Abstract
Purpose
Prehospital endotracheal intubation (ETI) for traumatic brain injury (TBI) is a controversial issue. The aim of this study was to investigate the effect of prehospital ETI in patients with TBI.
Methods
Cohort-matched study using the US National Trauma Data Bank (NTDB) 2008–2012. Patients with isolated severe blunt TBI (AIS head ≥3, AIS chest/abdomen <3) and a field GCS ≤8 were extracted from NTDB. A 1:1 matching of patients with and without prehospital ETI was performed. Matching criteria were sex, age, exact field GCS, exact AIS head, field hypotension, field cardiac arrest, and the brain injury type (according PREDOT-code). The matched cohorts were compared with univariable and multivariable regression analysis.
Results
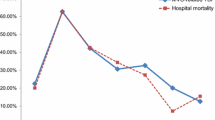
A total of 27,714 patients were included. Matching resulted in 8139 cases with and 8139 cases without prehospital ETI. Prehospital ETI was associated with significantly longer scene (median 9 vs. 8 min, p < 0.001) and transport times (median 26 vs. 19 min, p < 0.001), lower Emergency Department (ED) GCS scores (in patients without sedation; mean 3.7 vs. 3.9, p = 0.026), more ventilator days (mean 7.3 vs. 6.9, p = 0.006), longer ICU (median 6.0 vs. 5.0 days, p < 0.001) and total hospital length of stay (median 10.0 vs. 9.0 days, p < 0.001), and higher in-hospital mortality (31.4 vs. 27.5 %, p < 0.001). In regression analysis prehospital ETI was independently associated with lower ED GCS scores (RC −4.213, CI −4.562/−3.864, p < 0.001) and higher in-hospital mortality (OR 1.399, CI 1.205/1.624, p < 0.001).
Conclusion
In this large cohort-matched analysis, prehospital ETI in patients with isolated severe blunt TBI was independently associated with lower ED GCS scores and higher mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The role of prehospital endotracheal intubation (ETI) in patients with traumatic brain injury (TBI) is a controversial issue. Several retrospective and prospective studies reported worse outcomes associated with prehospital ETI in patients with TBI, including desaturation [1], poor oxygenation at hospital admission [2], more infectious complications [2], poorer neurologic outcomes and functional impairment scores [3], and a higher mortality rate [2, 4–7]. A randomized trial reported that prehospital ETI in patients with severe TBI had no effect on the in-hospital mortality but was associated with a significantly higher rate of favourable neurological outcomes at 6 months [8]. Other studies reported a higher rate of unexpected survivors associated with prehospital ETI in patients with severe TBI [9], no effect [10], or decreased mortality [11] in patients with a field GCS score ≤8 undergoing prehospital ETI.
Previous studies investigating the effect of prehospital ETI on outcomes included patients with severe TBI, defined as an abbreviated injury scale (AIS) head ≥3 or a Glasgow Coma Scale (GCS) ≤8, but most did not differentiate patients with and without associated extracranial traumatic injuries. This is a major limitation, because extracranial injuries may significantly impact the management and outcomes of patients with TBI. Furthermore, the majority of studies included patients with blunt and penetrating injuries. Penetrating TBI is associated with higher rates of certain complications, a different pathophysiology, and a much higher mortality rate when compared to blunt TBI [12–14].
The goal of prehospital ETI in patients with severe TBI is to maintain the airway and prevent hypoxia, thus potentially preventing aspiration and secondary brain injury [15–17]. However, prehospital ETI may be challenging [18], and potential benefits have to be outweighed with ETI-related complications, including multiple intubation attempts [6, 19, 20], improper tube placement [21–24], prolonged scene time [6, 19, 25], transient desaturation [1, 26], hyperventilation [26–29], hypotension [26, 30], hypertensive response to laryngoscopy and ETI [31] which may lead to increased intracranial pressure [32], and ETI/laryngoscopy-induced increased intracranial pressure [33, 34].
The prehospital treatment of trauma patients varies largely in the US [35–37], making it difficult to compare studies that investigated the effect of prehospital ETI in different US study populations. The aim of the current study was, therefore, to investigate the effect of prehospital ETI in patients with isolated severe blunt TBI by using the American College of Surgeons (ACS) National Trauma Data Bank (NTDB).
Patients and methods
Study design and setting
This is a retrospective cohort-matched study using NTDB 2008-2012. NTDB is a US trauma registry managed by the ACS and contains Health Insurance Portability and Accountability Act (HIPAA) de-identified data of participating hospitals [38].
Selection of participants
Patients with isolated severe blunt TBI and a GCS ≤8 were extracted from NTDB. Isolated TBI was defined as an AIS head score ≥3 and an AIS chest and abdomen score <3.
Included patients were divided into two groups: patients undergoing ETI before Emergency Department (ED) admission (prehospital ETI group) and patients not undergoing ETI before ED admission (no prehospital ETI group). Prehospital ETI was assessed using the initial ED GCS qualifier in NTDB.
Data collection
Data collection included patient characteristics (sex, age), injury severity [AIS head score, Injury Severity Score (ISS)], brain injury type (contusion, epidural hematoma, subdural hematoma, subarachnoid haemorrhage, intraparenchymal haemorrhage, intraventricular haemorrhage, diffuse axonal injury, brain swelling, brain laceration, pneumocephalus), prehospital variables (field systolic blood pressure, field GCS, Emergency Medical Service (EMS) prehospital times [total prehospital time (scene arrival to ED arrival), transport time (scene departure to ED arrival), scene time (scene arrival to scene departure)], ED GCS and vital signs (oxygen saturation, systolic blood pressure, heart rate), operative procedures [craniectomy, craniotomy, Intracranial pressure (ICP) monitoring, tracheostomy], and outcome variables [total hospital and intensive care unit (ICU) length of stay (LOS), ventilator days, in-hospital mortality]. Hypotension was defined as a systolic blood pressure <90 mmHg, cardiac arrest as a systolic blood pressure of 0 mmHg, and tachycardia as a heart rate >100 bpm.
Cohort matching
A 1:1 cohort matching of patients with and without prehospital ETI was performed. Matching criteria were age (±5 years), sex, exact field GCS score, exact AIS head score, field hypotension, field cardiac arrest, and the brain injury type (contusion, epidural hematoma, subdural hematoma, subarachnoid haemorrhage, intraparenchymal haemorrhage, intraventricular haemorrhage, diffuse axonal injury, brain swelling, brain laceration, pneumocephalus). The matching procedure was performed without replacement (Fig. 1).
Analysis
Prehospital times, ED variables, operative procedures, and outcome variables were compared in the matched cohorts of patients with and without prehospital ETI.
Normality of distribution was assessed using histograms, skewness, and the Shapiro–Wilk test.
Patient characteristics, injury severity, the brain injury type, prehospital variables, ED variables, operative procedures, and outcome variables were compared in univariable analysis. Categorical variables were analysed using Fisher’s exact test, continuous variables were compared using the Mann–Whitney test. Results were reported as numbers and percentages or medians and interquartile ranges, as appropriate. p values <0.05 were considered statistically significant.
The effect of prehospital ETI on the ED GCS score (in non-sedated patients) and in-hospital mortality was adjusted for patient and injury related factors in multivariate linear and logistic regression analysis. The association of clinically important predictor variables [sex, age, field hypotension, field GCS score, transport time (EMS scene departure to ED arrival), ISS] with the ED GCS score and in-hospital mortality was assessed using Fisher’s exact test, Spearman’s rank order correlation, and logistic regression analysis, as appropriate, and entered in the regression model if the p values was ≤0.1. Regression analysis was performed using the enter method. Interactions of prehospital ETI with other predictor variables were assessed using separate regression analyses. Significant interactions (p < 0.05) were entered in the regression model as interaction terms. Continuous variables with interactions were dichotomized at the median for ease of interpretation. Multicollinearity was assessed using the variance inflation factor (VIF). A VIF <5 was assumed to exclude significant collinearity. Results were reported as odds ratio (OR) or regression coefficient (RC) with 95 % confidence intervals (CI). The regression model performance was assessed using χ 2 goodness of fit statistics, Cox & Snell R 2, and Nagelkerke R 2 for logistic regression, and analysis of variance (ANOVA), R 2, and adjusted R 2 for linear regression.
All statistical analyses were performed using SPSS Statistics (IBM Corporation, Armonk, NY).
Results
Included patients
A total of 220,771 patients with isolated severe blunt TBI were extracted from NTDB. Of these, 19,065 (8.6 %) underwent prehospital ETI and 201,706 (91.4 %) had no prehospital ETI. After the exclusion of patients with a field GCS score >8, the prehospital ETI group was comprised of 11,769 patients and the no prehospital ETI group of 15,945 patients. The 1:1 ratio cohort matching revealed 8139 patients in both groups (Fig. 1).
Baseline characteristics
After the cohort matching, baseline characteristics of the prehospital ETI group and no prehospital ETI group were equal (Table 1).
Prehospital times
Prehospital times were significantly longer in the prehospital ETI group, including the total prehospital time (37 vs. 28 min, p < 0.001), transport time (26 vs. 19 min, p < 0.001), and scene time (9 vs. 8 min, p < 0.001) (Table 2).
Emergency Department variables
The ED GCS score was significantly lower in the prehospital ETI group, both in all patients (median 3.0 vs. 5.0, p < 0.001) and the subgroup of patients without prehospital sedation (mean 3.7 vs. 3.9, p = 0.026). Patients undergoing prehospital ETI had more frequent ED hypotension (7.2 % vs. 4.6 %, p < 0.001), but less frequent ED desaturation <90 mmHg (4.6 % vs. 5.8 %, p < 0.001). The percentage of patients with ED tachycardia was not significantly different between the two groups (37.7 % vs. 36.5 %, p = 0.103) (Table 2).
Procedures
ICP monitoring and tracheostomy were significantly more frequently performed in the prehospital ETI group (14.5 % vs. 12.2 %, p < 0.001 and 19.6 % vs. 14.3 %, p < 0.001). The frequency of neurosurgical procedures (craniectomy and craniotomy) performed was not significantly different between the two groups (Table 2).
Outcome variables
In univariable analysis, patients undergoing prehospital ETI had a longer total hospital LOS (median 10 vs. 9 days, p < 0.001) and ICU LOS (median 6 vs. 5 days, p < 0.001), increased ventilator days (mean 7.3 vs. 6.9 days, p = 0.006), and a higher in-hospital mortality (31.4 % vs. 27.5 %, p < 0.001) (Table 2).
Effect of prehospital ETI on the ED GCS score and in-hospital mortality
In the logistic regression model for in-hospital mortality, a significant interaction of prehospital ETI and the ISS was identified (p < 0.001). In the linear regression model for the ED GCS score, significant interactions of prehospital ETI and field hypotension (p = 0.035), the field GCS score (p < 0.001), and the ISS (p < 0.001) were found.
No significant collinearity was detected between the predictor variables of the regression models (VIF <4).
In multivariate regression analysis, adjusting for patient characteristics, injury related factors and the transport time, prehospital ETI was independently associated with increased in-hospital mortality and lower ED GCS scores (Table 3).
Discussion
It is currently unclear whether patients with severe TBI and a field GCS ≤8 benefit from prehospital ETI, as the effect of prehospital ETI on outcomes is reported differently in the literature [1–9, 11]. Furthermore, due to the great variability of EMS systems in the US [35, 36, 39], the comparison of different prehospital treatment algorithms for patients with severe TBI is difficult.
The aim of this matched cohort study was to investigate the effect of prehospital ETI on outcomes in patients with isolated severe blunt TBI using NTDB, which is a large national database.
In the current study, only patients with a field GCS score ≤8 were included in the analysis. Several current guidelines report a GCS score ≤8, along with other criteria such as airway obstruction, persistent hypoxia despite supplemental oxygen, hypoventilation, severe haemorrhagic shock, and cardiac arrest, as an indication for ETI in patients with severe TBI [40–43]. Thus, all patients included in the current study had the traditional indications for ETI.
Previous studies reported a prolonged scene time [6, 19, 20, 44] and total prehospital time [45] associated with prehospital ETI. In the current study, the scene time, total prehospital time, and transport time were significantly longer in the prehospital ETI group. The longer scene time is most likely related to the more time-consuming prehospital care when ETI is performed, whereas the longer transport time in the prehospital ETI group also may reflect longer transport distances as an indication for ETI [44].
The admission GCS score has been identified as a significant predictor for the need for tracheostomy in patients with TBI undergoing craniotomy [46]. In the current study, the more frequent use of ICP monitoring and the higher number of tracheostomies performed in the prehospital ETI group may also be attributed to the lower ED GCS score in this group, although the scene GCS was similar in both groups.
Prehospital ETI was associated with significantly worse outcomes and more operative procedures performed (Table 2). Even after adjusting for patient and injury related factors, as well as the transport time, patients undergoing prehospital ETI had lower ED GCS scores and higher in-hospital mortality (Table 3). Taking into consideration the results of the current study, likely reasons for the worse outcomes of patients in the prehospital ETI group are the prolonged scene time and more frequent hypotension [26, 30] at ED arrival in this group. Other potential reasons for the worse outcomes of patients undergoing prehospital ETI are technical problems with the procedure, such as esophageal [21–24] or right mainstem bronchus intubation [22–24, 47], aspiration of gastric contents [48], hyperventilation, and the limited experience of paramedics for ETI. According to the American Heart Association guidelines for advanced cardiovascular life support, ETI should only be attempted by healthcare providers experienced in performing the procedure. Providers that perform less than 6–12 prehospital ETI per year should use alternative, non-invasive techniques for airway management according to the guidelines [49]. However, in the literature, the reported number of prehospital ETI performed by paramedics per year is much lower [50–53]. The worse outcomes associated with prehospital ETI therefore may also be related to the insufficient skills for the procedure.
Previous studies report a higher prehospital ETI success rate when the procedure was performed by physicians compared to non-physicians [54, 55] and anesthesiologists compared to non-anesthesiologists [56] It is possible that prehospital ETI performed by an experienced emergency physician may be associated with different outcomes in the current study population. Further randomized studies are needed to resolve this important issue.
Based on the results of the current study, routine prehospital ETI may not be justified in patients with isolated severe blunt TBI and a field GCS score ≤8. The effect of prehospital ETI on outcomes should be evaluated based on the resources and organization of an EMS service, taking into account the training of the providers [57, 58], presence of an emergency physician on scene [44], and transport times [59].
Besides the usual limitations of a retrospective analysis, the current study may be confounded by a selection bias. Despite the accurate matching on multiple patient and injury related factors, it cannot be excluded that patients with worse clinical conditions on scene were more likely to undergo prehospital ETI. Thus, the potentially worse prehospital clinical conditions of patients in the prehospital ETI group may have contributed to the worse outcomes found in these patients. Therefore, a prospective, randomized study, which includes only patients with isolated blunt TBI and takes into account the skills of the health care provider who performs the ETI is imperative.
Conclusion
In this large matched cohort study including patients with isolated severe blunt TBI, prehospital ETI was independently associated with lower ED GCS scores and higher in-hospital mortality.
References
Dunford JV, Davis DP, Ochs M, Doney M, Hoyt DB. Incidence of transient hypoxia and pulse rate reactivity during paramedic rapid sequence intubation. Ann Emerg Med. 2003;42(6):721–8. doi:10.1016/s0196064403006607.
Karamanos E, Talving P, Skiada D, Osby M, Inaba K, Lam L, et al. Is prehospital endotracheal intubation associated with improved outcomes in isolated severe head injury? A matched cohort analysis. Prehosp Disaster Med. 2014;29(1):32–6. doi:10.1017/s1049023x13008947.
Wang HE, Peitzman AB, Cassidy LD, Adelson PD, Yealy DM. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004;5:439–50.
Davis DP, Peay J, Sise MJ, Vilke GM, Kennedy F, Eastman AB, et al. The impact of prehospital endotracheal intubation on outcome in moderate to severe traumatic brain injury. J trauma. 2005;58(5):933–9.
Davis DP, Koprowicz KM, Newgard CD, Daya M, Bulger EM, Stiell I, et al. The relationship between out-of-hospital airway management and outcome among trauma patients with Glasgow Coma Scale Scores of 8 or less. Prehospital Emerg Care. 2011;15(2):184–92. doi:10.3109/10903127.2010.545473.
Davis DP, Hoyt DB, Ochs M, Fortlage D, Holbrook T, Marshall LK, et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J trauma. 2003;54(3):444–53. doi:10.1097/01.ta.0000053396.02126.cd.
Bochicchio GV, Ilahi O, Joshi M, Bochicchio K, Scalea TM. Endotracheal intubation in the field does not improve outcome in trauma patients who present without an acutely lethal traumatic brain injury. J trauma. 2003;54(2):307–11. doi:10.1097/01.ta.0000046252.97590.be.
Bernard SA, Nguyen V, Cameron P, Masci K, Fitzgerald M, Cooper DJ, et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: a randomized controlled trial. Ann Surg. 2010;252(6):959–65. doi:10.1097/SLA.0b013e3181efc15f.
Davis DP, Peay J, Sise MJ, Kennedy F, Simon F, Tominaga G, et al. Prehospital airway and ventilation management: a trauma score and injury severity score-based analysis. J trauma. 2010;69(2):294–301. doi:10.1097/TA.0b013e3181dc6c7f.
Vandromme MJ, Melton SM, Griffin R, McGwin G, Weinberg JA, Minor M, et al. Intubation patterns and outcomes in patients with computed tomography-verified traumatic brain injury. J trauma. 2011;71(6):1615–9. doi:10.1097/TA.0b013e31822a30a1.
Winchell RJ, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury. Trauma Research and Education Foundation of San Diego. Arch Surg. 1997;132(6):592–7 (Chicago, Ill: 1960).
Black KL, Hanks RA, Wood DL, Zafonte RD, Cullen N, Cifu DX, et al. Blunt versus penetrating violent traumatic brain injury: frequency and factors associated with secondary conditions and complications. J head trauma rehabil. 2002;17(6):489–96.
Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7(8):728–41. doi:10.1016/s1474-4422(08)70164-9.
Santiago LA, Oh BC, Dash PK, Holcomb JB, Wade CE. A clinical comparison of penetrating and blunt traumatic brain injuries. Brain Inj: [BI]. 2012;26(2):107–25. doi:10.3109/02699052.2011.635363.
Badjatia N, Carney N, Crocco TJ, Fallat ME, Hennes HM, Jagoda AS, et al. Guidelines for prehospital management of traumatic brain injury, 2nd edition. Prehospital emergency care. 2008;12(Suppl 1):S1–52. doi:10.1080/10903120701732052.
Moppett IK. Traumatic brain injury: assessment, resuscitation and early management. Br J Anaesth. 2007;99(1):18–31. doi:10.1093/bja/aem128.
Yeh DD, Velmahos GC. Prehospital intubation for traumatic brain injury: do it correctly, or not at all. ANZ J surg. 2012;82(7–8):484–5. doi:10.1111/j.1445-2197.2012.06130.x.
Prekker ME, Kwok H, Shin J, Carlbom D, Grabinsky A, Rea TD. The process of prehospital airway management: challenges and solutions during paramedic endotracheal intubation. Crit Care Med. 2014;42(6):1372–8. doi:10.1097/ccm.0000000000000213.
Sloane C, Vilke GM, Chan TC, Hayden SR, Hoyt DB, Rosen P. Rapid sequence intubation in the field versus hospital in trauma patients. J Emerg Med. 2000;19(3):259–64.
von Elm E, Schoettker P, Henzi I, Osterwalder J, Walder B. Pre-hospital tracheal intubation in patients with traumatic brain injury: systematic review of current evidence. Br J Anaesth. 2009;103(3):371–86. doi:10.1093/bja/aep202.
Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37(1):32–7. doi:10.1067/mem.2001.112098.
Wirtz DD, Ortiz C, Newman DH, Zhitomirsky I. Unrecognized misplacement of endotracheal tubes by ground prehospital providers. Prehospital emergency care. 2007;11(2):213–8. doi:10.1080/10903120701205935.
Timmermann A, Russo SG, Eich C, Roessler M, Braun U, Rosenblatt WH, et al. The out-of-hospital esophageal and endobronchial intubations performed by emergency physicians. Anesth Analg. 2007;104(3):619–23. doi:10.1213/01.ane.0000253523.80050.e9.
Jemmett ME, Kendal KM, Fourre MW, Burton JH. Unrecognized misplacement of endotracheal tubes in a mixed urban to rural emergency medical services setting. Acad Emerg Med. 2003;10(9):961–5.
Falcone RE, Herron H, Dean B, Werman H. Emergency scene endotracheal intubation before and after the introduction of a rapid sequence induction protocol. Air Med J. 1996;15(4):163–7.
Rognas L, Hansen TM, Kirkegaard H, Tonnesen E. Anaesthesiologist-provided prehospital airway management in patients with traumatic brain injury: an observational study. Eur J Emerg Med. 2014;21(6):418–23. doi:10.1097/mej.0000000000000103.
Helm M, Hauke J, Lampl L. A prospective study of the quality of pre-hospital emergency ventilation in patients with severe head injury. Br J Anaesth. 2002;88(3):345–9.
Dumont TM, Visioni AJ, Rughani AI, Tranmer BI, Crookes B. Inappropriate prehospital ventilation in severe traumatic brain injury increases in-hospital mortality. J Neurotrauma. 2010;27(7):1233–41. doi:10.1089/neu.2009.1216.
Warner KJ, Cuschieri J, Copass MK, Jurkovich GJ, Bulger EM. The impact of prehospital ventilation on outcome after severe traumatic brain injury. J trauma. 2007;62(6):1330–6. doi:10.1097/TA.0b013e31804a8032 (discussion 6–8).
Shafi S, Gentilello L. Pre-hospital endotracheal intubation and positive pressure ventilation is associated with hypotension and decreased survival in hypovolemic trauma patients: an analysis of the National Trauma Data Bank. J trauma. 2005;59(5):1140–5 (discussion 5–7).
Perkins ZB, Wittenberg MD, Nevin D, Lockey DJ, O’Brien B. The relationship between head injury severity and hemodynamic response to tracheal intubation. J trauma acute care surg. 2013;74(4):1074–80. doi:10.1097/TA.0b013e3182827305.
Bouma GJ, Muizelaar JP, Bandoh K, Marmarou A. Blood pressure and intracranial pressure-volume dynamics in severe head injury: relationship with cerebral blood flow. J Neurosurg. 1992;77(1):15–9. doi:10.3171/jns.1992.77.1.0015.
Burney RG, Winn R. Increased cerbrospinal fluid pressure during laryngoscopy and intubation for induction of anesthesia. Anesth Analg. 1975;54(5):687–90.
Samaha T, Ravussin P, Claquin C, Ecoffey C. Prevention of increase of blood pressure and intracranial pressure during endotracheal intubation in neurosurgery: esmolol versus lidocaine. Ann Fr Anesth Reanim. 1996;15(1):36–40.
Bulger EM, Nathens AB, Rivara FP, MacKenzie E, Sabath DR, Jurkovich GJ. National variability in out-of-hospital treatment after traumatic injury. Ann Emerg Med. 2007;49(3):293–301. doi:10.1016/j.annemergmed.2006.06.038.
Oestern HJ, Trentz O, Uranues S. General trauma care and related aspects: trauma surgery II. Springer, Berlin Heidelberg 2013.
Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, et al. Access to trauma centers in the United States. JAMA J Am Med Assoc. 2005;293(21):2626–33. doi:10.1001/jama.293.21.2626.
Surgeons ACo. National Trauma Data Bank webpage. 2015. https://www.facs.org/quality programs/trauma/ntdb. Accessed March 19 2015.
Bulger EM, Nathens AB, Rivara FP, Moore M, MacKenzie EJ, Jurkovich GJ. Management of severe head injury: institutional variations in care and effect on outcome. Crit Care Med. 2002;30(8):1870–6.
Trauma TEAftSo. Emergency tracheal intubation immediately following traumatic injury—practice management guideline. 2015. https://www.east.org/education/practice-management-guidelines/emergency-tracheal-intubation-immediately-following-traumatic-injury Accessed June 2015.
Mayglothling J, Duane TM, Gibbs M, McCunn M, Legome E, Eastman AL, et al. Emergency tracheal intubation immediately following traumatic injury: an Eastern association for the surgery of trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S333–40. doi:10.1097/TA.0b013e31827018a5.
Evidence-based guidelines for adult traumatic brain injury care. 2015. http://www.jems.com/articles/print/volume-35/issue-4/patient-care/evidence-based-guidelines-adul.html Accessed June 2015.
Dinsmore J. Traumatic brain injury: an evidence-based review of management. Oxford University Press. 2013. http://ceaccp.oxfordjournals.org/content/early/2013/02/24/bjaceaccp.mkt010.full Accessed June 2015.
Sollid SJ, Lossius HM, Soreide E. Pre-hospital intubation by anaesthesiologists in patients with severe trauma: an audit of a Norwegian helicopter emergency medical service. Scandinavian J Trauma Resusc Emerg Med. 2010;18:30. doi:10.1186/1757-7241-18-30.
Cudnik MT, Newgard CD, Wang H, Bangs C, Herringtion RT. Endotracheal intubation increases out-of-hospital time in trauma patients. Prehospital Emerg Care. 2007;11(2):224–9. doi:10.1080/10903120701205208.
Huang YH, Lee TC, Liao CC, Deng YH, Kwan AL. Tracheostomy in craniectomised survivors after traumatic brain injury: a cross-sectional analytical study. Injury. 2013;44(9):1226–31. doi:10.1016/j.injury.2012.12.029.
Geisser W, Maybauer DM, Wolff H, Pfenninger E, Maybauer MO. Radiological validation of tracheal tube insertion depth in out-of-hospital and in-hospital emergency patients. Anaesthesia. 2009;64(9):973–7. doi:10.1111/j.1365-2044.2009.06007.x.
Ufberg JW, Bushra JS, Karras DJ, Satz WA, Kueppers F. Aspiration of gastric contents: association with prehospital intubation. Am J Emerg Med. 2005;23(3):379–82.
Part 6: Advanced Cardiovascular Life Support. Lippincott Williams & Wilkins. 2000. https://circ.ahajournals.org/content/102/suppl_1/I-86.full Accessed June 2015.
Burton JH, Baumann MR, Maoz T, Bradshaw JR, Lebrun JE. Endotracheal intubation in a rural EMS state: procedure utilization and impact of skills maintenance guidelines. Prehospital Emerg Care. 2003;7(3):352–6.
Wang HE, Kupas DF, Hostler D, Cooney R, Yealy DM, Lave JR. Procedural experience with out-of-hospital endotracheal intubation. Crit Care Med. 2005;33(8):1718–21.
Bledsoe BE, Gandy WE. The disappearing endotracheal tube: historic skill threatened by lack of practice & new devices. JEMS. 2009;34(3):88–99. doi:10.1016/s0197-2510(09)70075-0.
Cady CE, Pirrallo RG. The effect of Combitube use on paramedic experience in endotracheal intubation. Am J Emerg Med. 2005;23(7):868–71. doi:10.1016/j.ajem.2005.07.013.
Peters J, van Wageningen B, Hendriks I, Eijk R, Edwards M, Hoogerwerf N, et al. First-pass intubation success rate during rapid sequence induction of prehospital anaesthesia by physicians versus paramedics. Eur J Emerg Med. 2014;. doi:10.1097/mej.0000000000000161.
Lossius HM, Roislien J, Lockey DJ. Patient safety in pre-hospital emergency tracheal intubation: a comprehensive meta-analysis of the intubation success rates of EMS providers. Crit care (Lond Engl). 2012;16(1):R24. doi:10.1186/cc11189.
Lockey D, Crewdson K, Weaver A, Davies G. Observational study of the success rates of intubation and failed intubation airway rescue techniques in 7256 attempted intubations of trauma patients by pre-hospital physicians. Br J Anaesth. 2014;113(2):220–5. doi:10.1093/bja/aeu227.
Breckwoldt J, Klemstein S, Brunne B, Schnitzer L, Arntz HR, Mochmann HC. Expertise in prehospital endotracheal intubation by emergency medicine physicians-Comparing ‘proficient performers’ and ‘experts’. Resuscitation. 2012;83(4):434–9. doi:10.1016/j.resuscitation.2011.10.011.
Harris T, Lockey D. Success in physician prehospital rapid sequence intubation: what is the effect of base speciality and length of anaesthetic training? Emerg Med J EMJ. 2011;28(3):225–9. doi:10.1136/emj.2009.088302.
Boer C, Franschman G, Loer SA. Prehospital management of severe traumatic brain injury: concepts and ongoing controversies. Current Opin Anaesthesiol. 2012;25(5):556–62. doi:10.1097/ACO.0b013e328357225c.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tobias Haltmeier, Elizabeth Benjamin, Stefano Siboni, Evren Dilektasli, Kenji Inaba, and Demetrios Demetriades have no conflicts of interest or financial ties to disclose.
Ethical approval
Ethical approval for the current study was obtained from the Institutional Review Board (IRB) of the University of Southern California.
Rights and permissions
About this article
Cite this article
Haltmeier, T., Benjamin, E., Siboni, S. et al. Prehospital intubation for isolated severe blunt traumatic brain injury: worse outcomes and higher mortality. Eur J Trauma Emerg Surg 43, 731–739 (2017). https://doi.org/10.1007/s00068-016-0718-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-016-0718-x