Abstract
Purpose
Little is known about the attitudes of radiation oncologists towards palliative care, about their competences in this field, and about the collaboration with palliative care specialists. Our aim was to close this gap and understand more about the importance of an additional qualification in palliative care.
Methods
Medical members of the German Society for Radiation Oncology (DEGRO) were electronically surveyed during November–December 2016.
Results
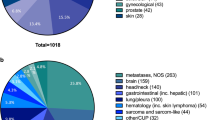
The survey was emailed successfully to 1110 addressees, whereas a total of 205 questionnaires were eligible for analysis (response rate 18.4%). 55 (26.8%) of the respondents had an additional qualification in palliative care. Physicians who had an additional qualification in palliative care (PC qualification) reported palliative care needs for their patients more frequently than the other respondents (89.0 vs. 82.7%, p = 0.008). Furthermore, they were most likely to report a high confidence in palliative care competences, such as “communication skills & support for relatives” (83.6 vs. 59.3%, p = 0.013), “symptom control,” and “pain management” (94.5 vs. 67.7%, p < 0.001 and 90.9 vs. 73.3%, p = 0.008, respectively). Respondents with a PC qualification more often involved palliative care specialists than the other respondents (63.3 vs. 39.3%, p = 0.007). Perceived main barriers regarding palliative care in radiation oncology included time aspects (9.2%), stigmata (8.5%), and the lack of interdisciplinary collaboration (8.5%).
Conclusions
This analysis demonstrated that aspects of palliative care strongly impact on daily practice in radiation oncology. Additional qualifications and comprehensive training in palliative medicine may contribute to improved patient care in radiation oncology.
Zusammenfassung
Zielsetzung
Wenig ist bisher über die Einstellungen der Strahlentherapeuten gegenüber der Palliativmedizin, über ihre Kompetenzen und über die Zusammenarbeit der Strahlentherapeuten mit den Palliativmedizinern bekannt. Ziel ist es, diese Lücke zu schließen und mehr über die Bedeutung der Zusatzbezeichnung Palliativmedizin (ZPM) herauszufinden.
Methoden
Ärztliche Mitglieder der Deutschen Gesellschaft für Radioonkologie (DEGRO) wurden im Zeitraum von November bis Dezember 2016 elektronisch befragt.
Ergebnisse
Der Fragebogen wurde erfolgreich an 1110 DEGRO-Mitglieder gesendet, während 205 Fragebögen vollständig beantwortet wurden (Rücklaufquote 18,4 %). Von den Teilnehmern hatten 55 (26,8 %) die ZPM. Befragte mit ZPM fühlten sich signifikant häufiger sicher in palliativmedizinischen Fähigkeiten, wie z. B. im Gespräch über das Thema „keine lebensverlängernden Maßnahmen“ (89,0 % vs. 74,1 %; p < 0,001), im Überbringen schlechter Nachrichten (85,4 % vs. 59,3 %; p = 0,009), in der Gesprächsführung und psychischen Unterstützung der Angehörigen (83,6 % vs. 59,3 %; p = 0,013), in der Symptomkontrolle (94,5 % vs. 67,7 %; p < 0,001) und in der Schmerztherapie (90,9 % vs. 73,3 %; p = 0,008). Teilnehmer mit ZPM bezogen öfter Palliativmediziner in ihre Behandlung mit ein als Strahlentherapeuten ohne palliativmedizinische Weiterbildung (63,3 % vs. 39,3 %; p = 0,007). Die häufigsten genannten Barrieren waren Zeitaspekte (9,2 %), Stigmata (8,5 %) und die interdisziplinäre Zusammenarbeit (8,5 %).
Schlussfolgerung
Die vorliegende Studie zeigt, dass die Palliativversorgung einen hohen Stellenwert im Praxisalltag der Strahlentherapeuten hat. Zusätzliche Qualifikationen und klinisches Training in der Palliativmedizin können zu einer verbesserten Patientenversorgung in der Strahlentherapie beitragen.

Similar content being viewed by others
Abbreviations
- ASCO:
-
American Society of Clinical Oncology
- ASTRO:
-
American Society for Radiation Oncology
- DEGRO:
-
Deutsche Gesellschaft für Radioonkologie—German Society for Radiation Oncology
- DGP:
-
Deutsche Gesellschaft für Palliativmedizin—German Society for Palliative Care
- ESMO:
-
European Society for Medical Oncology
References
Jones JA, Lutz ST, Chow E, Johnstone PA (2014) Palliative radiotherapy at the end of life: a critical review. CA Cancer J Clin 64(5):295–310
Lutz S, Chow E (2014) Palliative radiotherapy: past, present and future-where do we go from here? Ann Palliat Med 3(4):286–290
Körner P, Ehrmann K, Hartmannsgruber J, Metz M, Steigerwald S, Flentje M et al (2017) Patient-reported symptoms during radiotherapy. Strahlenther Onkol 193(7):570–577
van Oorschot B, Schuler M, Simon A, Schleicher U, Geinitz H (2011) Patterns of care and course of symptoms in palliative radiotherapy. Strahlenther Onkol 187(8):461–466
Murphy JD, Nelson LM, Chang DT, Mell LK, Le Q‑T (2013) Patterns of care in palliative radiotherapy: a population-based study. J Oncol Pract 9(5):e220–e227
Parker GM, LeBaron VT, Krishnan M, Shiloh RY, Spektor A, Hertan L et al (2017) Burden of palliative care issues encountered by radiation oncologists caring for patients with advanced cancer. Pract Radiat Oncol 7(6):e517–e524
Yamaguchi S, Ohguri T, Matsuki Y, Yahara K, Narisada H, Imada H et al (2013) Palliative radiotherapy in patients with a poor performance status: the palliative effect is correlated with prolongation of the survival time. Radiat Oncol 8(1):166
Bickel KE, McNiff K, Buss MK, Kamal A, Lupu D, Abernethy AP et al (2016) Defining high-quality palliative care in oncology practice: an American Society of Clinical Oncology/American Academy of Hospice and Palliative Medicine guidance statement. J Oncol Pract 12(9):e828–e838
Morrison RS, Dietrich J, Ladwig S, Quill T, Sacco J, Tangeman J et al (2011) Palliative care consultation teams cut hospital costs for medicaid beneficiaries. Health Aff 30(3):454–463
Smith TJ, Temin S, Alesi ER, Abernethy AP, Balboni TA, Basch EM et al (2012) American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol 30(8):880–887
Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA et al (2010) Early palliative care for patients with metastatic non-small-cell lung. Cancer 8(19). https://doi.org/10.1056/NEJMoa1000678
Dalgaard KM, Bergenholtz H, Nielsen ME, Timm H (2014) Early integration of palliative care in hospitals: a systematic review on methods, barriers, and outcome. Palliat Support Care 12(6):495–513
Wentlandt K, Krzyzanowska MK, Swami N, Rodin GM, Le LW, Zimmermann C (2012) Referral practices of oncologists to specialized palliative care. J Clin Oncol 30(35):4380–4386
Finn L, Green AR, Malhotra S (2017) Oncology and palliative medicine: providing comprehensive care for patients with cancer. Ochsner J 17(4):393–397
Leitlinienprogramm Onkologie, Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF (2015) Palliativmedizin für Patienten mit einer nicht heilbaren Krebserkrankung, Langversion 1.0, pp 1–265
Jordan K, Aapro M, Kaasa S, Ripamonti CI, Scotté F, Strasser F et al (2018) European Society for Medical Oncology (ESMO) position paper on supportive and palliative care. Ann Oncol 29(1):36–43
Momm F, Becker G, Ewald H, Baumgartner J, Adamietz IA, Frommhold H (2004) Participation of radiotherapy in interdisciplinary palliative care units—challenge and chance. Strahlenther Onkol 180(2):73–77
Momm F, Lingg S, Xander C, Adebahr S, Grosu A‑L, Becker G (2010) Die Situation der Angehörigen von Strahlentherapiepatienten. Strahlenther Onkol 186(6):344–350
Nieder C, Dalhaug A, Pawinski A, Haukland E, Mannsåker B, Engljähringer K (2015) Palliative radiotherapy with or without additional care by a multidisciplinary palliative care team in patients with newly diagnosed cancer: a retrospective matched pairs comparison. Radiat Oncol 10(1):61
Cleeland CS, Janjan NA, Scott CB, Seiferheld WF, Curran WJ (2000) Cancer pain management by radiotherapists: a survey of radiation therapy oncology group physicians. Int J Radiat Oncol Biol Phys 47(1):203–208
Krishnan M, Racsa M, Jones J, Chittenden E, Schaefer KG, Spektor A et al (2017) Radiation oncology resident palliative education. Pract Radiat Oncol 7(6):e439–e448
Wei RL, Mattes MD, Yu J, Thrasher A, Shu H‑K, Paganetti H et al (2017) Attitudes of radiation oncologists toward palliative and supportive care in the United States: report on national membership survey by the American Society for Radiation Oncology (ASTRO). Pract Radiat Oncol 7(2):113–119
Odejide OO, Salas Coronado DY, Watts CD, Wright AA, Abel GA (2014) End-of-life care for blood cancers: a series of focus groups with hematologic oncologists. J Oncol Pract 10(6):e396–e403
Wei RL, Colbert LE, Jones J, Racsa M, Kane G, Lutz S et al (2017) Palliative care and palliative radiation therapy education in radiation oncology: a survey of US radiation oncology program directors. Pract Radiat Oncol 7(4):234–240
Mayring P (2000) Qualitative Inhaltsanalyse. Qual Soc Res (Online Journal), 1(2):10
Pifer PM, Farrugia MK, Mattes MD (2018) Comparative analysis of the views of oncologic subspecialists and palliative/supportive care physicians regarding advanced care planning and end-of-life care. Am J Hosp Palliat Med. https://doi.org/10.1177/1049909118763592
Buckley de Meritens A, Margolis B, Blinderman C, Prigerson HG, Maciejewski PK, Shen MJ et al (2017) Practice patterns, attitudes, and barriers to palliative care consultation by gynecologic oncologists. J Oncol Pract 13(9):e703–e711
Dalberg T, McNinch NL, Friebert S (2018) Perceptions of barriers and facilitators to early integration of pediatric palliative care: a national survey of pediatric oncology providers. Pediatr Blood Cancer 65:e26996
Eskander RN, Osann K, Dickson E, Holman LL, Rauh-Hain JA, Spoozak L et al (2014) Assessment of palliative care training in gynecologic oncology: a gynecologic oncology fellow research network study. Gynecol Oncol 134(2):379–384. https://doi.org/10.1016/j.ygyno.2014.05.021
Gu X, Cheng W (2016) Chinese oncologists’ knowledge, attitudes and practice towards palliative care and end of life issues. BMC Med Educ 16:149
Hay CM, Lefkowits C, Crowley-Matoka M, Bakitas MA, Clark LH, Duska LR et al (2017) Strategies for introducing outpatient specialty palliative care in gynecologic oncology. J Oncol Pract 13(9):e712–e720
Odejide OO, Cronin AM, Condron NB, Fletcher SA, Earle CC, Tulsky JA et al (2016) Barriers to quality end-of-life care for patients with blood cancers. J Clin Oncol. https://doi.org/10.1200/jco.2016.67.8177
Snyder S, Hazelett S, Allen K, Radwany S (2013) Physician knowledge, attitude, and experience with advance care planning, palliative care, and hospice. Am J Hosp Palliat Med 30(5):419–424
Thomas RA, Curley B, Wen S, Zhang J, Abraham J, Moss AH (2015) Palliative care training during fellowship: a national survey of U.S. hematology and oncology fellows. J Palliat Med 18(9):747–751
Wong A, Reddy A, Williams JL, Wu J, Liu D, Bruera E et al (2016) ReCAP: attitudes, beliefs, and awareness of graduate medical education trainees regarding palliative care at a comprehensive cancer center. J Oncol Pract 12(2):149–150
Quill TE, Abernethy AP (2013) Generalist plus specialist palliative care—creating a more sustainable model. N Engl J Med 368(13):1173–1175
Hui D, Park M, Liu D, Reddy A, Dalal S, Bruera E (2015) Attitudes and beliefs toward supportive and palliative care referral among hematologic and solid tumor oncology specialists. Oncologist 20(11):1326–1332
Onkologie L, Deutsche Krebsgesellschaft, Deutsche Krebshilfe (2015) S3-Leitlinie Palliativmedizin für Patienten mit einer nicht heilbaren Krebserkrankung
Jones JA, Lutz ST, Chow E, Johnstone PA (2014) Palliative radiotherapy at the end of life: a critical review. CA Cancer J Clin 64(5):296–310
Sharma S, Hertan L, Jones J (2014) Palliative radiotherapy: current status and future directions. Semin Oncol 41(6):751–763
Fairchild A, Ghosh S, Baker J (2012) Patterns of referral and knowledge of palliative radiotherapy in Alberta. Can Fam Physician 58:113–122
Danielson B, Fairchild A (2012) Beyond palliative radiotherapy: a pilot multidisciplinary brain metastases clinic. Support Care Cancer 20(4):773–781
Schroder C, Heyland D, Jiang X, Rocker G, Dodek P (2009) Canadian researchers at the end of life network. Educating medical residents in end-of-life care: insights from a multicenter survey. J Palliat Med 12(5):459–470
Oneschuk D, Fainsinger R, Hanson J, Bruera E (1997) Assessment and knowledge in palliative care in second year family medicine residents. J Pain Symptom Manage 14(5):265–273
Hui D, Finlay E, Buss MK, Prommer EE, Bruera E (2015) Palliative oncologists: specialists in the science and art of patient care. J Clin Oncol 33(20):2314–2317
Hannon B, Swami N, Pope A, Rodin G, Dougherty E, Mak E et al (2015) The oncology palliative care clinic at the Princess Margaret Cancer Centre: an early intervention model for patients with advanced cancer. Support Care Cancer 23(4):1073–1080
Mitin T, Thomas CR, Jaboin JJ (2017) PRADO: a palliative care model for every radiation oncology practice. Int J Radiat Oncol Biol Phys 99(3):518–519
Back AL, Arnold RM, Baile WF, Fryer-Edwards KA, Alexander SC, Barley GE et al (2007) Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 167:453–460
Kellerman SE, Herold J (2001) Physician response to surveys: a review of the literature. Am J Prev Med 20(1):61–67
Martins Y, Lederman R, Lowenstein C, Joffe S, Neville B, Hastings B et al (2012) Increasing response rates from physicians in oncology research: a structured literature review and data from a recent physician survey. Br J Cancer 106:1021–102628
Kalies H, Schöttmer R, Simon ST, Voltz R, Crispin A, Bausewein C (2018) Barriers for the implementation of guidelines in palliative care—results from a national survey of professionals. Support Care Cancer. https://doi.org/10.1007/s00520-017-4030-z
Koontz BF, Benda R, De Los Santos J, Hoffman KE, Saiful Huq M, Morrell R et al (2016) US radiation oncology practice patterns for posttreatment survivor care. Pract Radiat Oncol. https://doi.org/10.1016/j.prro.2015.10.002
Semrau R, Hansemann K, Adam M, Andratschke N, Brunner T, Heinzelmann F et al (2008) Quality of training in radiation oncology in Germany. Results of a 2006 survey. Strahlenther Onkol 184(5):239–244
Dunning D, Heath C, Suls JM (2004) Flawed self-assessment implications for health, education, and the workplace. Psychol Sci Public Interest 5(3):69–106
Acknowledgements
We would like to thank the German Society for Radiation Oncology (DEGRO) office team for providing the mailing list and data of the basic population.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Fels, S. Pigorsch, H. Vorwerk, R. Engenhart-Cabillic, and B. van Oorschot declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Rights and permissions
About this article
Cite this article
Fels, J., Pigorsch, S., Vorwerk, H. et al. Palliative care in everyday practice of radiation oncologists. Strahlenther Onkol 195, 659–667 (2019). https://doi.org/10.1007/s00066-018-1403-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1403-2