 (mean rank 22) compared to an average ISS of 9.5 ± 8.6 (mean rank 8) for falls <25 ft. and 3.2 ± 3.4 (mean rank 2) for non-admissions, however not significant (p = 0.167). As the height of fall increased, ISS increased (Fig. 1). Among admitted patients, the ISS was significantly higher with heights ≥25 ft. (p = 0.001). Those with a GCS of ≤8 had fallen significantly higher heights (p < 0.001), a mean fall height of 31 versus 17.3 ft. (GCS of ≥9). Blood transfusions were required in 12.9% of all patients with falls ≥25 ft. more likely to require a transfusion (p < 0.001). Blood product utilization included: packed red blood cells 115 U; fresh frozen plasma 20 U; platelet 13 pack cells. Additional demographics and clinical data are summarized in Table 1.
Four patients (3%) arrived in shock (systolic blood pressure <90 mmHg), with a mean fall height of 55 ± 17 ft., an ISS of 16 (9–24), and a GCS of 6 ± 6 (3–15). The etiology of the hypotension in two patients was related to hemorrhagic shock and bleeding from pelvic fractures. The remaining two patients had depressed skull fractures and significant intracranial hemorrhage, subsequently dying. Two patients did arrive in cardiac arrest with one surviving. Various injury patterns were observed and are summarized in Table 2. Orthopedic (56.3%) and neurospine injury (52.9%) were the most common injuries encountered. Surgical intervention was performed on 37.6% of the admitted patients and was directly related to the type of injury endured (p = 0.040). Thoracic injuries were more likely to require surgical intervention than neuro spinal injuries (p = 0.033; OR 3.1, 95% Confidence Interval 1.1–8.7). Upper and lower extremity fractures were 7 times more likely to require surgical intervention than head injuries (p = 0.001; OR 7.2, 95% Confidence interval 2.2–23.6). Intra-abdominal injuries were encountered in 13.8% of the patients, a fall height 25 ± 14 ft. Hollow viscus injury occurred in only two patients while splenic injury (60%) was the most common of the solid organs (83%) injured followed by kidney (20%). When comparing torso injuries, intra-abdominal injuries were significantly less likely to require surgical intervention compared to the thorax (p = 0.012). Height of fall was not an influential factor in requiring surgical intervention.
Overall mean LOS was 6.6 ± 14.9 days (range 1–129) and an ICU LOS of 2.8 ± 8.9 days (range 1–68) in 33 patients, with average ventilator days of 11.5 ± 16.3 days. On average, total LOS, ICU LOS, and ventilator days were longer among males. In comparison between gender: total LOS of 7.2 ± 16.0 versus 3.4 ± 3.6 days (p = 0.046); ICU LOS 10.8 ± 15.0 versus 3 ± 1.0 days (p = 0.009) and ventilator days of 12.5 ± 16.8 versus 1.5 ± 0.7 days (p = 0.011).
Brain injury was the most common cause of death, 50% sustaining depressed skull fractures. In-hospital mortality was 5.2%, a mean distance fallen of 39 ± 22 ft., an ISS of 31.5 ± 16.5, a base deficit −6.4 ± 7.7, and a pH of 7.19 ± 0.24. Patients falling ≥25 feet patients were more likely to die in comparison to falls <25 ft. (p < 0.001) and non-admissions. However, one patient survived a fall of 65 ft., sustaining multiple injuries with an ISS of 24.
Discussion
The use of the distance of a fall as a predictor of severe injury has been established as part of the trauma field triage. The American College of Surgeons recommend that patients injured in falls from heights greater than 20 feet need to be evaluated at a trauma center and commonly represent a significant portion of trauma hospital admissions. Our state and regional protocol mandates fall victims of greater than 20 feet be transfered to nearest trauma center. Historically, the median lethal dose (LD50) for falls is four stories, or 48 ft., and the lethal dose for 90% (LD90) of test subjects is seven stories, or 84 ft [2, 6]. In our study, the lethal dose at three stories correlated with 30% of patients, as 18 total patients fell greater than 30 feet with five expiring during their hospitalization.
Over a 10-year period, Demetriades et al. demonstrated high-level falls (>15 feet) occurring in 2.3% of trauma admissions [7]. Their triage protocol mandates transfer of victims of falls >15 ft. to designated trauma centers for evaluations [7]. Longer hospitalizations were observed when the victims were over 55 years of age, and an increased mortality seen in patients greater than 65 years of age [7, 8]. Understanding the injury patterns and early institution of subspecialty surgical care is imperative for improved outcomes. Overall prognosis of high-level falls remains multifactorial and clinical management can be challenging with increased fall height.
The distance fallen is considered a dominant factor influencing vertical deceleration injury patterns but variability exist in the literature with severity of injury and height fallen. Simmons et al. used a threshold of 20 feet to predict major trauma (ISS > 15) however, Goodacre et al. reported that the height of fall was an isolated variable and a poor predictor of injury severity and did not identify a height threshold [9, 10]. Our results found a significant relationship between the height of fall greater than or equal to 25 ft. with correlation to ISS, GCS, transfusion requirements and risk of death.
Other components that play a critical role impacting injury severity include: the landing surface, fall orientation, elasticity and viscosity of tissue upon contact [7, 11,12,13]. The extent of injury and the likelihood of survival by a certain degree are dependent on body position at impact and predicted by its center of gravity in the upper torso. [10, 12,13,14,15,16,17] The deceleration force to which the body is subjected is proportional to the velocity of impact. The kinetic energy increases due to acceleration during the fall and is maximum at the moment of impact [12, 13].
In our study, brain injuries were the most common cause of death while spinal fractures, particularly the lumbar spine, were one of the most frequent injuries encountered. We identified 17 patients with spinal fractures, with thoracic spine the least common occurrence. The incidence of spinal fractures remains high with high-level falls and commonly occurs at the thoracolumbar junction [11, 17, 18]. Velmahos et al. series found more than two-thirds had spinal trauma confined to the T12 to L5 region [11]. Adherence to spinal precautions and a thorough neurologic examination is crucial. Scalea et al. reported unstable spinal configuration in thirty-seven percent of patients with paraplegia as a common presentation [18]. At our institution, computed tomography scans are generally completed as part of our radiographic workup to identify spinal fractures.
The presentation of skeletal injuries after a significant fall is expected with an overall incidence as high as 80% [11, 17, 18]. Orthopedic injuries are heavily influenced by the site and position at impact. In this series, upper and lower extremity fractures were more likely to require surgical intervention when compared to head injuries. Early operative fracture stabilization and coordination of orthopedic surgical services can lead to improved outcomes, decreased short-term morbidity, early mobilization, and shorter hospitalization. Despite our low incidence of pelvic ring fractures, buttock type landings are associated with pelvic fractures in as many as 80% of cases and vertebral injuries in approximately 50% [19]. We suspect our lower incidence is directly related to the kinematics of the falling body and final position at impact.
In our series, intraabdominal organ injuries occurred in 13.8%, higher than previous published reports with similar fall heights of >25 ft. but these injuries were not the predominant cause of death compared to other series [11, 18, 20]. Reported hollow viscus injuries on the other hand remain a low occurrence [7, 11]. Other injuries well described in the literature include extra-skeletal injuries: retroperitoneal bleeding, vascular and pulmonary injuries.
Mortality, anatomic distribution and the severity of injury increase with age with high level falls [7, 8]. Age, alcohol intoxication, and height of fall were principle determinants in this series for increased risk of injury with a direct correlation found between alcohol and gender. Not uncommonly when screened, alcohol intoxication and illicit drugs play a significant role in fall etiology [11, 21]. Recognizing injury patterns after fall from heights facilitates and improves the assessment and management of fall victims, reflecting a decreased LOS, and overall morbidity and mortality. This study has some limitations; it is a retrospective study and the out-of-hospital mortality rate was not taken into account as well as variables like comorbidities of the patients. Post-mortem review and diagnostics are not completed, leaving undetected injuries in those suffering an early death upon arrival to our institution. Furthermore, details of the surface of impact or circumstances surrounding the fall were not assessed but could provide more insight in the injury patterns we encountered.
In summary, heights ≥ 25 ft. determine the increased severity of injury and likelihood of death, and mandate care by a specialized trauma team and preparedness by first responders. These high-level falls are a predictor of increased ISS, lower GCS, longer LOS, and the need for transfusions. A high index of suspicion and an understanding of potential injuries associated with level of height fallen are a good predictor of overall outcome and survival.
References
David JS, Gelas-Dore B, Inaba K, Levrat A, Riou B, Gueugniaud PY, Schott AM. Are patients with self-inflicted injuries more likely to die? J Trauma. 2007;62(6):1495–500.
Buckman RF, Buckman PD. Vertical deceleration trauma: principles of management. Surg Clin N Am. 1991;71:331–44.
Dong XS, Wang X, Largay JA, Platner JW, Stafford E, Cain CT, Choi SD. Fatal falls in the U.S. residential construction industry. Am J Ind Med. 2014;57(9):992–1000.
Spiegel CN, Lindaman FC. Children can’t fly: a pro- gram to prevent childhood morbidity and mortality from window falls. Am J Public Health. 1977;67:1143–7.
Shields BJ, Burkett E, Smith GA. Epidemiology of balcony fall-related injuries, United States, 1990-2006. Am J Emerg Med. 2011;29(2):174–80.
Rosen P. Emergency medicine: concepts and clinical practice. 4th ed. St. Louis: Mosby-Year Book, Inc; 1998. p. 352.
Demetriades D, Murray J, Brown C, Velmahos G, Salim A, Alo K, Rhee P. High-level falls: type and severity of injuries and survival outcome according to age. J Trauma. 2005;58:342–5.
Rozycki GS, Maull KI. Injuries sustained by falls. Arch Emerg Med. 1991;8(4):245–52.
Simmons E, Hedges JR, Irwin L, Maassberg W, Kirkwood HA Jr. Paramedic injury severity perception can aid trauma triage. Ann Emerg Med. 1995;26:461–8.
Goodacre S, Than M, Goyder EC, et al. Can the distance fallen predict serious injury after a fall from a height? J Trauma. 1999;46:1055–8.
Velmahos G, Demetriades D, Theodorou D, et al. Patterns of injury in victims of urban free-falls. World J Surg. 1997;21(8):816–20.
Atanasijevic TC, Savic SN, Nikolic SD, Djoki VM. Frequency and severity of injuries in correlation with the height of fall. J Forensic Sci. 2005;50(3):608–12.
Lowenstein SR, Yaron M, Carrerro R, Devereux D, Jacobs LM. Vertical trauma: injuries to patients who fall and land on their feet. Ann Emerg Med. 1989;18(2):161–5.
Bergner L, Mayer S, Harris D. Falls from heights: a childhood epidemic in an urban area. Am J Public Health. 1971;61:90–6.
Richter D, Hahn MP, Ostermann PAW, et al. Vertical deceleration injuries: a comparative study of the injury patterns of 101 patients after accidental and intentional high falls. Injury. 1996;27:655–9.
Mathis RD, Levine SH, Phifer S. An analysis of accidental free falls from a height: the ‘spring break’ syndrome. J Trauma. 1993;34:123–6.
Auñón-Martín I, Doussoux PC, Baltasar JL, Polentinos-Castro E, Mazzini JP, Erasun CR. Correlation between pattern and mechanism of injury of free fall. Strateg Trauma Limb Reconstr. 2012;7(3):141–5.
Scalea T, Goldstein A, Phillips T, Sclafani SJA, Panetta T, McAuley J, Shaftan G. An analysis of 161 falls from a height: “the jumper syndrome”. J Trauma. 1986;26:706.
Goonetilleke A. Injuries caused by falls from heights. Med Sci Law. 1980;20:262–75.
Wang MY, Kim A, Griffith PM, et al. Injuries from falls in the pediatric population: an analysis of 729 cases. J Pediatr Surg. 2001;36:1628–32.
Mosenthal AC, Livingston DH, Elcavage J, Merritt S, Stucker S, Falls S. Epidemiology and strategies for prevention. J Trauma. 1995;38(5):753–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest or funding reported by the above authors.
Ethical approval
All human and animal studies have been approved by the appropriate ethics committee/IRB and have therefore been performed in accordance with the ethical standards in the 1964 Declaration of Helsinki, later amendments and National laws.
Rights and permissions
About this article
Cite this article
Alizo, G., Sciarretta, J.D., Gibson, S. et al. Fall from heights: does height really matter?. Eur J Trauma Emerg Surg 44, 411–416 (2018). https://doi.org/10.1007/s00068-017-0799-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0799-1