Abstract
Background
To evaluate complications and identify risk factors for adverse events in patients undergoing high-dose-rate interstitial brachytherapy (iBT).
Material and methods
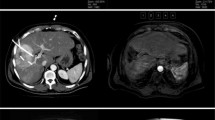
Data from 192 patients treated in 343 CT- or MRI-guided interventions from 2006–2009 at our institution were analyzed. In 41 %, the largest tumor treated was ≥ 5 cm, 6 % of the patients had tumors ≥ 10 cm. Prior to iBT, 60 % of the patients had chemotherapy, 22 % liver resection, 19 % thermoablation or transarterial chemoembolization (TACE). Safety was the primary endpoint; survival data were obtained as the secondary endpoints. During follow-up, MRI or CT imaging was performed and clinical and laboratory parameters were obtained.
Results
The rate of major complications was below 5 %. Five major bleedings (1.5 %) occurred. The frequency of severe bleeding was significantly higher in patients with advanced liver cirrhosis. One patient developed signs of a nonclassic radiation-induced liver disease. In 3 patients, symptomatic gastrointestinal (GI) ulcers were detected. A dose exposure to the GI wall above 14 Gy/ml was a reliable threshold to predict ulcer formation. A combination of C-reactive protein ≥ 165 mg/l and/or leukocyte count ≥ 12.7 Gpt/l on the second day after the intervention predicted infection (sensitivity 90.0 %; specificity 92.8 %.) Two patients (0.6 %) died within 30 days. Median overall survival after the first liver treatment was 20.1 months for all patients and the local recurrence-free surviving proportion was 89 % after 12 months.
Conclusions
Image-guided iBT yields a low rate of major complications and is effective.
Zusammenfassung
Hintergrund
Evaluierung der Komplikationsrate und Identifizierung von Risikofaktoren für Komplikationen und Nebenwirkungen bei Patienten mit Lebermalignomen, die mit der hochdosierten interstitiellen Brachytherapie (iBT) behandelt wurden.
Material und Methoden
Von 2006 bis 2009 wurden 192 Patienten in 343 CT- oder MRT-geführten Interventionen behandelt und deren Daten ausgewertet. Der größte behandelte Tumor war in 41% der Fälle ≥ 5 cm, 6% der Patienten hatten Tumoren ≥ 10 cm. Vor Behandlungsbeginn hatten 60% der Patienten eine Chemotherapie, 22% eine Leberesektion und 19% eine Thermoablation oder transarterielle Chemoembolisation (TACE). Primärer Endpunkt war die Behandlungssicherheit, als sekundäre Endpunkte wurden Überlebensdaten ausgewertet. Die Nachsorge umfasste neben klinischen und paraklinischen Parametern MRT- und CT-Untersuchungen.
Ergebnisse
Die Rate an Major-Komplikationen lag unter 5%. Es traten 5 behandlungsbedürftige Blutungen auf (1,5%). Die Häufigkeit schwerer Blutungen war bei Patienten mit Leberzirrhose im fortgeschrittenen Stadium signifikant höher. Ein Patient entwickelte Zeichen einer nichtklassischen Strahlenhepatitis. Bei 3 Patienten zeigten sich symptomatische Magen-Darm-Ulzera. Eine Dosisexposition der Magen- bzw. Duodenalschleimhaut von mehr als 14 Gy/ml Einzeitdosis war mit dem Risiko von radiogen bedingten Ulzera verbunden. Eine CRP-Erhöhung auf mehr als ≥ 165 mg/l und/oder ein Anstieg der Leukozytenzahl auf mehr als ≥12,7 Gpt/l am 2. postinterventionellen Tag wies auf eine Infektion hin (Sensitivität 90,0%; Spezifität 92,8%). Die 30-Tage-Mortalität betrug 0,6%. Das mediane Gesamtüberleben nach der ersten Leberbehandlung betrug 20,1 Monate, die Lokalrezidivfreiheit nach 12 Monaten lag bei 89%.
Schlussfolgerung
Die bildgeführte iBT hat eine niedrige Komplikationsrate und ist effektiv.



Similar content being viewed by others
References
Deshpande R, O’Reilly D, Sherlock D (2011) Improving outcomes with surgical resection and other ablative therapies in HCC. Int J Hepatol 2011:686074
Pawlik TM, Assumpcao L, Vossen JA et al (2009) Trends in nontherapeutic laparotomy rates in patients undergoing surgical therapy for hepatic colorectal metastases. Ann Surg Oncol 16:371–378
Dhir M, Lyden ER, Smith LM, Are C (2012) Comparison of outcomes of transplantation and resection in patients with early hepatocellular carcinoma: a meta-analysis. HPB (Oxford) 14:635–645
Jones RP, Jackson R, Dunne DF et al (2012) Systematic review and meta-analysis of follow-up after hepatectomy for colorectal liver metastases. Br J Surg 99:477–486
Smith MD, McCall JL (2009) Systematic review of tumour number and outcome after radical treatment of colorectal liver metastases. Br J Surg 96:1101–1113
Khatri VP, Petrelli NJ, Belghiti J (2005) Extending the frontiers of surgical therapy for hepatic colorectal metastases: is there a limit? J Clin Oncol 23:8490–8499
Cirocchi R, Trastulli S, Boselli C et al. Radiofrequency ablation in the treatment of liver metastases from colorectal cancer. Cochrane Database Syst Rev 6:CD006317
Ruers T, Punt C, Van Coevorden F et al (2012) Radiofrequency ablation combined with systemic treatment versus systemic treatment alone in patients with non-resectable colorectal liver metastases: a randomized EORTC Intergroup phase II study (EORTC 40004). Ann Oncol 23:2619–2626
Sutherland LM, Williams JA, Padbury RT, Gotley DC, Stokes B, Maddern GJ (2006) Radiofrequency ablation of liver tumors: a systematic review. Arch Surg 141:181–190
Tanis E, Nordlinger B, Mauer M et al (2014) Local recurrence rates after radiofrequency ablation or resection of colorectal liver metastases. Analysis of the European Organisation for Research and Treatment of Cancer #40004 and #40983. Eur J Cancer 50:912–919
Herfarth KK, Debus J, Lohr F et al (2001) Stereotactic single-dose radiation therapy of liver tumors: results of a phase I/II trial. J Clin Oncol 19:164–170
Bush DA, Kayali Z, Grove R, Slater JD (2011) The safety and efficacy of high-dose proton beam radiotherapy for hepatocellular carcinoma: a phase 2 prospective trial. Cancer 117:3053–3059
Kawashima M, Furuse J, Nishio T et al (2005) Phase II study of radiotherapy employing proton beam for hepatocellular carcinoma. J Clin Oncol 23:1839–1846
Dawson LA (2011) Overview: where does radiation therapy fit in the spectrum of liver cancer local-regional therapies? Semin Radiat Oncol 21:241–246
Scorsetti M, Arcangeli S, Tozzi A et al. Is stereotactic body radiation therapy an attractive option for unresectable liver metastases? A preliminary report from a phase 2 trial. Int J Radiat Oncol Biol Phys 2013;86:336–342
Dawood O, Mahadevan A, Goodman KA (2009) Stereotactic body radiation therapy for liver metastases. Eur J Cancer 45:2947–2959
Kirkpatrick JP, Kelsey CR, Palta M et al (2014) Stereotactic body radiotherapy: a critical review for nonradiation oncologists. Cancer 120:942–954
Ricke J, Wust P, Wieners G et al (2004) Liver malignancies: CT-guided interstitial brachytherapy in patients with unfavorable lesions for thermal ablation. J Vasc Interv Radiol 15:1279–1286
Mohnike K, Wieners G, Pech M et al (2009) Image-guided interstitial high-dose-rate brachytherapy in hepatocellular carcinoma. Dig Dis 27:170–174
Mohnike K, Wieners G, Schwartz F et al. (2010) Computed tomography-guided high-dose-rate brachytherapy in hepatocellular carcinoma: safety, efficacy, and effect on survival. Int J Radiat Oncol Biol Phys 78:172–179
Ricke J, Mohnike K, Pech M et al. (2010) Local response and impact on survival after local ablation of liver metastases from colorectal carcinoma by computed tomography-guided high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys 78:479–485
Collettini F, Poellinger A, Schnapauff D et al (2011) CT-guided high-dose-rate brachytherapy of metachronous ovarian cancer metastasis to the liver: initial experience. Anticancer Res 31:2597–2602
Collettini F, Schnapauff D, Poellinger A et al (2012) Hepatocellular carcinoma: computed-tomography-guided high-dose-rate brachytherapy (CT-HDRBT) ablation of large (5–7 cm) and very large (> 7 cm) tumours. Eur Radiol 22:1101–1109
Tselis N, Chatzikonstantinou G, Kolotas C, Milickovic N, Baltas D, Zamboglou N (2013) Computed tomography-guided interstitial high dose rate brachytherapy for centrally located liver tumours: a single institution study. Eur Radiol 23:2264–2270
Wieners G, Mohnike K, Peters N et al (2011) Treatment of hepatic metastases of breast cancer with CT-guided interstitial brachytherapy - a phase II-study. Radiother Oncol 100:314–319
Wieners G, Pech M, Hildebrandt B et al (2009) Phase II feasibility study on the combination of two different regional treatment approaches in patients with colorectal “liver-only” metastases: hepatic interstitial brachytherapy plus regional chemotherapy. Cardiovasc Intervent Radiol 32:937–945
Trotti A, Colevas AD, Setser A et al (2003) CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol 13:176–181
Lawrence TS, Robertson JM, Anscher MS, Jirtle RL, Ensminger WD, Fajardo LF (1995) Hepatic toxicity resulting from cancer treatment. Int J Radiat Oncol Biol Phys 31:1237–1248
Bertot LC, Sato M, Tateishi R, Yoshida H, Koike K (2011) Mortality and complication rates of percutaneous ablative techniques for the treatment of liver tumors: a systematic review. Eur Radiol 21:2584–2596
Cheung TT, Poon RT, Yuen WK et al (2013) Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg 257:506–511
Streitparth F, Pech M, Bohmig M et al (2006) In vivo assessment of the gastric mucosal tolerance dose after single fraction, small volume irradiation of liver malignancies by computed tomography-guided, high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys 65:1479–1486
Ruhl R, Seidensticker M, Peters N et al (2009) Hepatocellular carcinoma and liver cirrhosis: assessment of the liver function after Yttrium-90 radioembolization with resin microspheres or after CT-guided high-dose-rate brachytherapy. Dig Dis 27:189–199
Bujold A, Massey CA, Kim JJ et al (2013) Sequential phase I and II trials of stereotactic body radiotherapy for locally advanced hepatocellular carcinoma. J Clin Oncol 31:1631–1639
Kawashima M, Kohno R, Nakachi K et al (2011) Dose-volume histogram analysis of the safety of proton beam therapy for unresectable hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 79:1479–1486
Seidensticker M, Seidensticker R, Mohnike K et al (2011) Quantitative in vivo assessment of radiation injury of the liver using Gd-EOB-DTPA enhanced MRI: tolerance dose of small liver volumes. Radiat Oncol 6:40
Ricke J, Seidensticker M, Ludemann L et al (2005) In vivo assessment of the tolerance dose of small liver volumes after single-fraction HDR irradiation. Int J Radiat Oncol Biol Phys 62:776–784
Ruhl R, Ludemann L, Czarnecka A et al (2010) Radiobiological restrictions and tolerance doses of repeated single-fraction hdr-irradiation of intersecting small liver volumes for recurrent hepatic metastases. Radiat Oncol 5:44
Brinkhaus G, Lock JF, Malinowski M et al (2014) CT-guided high-dose-rate brachytherapy of liver tumours does not impair hepatic function and shows high overall safety and favourable survival rates. Ann Surg Oncol 21:4284–4292
Sangro B, Gil-Alzugaray B, Rodriguez J et al (2008) Liver disease induced by radioembolization of liver tumors: description and possible risk factors. Cancer 112:1538–1546
Seidensticker M, Seidensticker R, Damm R et al (2014) Prospective randomized trial of enoxaparin, pentoxifylline and ursodeoxycholic Acid for prevention of radiation-induced liver toxicity. PLoS One 9:e112731
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K. Mohnike, S. Wolf, R. Damm, M. Seidensticker, R. Seidensticker, F. Fischbach, N. Peters, P. Hass, G. Gademann, M. Pech, and J. Ricke state that there are no conflicts of interest.
The study was conducted in accordance with the protocol, the ethical principles that have their origin in the Declaration of Helsinki and ICH-GCP. The study protocol and all study-related documentation were approved by all relevant authorities.
Rights and permissions
About this article
Cite this article
Mohnike, K., Wolf, S., Damm, R. et al. Radioablation of liver malignancies with interstitial high-dose-rate brachytherapy. Strahlenther Onkol 192, 288–296 (2016). https://doi.org/10.1007/s00066-016-0957-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-016-0957-0