Abstract
Purpose and objective
To test the hypothesis that a rectal and bladder preparation protocol is associated with an increase in prostate cancer specific survival (PCSS), clinical disease free survival (CDFS) and biochemical disease free survival (BDFS).
Patients and methods
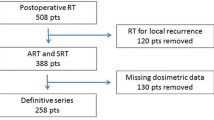
From 1999 to 2012, 1080 prostate cancer (PCa) patients were treated with three-dimensional conformal radiotherapy (3DCRT). Of these patients, 761 were treated with an empty rectum and comfortably full bladder (RBP) preparation protocol, while for 319 patients no rectal/bladder preparation (NRBP) protocol was adopted.
Results
Compared with NRBP patients, patients with RBP had significantly higher BDFS (64% vs 48% at 10 years, respectively), CDFS (81% vs 70.5% at 10 years, respectively) and PCSS (95% vs 88% at 10 years, respectively) (log-rank test p < 0.001). Multivariate analysis (MVA) indicated for all treated patients and intermediate high-risk patients that the Gleason score (GS) and the rectal and bladder preparation were the most important prognostic factors for PCSS, CDFS and BDFS. With regard to high- and very high-risk patients, GS, RBP, prostate cancer staging and RT dose were predictors of PCSS, CDFS and BDFS in univariate analysis (UVA).
Conclusion
We found strong evidence that rectal and bladder preparation significantly decreases biochemical and clinical failures and the probability of death from PCa in patients treated without daily image-guided prostate localization, presumably since patients with RBP are able to maintain a reproducibly empty rectum and comfortably full bladder across the whole treatment compared with NRPB patients.
Zusammenfassung
Ziel
Prüfung der Hypothese, dass ein Rektum-Blasen-Vorbereitungsprotokoll mit einer Zunahme des prostatakarzinomspezifischen Überlebens (PCSS), des klinisch krankheitsfreien Überlebens (CDFS) und des biochemisch krankheitsfreien Überlebens (BDFS) verbunden ist.
Patienten und Methoden
Von 1999 bis 2012 erhielten 1080 Patienten mit Prostatakarzinom eine 3‑dimensional geplante Strahlentherapie. Bei 761 Patienten wurde ein Vorbereitungsprotokoll mit leerem Rektum und angenehm voller Blase (Rektum-Blasen-Vorbereitung [RBV]) angewendet, bei den weiteren 319 Patienten kam kein Protokoll zur Vorbereitung von Rektum und Blase (NRBV) zur Anwendung.
Ergebnisse
Patienten mit RBV hatten im Vergleich zu NRBV-Patienten ein signifikant höheres BDFS (64 % vs. 48 % nach 10 Jahren), CDFS (81 % vs. 70,5 % nach 10 Jahren) und PCSS (95 % vs. 88 % nach 10 Jahren; log-Rang-Test p < 0,001). Die multivariate Analyse (MVA) aller behandelten Patienten und der Patienten mit moderat hohem Risiko zeigte, dass der Gleason-Score (GS) und die Rektum-Blasen-Vorbereitung die wichtigsten prognostischen Faktoren des PCSS, CDFS und BDFS waren. Hinsichtlich der Patienten mit hohem und sehr hohem Risiko waren in der univariaten Analyse (UVA) GS, RBV, Prostatakarzinom-Staging und Strahlentherapiedosis Prädiktoren für PCSS, CDFS und BDFS.
Schlussfolgerung
Wie unsere Studie deutlich belegt, verringert die RBV signifikant die biochemischen und klinischen Rückfälle und die Wahrscheinlichkeit eines prostatakarzinombedingten Tods bei Patienten ohne tägliche bildgeführte Prostatalokalisierung, vermutlich weil die Patienten mit RBV im Vergleich zu NRBV-Patienten während der gesamten Behandlung reproduzierbar ein leeres Rektum und eine angenehm volle Blase haben.



Similar content being viewed by others
References
Zelefsky MJ, Leibel SA, Gaudin PB et al (1998) Dose escalation with three-dimensional conformal radiation therapy affects the outcome in prostate cancer. Int J Radiat Oncol Biol Phys 41:491–500
Antolak JA, Rosen II, Childress CH et al (1998) Prostate target volume variations during a course of radiotherapy. Int J Radiat Oncol Biol Phys 42:661–672
Zelefsky MJ, Crean D, Mageras GS et al (1999) Quantification and predictors of prostate position variability in 50 patients evaluated with multiple CT scans during conformal radiotherapy. Radiother Oncol 50:225–234
Van Herk M, Bruce A, Kroes AP et al (1995) Quantification of organ motion during conformal radiotherapy of the prostate by three dimensional image registration. Int J Radiat Oncol Biol Phys 33:1311–1320
Balter JM, Sandler HM, Lam K et al (1995) Measurement of prostate movement over the course of routine radiotherapy using implanted markers. Int J Radiat Oncol Biol Phys 31:113–118
Stroom JC, Koper PC, Korevaar GA et al (1999) Internal organ motion in prostate cancer patients treated in prone and supine treatment position. Radiother Oncol 51:237–248
Rudat V, Schraube P, Oetzel D et al (1996) Combined error of patient positioning variability and prostate motion uncertainty in 3D conformal radiotherapy of localized prostate cancer. Int J Radiat Oncol Biol Phys 35:1027–1034
Nguyen T, Boldt RG, Rodrigues G (2015) Prognostic factors for prostate cancer endpoints following biochemical failure: a review of the literature. Cureus 7(1):e238
Zelefsky MJ, Pei X, Chou JF, Schechter M, Kollmeier M, Cox B, Yamada Y, Fidaleo A, Sperling D, Happersett L, Zhang Z (2011) Dose escalation for prostate cancer radiotherapy: predictors of long-term biochemical tumor control and distant metastases-free survival outcomes. Eur Urol 60(6):1133–1139
Zelefsky MJ, Yamada Y, Fuks Z, Zhang Z, Hunt M, Cahlon O, Park J, Shippy A (2008) Long-term results of conformal radiotherapy for prostate cancer: impact of dose escalation on biochemical tumor control and distant metastases-free survival outcomes. Int J Radiat Oncol Biol Phys 71(4):1028–1033
Heemsberg W, Hoogeman M, Witte M et al (2007) Increased risk of biochemical and clinical failure for prostate patients with a large rectum at radiotherapy planning: results from the Dutch trial of 68 Gy versus 78 Gy. Int J Radiat Oncol Biol Phys 67(5):1418–1424
de Crevoisier R, Tucker S, Dong L et al (2005) Increased risk of biochemical and local failure in patients with distended rectum on the planning CT for prostate cancer radiotherapy. Int J Radiat Oncol Biol Phys 62(4):965–973
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick G, Tomaszewski J, Renshaw A, Kaplan I, Beard C, Wein A (1998) Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280:969–974
Antolak JA, Rosen II, Childress CH et al (1998) Prostate target volume variations during a course of radiotherapy. Int J Radiat Oncol Biol Phys 42:661–672
Chen ME, Johnston DA, Tang K et al (2000) Detailed mapping of prostate carcinoma foci: Biopsy strategy implications. Cancer 89:1800–1809
Greene DR, Wheeler TM, Egawa S et al (1991) Relationship between clinical stage and histological zone of origin in early prostate cancer: Morphometric analysis. Br J Urol 68:499–509
Schultheiss TE, Lee WR, Hunt MA et al (1997) Late GI and GU complications in the treatment of prostate cancer. Int J Radiat Oncol Biol Phys 37:3–11
Jackson A, Skwarchuk MW, Zelefsky MJ (2001) Late rectal bleeding after conformal radiotherapy of prostate cancer. II. Volume effects and dose-volume histograms. Int J Radiat Oncol Biol Phys 49:685–698
Lee WR, Hanks GE, Hanlon AL et al (1996) Lateral rectal shielding reduces late rectal morbidity following high-dose three dimensional conformal radiation therapy for clinically localized prostate cancer: Further evidence for a significant dose effect. Int J Radiat Oncol Biol Phys 35:251–257
O’Doherty UM, McNair HA, Norman AR et al (2006) Variability of bladder filling in patients receiving radical radiotherapy to the prostate. Radiother Oncol 79(3):335–340
Stasi M, Munoz F, Fiorino C et al (2006) Emptying the rectum before treatment delivery limits the variations of rectal dose – volume parameters during 3DCRT of prostate cancer. Radiother Oncol 80(3):363–370
Gleason DF (1977) The veterans administrative cooperative urologic research group. Histological grading and clinical staging of prostatic carcinoma. Urologic Pathology: The prostate. Lea and Febiger, Philadelphia, pp 171–198
Sogani PC, Israel A, Lieberman PH, Lesser ML, Whitmore WF (1985) Gleason grading of prostate cancer: a predictor of survival. Urology 25:223–227
Björk T, Lilja H, Christensson A (1999) The prognostic value of different forms of prostate specific antigen and their ratios in patients with prostate cancer. BJU Int 84(9):1021–1027
Gabriele D, Jereczek-Fossa BA, Krengli M et al (2016) Beyond D’Amico risk classes for predicting recurrence after external beam radiotherapy for prostate cancer: the Candiolo classifier. Radiat Oncol 11(1):23–24. doi:10.1186/s13014-016-0599-5
Karlsdottir A, Muren LP, Wentzel-Larsen T et al (2009) Outcome in intermediate or high risk prostate cancer patients receiving radiation dose and hormone therapy. Acta Oncol 48(6):874–881. doi:10.1080/02841860902974159
Park SS, Yan D, McGrath S et al (2012) Adaptive image-guided radiotherapy (IGRT) eliminates the risk of biochemical failure caused by the bias of rectal distension in prostate cancer treatment planning: clinical evidence. Int J Radiat Oncol Biol Phys 83(3):947–952
Kupelian PA, Willoughby TR, Reddy CA et al (2008) Impact of image guidance on outcomes after external beam radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 70(4):1146–1150
Edge S, Byrd D, Compton C, Fritz A, Greene F, Trotti A (2010) AJCC cancer staging manual, 7th edn. Springer, New York NY
Albertsen PC, Hanley JA, Barrows GH et al (2005) Prostate cancer and the Will Rogers phenomenon. J Natl Cancer Inst 97(17):1248–1253
Gofrit ON, Zorn KC, Steinberg GD, Zagaja GP, Shalhav AL (2008) The Will Rogers phenomenon in urological oncology. J Urol 179:28–33
Zelefsky MJ, Fuks Z, Hunt M et al (2002) High-dose intensity modulated radiation therapy for prostate cancer: early toxicity and biochemical outcome in 772 patients. Int J Radiat Oncol Biol Phys 53(5):1111–1116
Zelefsky MJ, Fuks Z, Happersett L et al (2000) Clinical experience with intensity modulated radiation therapy (IMRT) in prostate cancer. Radiother Oncol 55:241–249
Michalski JM, Yan Y, Watkins-Bruner D et al (2013) Preliminary toxicity analysis of 3‑dimensional conformal radiation therapy versus intensity modulated radiation therapy on the high-dose arm of the Radiation Therapy Oncology Group 0126 prostate cancer trial. Int J Radiat Oncol Biol Phys 87:932–938
Sheets NC, Goldin GH, Meyer AM et al (2012) Intensity-modulated radiation therapy, proton therapy, or Conformal radiation therapy and morbidity and disease control in localized prostate cancer. JAMA 307(15):1611–1620
Arnaud A, Maingon P, Gauthier M et al (2014) Image-guided IMRT for localized prostate cancer with daily repositioning: Inferring the difference between planned dose and delivered dose distribution. Phys Med 30:669–675
Pollack A, Zagars GK, Smith LG et al (2000) Preliminary results of a randomized radiotherapy dose-escalation study comparing 70 Gy with 78 Gy for prostate cancer. J Clin Oncol 18(23):3904–3911
Funding
This work was supported by “5 per Mille 2009 Ministero della Salute-FPRC Onlus”. This work was also supported by the EUREKA-2 study, promoted by the CHIC project (Computational Horizons In Cancer, sponsored by the European Union, 7th Framework Program, grant agreement n. 600841).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Maggio, D. Gabriele, E. Garibaldi, S. Bresciani, E. Delmastro, A. Di Dia, A. Miranti, M. Poli, T. Varetto, M. Stasi and P. Gabriele declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Maggio, A., Gabriele, D., Garibaldi, E. et al. Impact of a rectal and bladder preparation protocol on prostate cancer outcome in patients treated with external beam radiotherapy. Strahlenther Onkol 193, 722–732 (2017). https://doi.org/10.1007/s00066-017-1163-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-017-1163-4