Abstract
Purpose
The aim of this study was to retrospectively study survival and long-term morbidities of children with nasopharyngeal carcinoma (NPC) treated by induction chemotherapy and concurrent chemoradiation (CRT). The total dose of radiation was adapted to the response following neoadjuvant chemotherapy.
Methods
Children with non-metastatic NPC treated in France between 1999 and 2015 were retrospectively included in the study. The strategy combined neoadjuvant platinum-based chemotherapy, followed by adapted CRT to tumor response.
Results
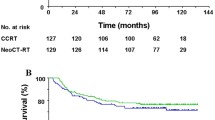
In total, 95 patients (median age 15 years [range, 7–23 years], male-to-female ratio 1.8) with undifferentiated NPC were included; 59% of patients had TNM stage IV. Intensity-modulated radiotherapy (IMRT) was delivered to 57 patients (60%), while the other patients were treated with conformal RT (3D-RT). After a median follow-up of 4.5 years [range, 3.6–5.5 years], 13 relapses and seven deaths had occurred. The 3‑year overall and relapse-free survival (RFS) were 94% [95% CI, 85–97%] and 86% [77–92%], respectively. The locoregional failure rate was 6% [95% CI, 2–14]. Long-term treatment-related sequelae of grade 2+ were reported by 37 (50%) patients; odynophagia was significantly reduced treated by IMRT vs. conventional 3D-RT (7% vs. 55%, p = 0.015). Using a reduction dose of 59.4 Gy, 54 Gy, and 45 Gy, respectively, to the primary, involved, and uninvolved neck nodes, after a favorable tumor response, was not associated with an increased locoregional failure rate.
Conclusions
The survival rates for NPC have been considerably improved by means of multimodal therapy, but long-term locoregional morbidity remains common. Use of IMRT may induce less residual odynophagia. Radiation dose reduction adapted to chemotherapy response does not have a negative impact on outcome. These findings support the use of an RT protocol adapted to the tumor response to neoadjuvant chemotherapy for a long-lasting improvement in the patient’s quality of life.
Zusammenfassung
Zielsetzung
Retrospektive Analyse der Überlebenszeit und der Langzeitmorbidität von Kindern mit Nasopharynxkarzinom (NPC), die mit neoadjuvanter Chemotherapie und zeitgleicher Chemoradiotherapie (CRT) behandelt wurden. Die Strahlendosis wurde an die Reaktion auf die neoadjuvante Chemotherapie angepasst.
Methoden
Kinder mit nichtmetastasiertem NPC, die zwischen 1999 und 2015 in Frankreich behandelt wurden, wurden retrospektiv in die Studie eingeschlossen. Die Behandlungsstrategie bestand aus einer Kombination von neoadjuvanter platinbasierter Chemotherapie, gefolgt von einer an das Ansprechen auf Chemotherapie angepassten Strahlentherapie.
Ergebnisse
Fünfundneunzig Patienten (mittleres Alter 15 Jahre, Spanne7–23 Jahre; Verhältnis Männer/Frauen 1,8) mit NPC vom Typ III konnten in die Studie eingeschlossen werden; 59 % der Patienten hatten ein TNM-Stadium IV. Bei 57 Patienten (60 %) wurde eine intensitätsmodulierte Strahlentherapie (IMRT) verabreicht, während die anderen Patienten mit einer konformen RT (3D-RT) behandelt wurden. Nach einer medianen Nachbeobachtungszeit von 4,5 Jahren (Spanne 3,6–5,5 Jahre) traten 13 Rückfälle und 7 Todesfälle auf. Die 3‑Jahres-Gesamtüberlebensrate und die rezidivfreie Überlebensrate (RÜR) betrugen 94 % (95 %-Konfidenzintervall [KI] 85–97 %) bzw. 86 % (95%-KI 77–92 %). Die regionale Rückfallrate betrug 6 % (95 %-KI 2–14). Langzeitfolgeerscheinungen von Grad 2 oder höher traten bei 37 Patienten (50 %) auf; Odynophagie war bei Patienten, die mit IMRT behandelt wurden, im Vergleich zu herkömmlicher 3D-RT signifikant reduziert (7 % vs. 55 %; p = 0,015). Die Verwendung einer Reduktionsdosis von 59,4 Gy, 54 Gy bzw. 45 Gy für die primären, betroffenen und nichtbetroffenen Halsknoten nach günstiger Tumorantwort war nicht mit einer erhöhten lokoregionalen Ausfallrate verbunden.
Schlussfolgerung
Die NPC-Überlebensraten konnten durch eine multimodale Therapie erheblich verbessert werden; eine lokoregionale Langzeitmorbidität besteht jedoch nach wie vor. Das IMRT-Verfahren kann zu einer Verringerung der Odynophagie führen. Die an das Ansprechen auf Chemotherapie angepasste Dosisreduktion hat keinen negativen Einfluss auf die Überlebensraten. Diese Ergebnisse unterstützen die Verwendung eines RT-Protokolls, das an das Ansprechen auf neoadjuvante Chemotherapie angepasst ist, um die Lebensqualität des Patienten nachhaltig zu verbessern.

Similar content being viewed by others
References
Desandes E, Lacour B, Sommelet D et al (2004) Cancer incidence among adolescents in France. Pediatr Blood Cancer 43(7):742–748
Downing NL, Wolden S, Wong P et al (2009) Comparison of treatment results between adult and juvenile nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 75(4):1064–1070
Orbach D, Brisse H, Helfre S et al (2008) Radiation and chemotherapy combination for nasopharyngeal carcinoma in children: Radiotherapy dose adaptation after chemotherapy response to minimize late effects. Pediatr Blood Cancer 50(4):849–853
Dourthe ME, Bolle S, Temam S et al (2018) Childhood Nasopharyngeal Carcinoma: State-of-the-Art, and Questions for the Future. J Pediatr Hematol Oncol 40:85–92
Casanova M, Bisogno G, Gandola L et al (2011) A prospective protocol for nasopharyngeal carcinoma in children and adolescents: the Italian Rare Tumors in Pediatric Age (TREP) project. Cancer 118(10):2718–2725
Yan Z, Xia L, Huang Y et al (2013) Nasopharyngeal carcinoma in children and adolescents in an endemic area: a report of 185 cases. Int J Pediatr Otorhinolaryngol 77(9):1454–1460
Tao CJ, Liu X, Tang LL et al (2013) Long-term outcome and late toxicities of simultaneous integrated boost-intensity modulated radiotherapy in pediatric and adolescent nasopharyngeal carcinoma. Chin. J Cancer 32(10):525–532
Wu SG, Liao XL, He ZY et al (2017) Demographic and clinicopathological characteristics of nasopharyngeal carcinoma and survival outcomes according to age at diagnosis: A population-based analysis. Oral Oncol 73:83–87
Gioacchini FM, Tulli M, Kaleci S et al (2017) Therapeutic modalities and oncologic outcomes in the treatment of T1b glottic squamous cell carcinoma: a systematic review. Eur Arch Otorhinolaryngol 274(12):4091–4102
Buehrlen M, Zwaan CM, Granzen B et al (2012) Multimodal treatment, including interferon beta, of nasopharyngeal carcinoma in children and young adults: preliminary results from the prospective, multicenter study NPC-2003-GPOH/DCOG. Cancer 118(19):4892–4900
Sahai P, Mohanti BK, Sharma A et al (2017) Clinical outcome and morbidity in pediatric patients with nasopharyngeal cancer treated with chemoradiotherapy. Pediatr Blood Cancer 64(2):259–266
Guo Q, Cui X, Lin S et al (2016) Locoregionally advanced nasopharyngeal carcinoma in childhood and adolescence: Analysis of 95 patients treated with combined chemotherapy and intensity-modulated radiotherapy. Head Neck 38(Suppl 1):E665–672
Daoud J, Ghorbal L, Siala W et al (2013) Is there any difference in therapeutic results of nasopharyngeal carcinoma between adults and children? Cancer Radiother 17(8):763–767
Mertens R, Granzen B, Lassay L et al (2005) Treatment of nasopharyngeal carcinoma in children and adolescents: definitive results of a multicenter study (NPC-91-GPOH). Cancer 104(5):1083–1089
Casanova M, Ozyar E, Patte C et al (2016) International randomized phase 2 study on the addition of docetaxel to the combination of cisplatin and 5‑fluorouracil in the induction treatment for nasopharyngeal carcinoma in children and adolescents. Cancer Chemother Pharmacol 77(2):289–298
Qiu WZ, Peng XS, Xia HQ et al (2017) A retrospective study comparing the outcomes and toxicities of intensity-modulated radiotherapy versus two-dimensional conventional radiotherapy for the treatment of children and adolescent nasopharyngeal carcinoma. J Cancer Res Clin Oncol 143(8):1563–1572
Edge S, Byrd D, Compton C et al (2010) AJCC cancer staging handbook AJCC cancer staging manual, 7th edn. Springer, New York, pp 63–79
Miller AB, Hoogstraten B, Staquet M et al (1981) Reporting results of cancer treatment. Cancer 47(1):207–214
Reguerre Y, Lacour B, Andre N et al (2010) Epidemiology and management of rare paediatric tumours within the framework of the French Society for Children Cancer. Bull Cancer 97(9):1041–1045
Brock PR, Bellman SC, Yeomans EC et al (1991) Cisplatin ototoxicity in children: a practical grading system. Med Pediatr Oncol 19(4):295–300
Kaplan E, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:467–471
Rodriguez-Galindo C, Wofford M, Castleberry RP et al (2005) Preradiation chemotherapy with methotrexate, cisplatin, 5‑fluorouracil, and leucovorin for pediatric nasopharyngeal carcinoma. Cancer 103(4):850–857
Kontny U, Franzen S, Behrends U et al (2016) Diagnosis and treatment of Nasopharyngeal carcinoma in children and adolescents—recommendations of the GPOH-NPC study group. Klin Padiatr 228(3):105–112
Lee AW, Lin JC, Ng WT (2012) Current management of nasopharyngeal cancer. Semin Radiat Oncol 22(3):233–244
Gioacchini FM, Tulli M, Kaleci S et al (2017) Prognostic aspects in the treatment of juvenile nasopharyngeal carcinoma: a systematic review. Eur Arch Otorhinolaryngol 274(3):1205–1214
Laskar S, Sanghavi V, Muckaden MA et al (2004) Nasopharyngeal carcinoma in children: ten years’ experience at the Tata Memorial Hospital, Mumbai. Int J Radiat Oncol Biol Phys 58(1):189–195
Wolden SL, Steinherz PG, Kraus DH et al (2000) Improved long-term survival with combined modality therapy for pediatric nasopharynx cancer. Int J Radiat Oncol Biol Phys 46(4):859–864
Ozyar E, Selek U, Laskar S et al (2006) Treatment results of 165 pediatric patients with non-metastatic nasopharyngeal carcinoma: a Rare Cancer Network study. Radiother Oncol 81(1):39–46
Guruprasad B, Tanvir P, Rohan B et al (2013) Paediatric nasopharyngeal carcinoma: an 8‑year study from a tertiary care cancer centre in South India. Indian J Otolaryngol Head Neck Surg 65(Suppl 1):131–134
Cheuk DK, Billups CA, Martin MG et al (2011) Prognostic factors and long-term outcomes of childhood nasopharyngeal carcinoma. Cancer 117(1):197–206
Liu T (1999) Issues in the management of nasopharyngeal carcinoma. Crit Rev Oncol Hematol 31(1):55–69
Laskar S, Bahl G, Muckaden M et al (2008) Nasopharyngeal carcinoma in children: comparison of conventional and intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 72(3):728–736
Liu W, Tang Y, Gao L et al (2014) Nasopharyngeal carcinoma in children and adolescents—a single institution experience of 158 patients. Radiat Oncol 9:274
Sultan I, Casanova M, Ferrari A et al (2010) Differential features of nasopharyngeal carcinoma in children and adults: a SEER study. Pediatr Blood Cancer 55(2):279–284
Lin H, Huang S, Deng X et al (2014) Comparison of 3D anatomical dose verification and 2D phantom dose verification of IMRT/VMAT treatments for nasopharyngeal carcinoma. Radiat Oncol 9:71
Zhang MX, Li J, Shen GP et al (2015) Intensity-modulated radiotherapy prolongs the survival of patients with nasopharyngeal carcinoma compared with conventional two-dimensional radiotherapy: A 10-year experience with a large cohort and long follow-up. Eur J Cancer 51(17):2587–2595
Chen JL, Huang YS, Kuo SH et al (2017) Intensity-modulated radiation therapy achieves better local control compared to three-dimensional conformal radiation therapy for T4-stage nasopharyngeal carcinoma. Oncotarget 8(8):14068–14077
Peng G, Wang T, Yang KY et al (2012) A prospective, randomized study comparing outcomes and toxicities of intensity-modulated radiotherapy vs. conventional two-dimensional radiotherapy for the treatment of nasopharyngeal carcinoma. Radiother Oncol 104(3):286–293
Widesott L, Pierelli A, Fiorino C et al (2008) Intensity-modulated proton therapy versus helical tomotherapy in nasopharynx cancer: planning comparison and NTCP evaluation. Int J Radiat Oncol Biol Phys 72(2):589–596
Lewis GD, Holliday EB, Kocak-Uzel E et al (2016) Intensity-modulated proton therapy for nasopharyngeal carcinoma: Decreased radiation dose to normal structures and encouraging clinical outcomes. Head Neck 38(Suppl 1):E1886–1895
Taheri-Kadkhoda Z, Bjork-Eriksson T, Nill S et al (2008) Intensity-modulated radiotherapy of nasopharyngeal carcinoma: a comparative treatment planning study of photons and protons. Radiat Oncol 3:4
Shaw PH, Reed DR, Yeager N et al (2015) Adolescent and young adult (AYA) oncology in the united states: a specialty in its late adolescence. J Pediatr Hematol Oncol 37(3):161–169
Downs-Canner S, Shaw PH (2009) A comparison of clinical trial enrollment between adolescent and young adult (AYA) oncology patients treated at affiliated adult and pediatric oncology centers. J Pediatr Hematol Oncol 31(12):927–929
Keegan TH, Ries LA, Barr RD et al (2016) Comparison of cancer survival trends in the United States of adolescents and young adults with those in children and older adults. Cancer 122(7):1009–1016
Cash T, Qayed M, Ward KC et al (2015) Comparison of survival at adult versus pediatric treatment centers for rare pediatric tumors in an adolescent and young adult (AYA) population in the State of Georgia. Pediatr Blood Cancer 62(3):456–462
Sun Y, Li WF, Chen NY et al (2016) Induction chemotherapy plus concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a phase 3, multicentre, randomised controlled trial. Lancet Oncol 17(11):1509–1520
Baujat B, Audry H, Bourhis J et al (2006) Chemotherapy as an adjunct to radiotherapy in locally advanced nasopharyngeal carcinoma. Cochrane Database Syst Rev 4:CD4329
Blanchard P, Lee A, Marguet S et al (2015) Chemotherapy and radiotherapy in nasopharyngeal carcinoma: an update of the MAC-NPC meta-analysis. Lancet Oncol 16(6):645–655
Ribassin-Majed L, Marguet S, Lee AWM et al (2017) What is the best treatment of locally advanced Nasopharyngeal carcinoma? An individual patient data network meta-analysis. J Clin Oncol 35(5):498–505
Machtay M, Moughan J, Trotti A et al (2008) Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol 26(21):3582–3589
Hong M, Tang K, Qian J et al (2018) Immunotherapy for EBV-Associated Nasopharyngeal Carcinoma. Crit Rev Oncog 23(3–4):219–234
Acknowledgements
The French Fracture database is supported by the “Enfants, cancers et Santé” association who did not take part in any analyses of this study. We thank Dr G. Schleiermacher for the editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Jouin, S. Helfre, S. Bolle, L. Claude, A. Laprie, E. Bogart, C. Vigneron, H. Potet, A. Ducassou, A. Claren, F.G. Riet, M.P. Castex, C. Faure-Conter, B. Fresneau, A.S. Defachelles, and D. Orbach declare no actual or potential conflict of interest including any financial, personal or other relationships with other people or organizations that could inappropriately influence (bias) their work.
Caption Electronic Supplementary Material
66_2019_1461_MOESM2_ESM.docx
ONLINE RESOURCE 3: SUPPLEMENTAL TABLE ST2. Long-term head and neck severe morbidities with comparison between patients treated with 3D-RT and those treated with IMRT
66_2019_1461_MOESM4_ESM.doc
ONLINE RESOURCE 4: SUPPLEMENTAL FIGURE SF2. NPC French FRACTURE group proposals adapted to the response to induction chemotherapy
Rights and permissions
About this article
Cite this article
Jouin, A., Helfre, S., Bolle, S. et al. Adapted strategy to tumor response in childhood nasopharyngeal carcinoma: the French experience. Strahlenther Onkol 195, 504–516 (2019). https://doi.org/10.1007/s00066-019-01461-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01461-6