Abstract
Purpose
Mild traumatic brain injuries (mTBI) sustained during contact sports like amateur boxing are found to have long-term sequelae, being linked to an increased risk of developing neurological conditions like Parkinson’s disease. The aim of this study was to assess differences in volume of anatomical brain structures between amateur boxers and control subjects with a special interest in the affection of deep grey matter structures.
Methods
A total of 19 amateur boxers and 19 healthy controls (HC), matched for age and intelligence quotient (IQ), underwent 3T magnetic resonance imaging (MRI) as well as neuropsychological testing. Body mass index (BMI) was evaluated for every subject and data about years of boxing training and number of fights were collected for each boxer. The acquired 3D high resolution T1 weighted MR images were analyzed to measure the volumes of cortical grey matter (GM), white matter (WM), cerebrospinal fluid (CSF) and deep grey matter structures. Multivariate analysis was applied to reveal differences between groups referencing deep grey matter structures to normalized brain volume (NBV) to adjust for differences in head size and brain volume as well as adding BMI as cofactor.
Results
Total intracranial volume (TIV), comprising GM, WM and CSF, was lower in boxers compared to controls (by 7.1%, P = 0.009). Accordingly, GM (by 5.5%, P = 0.038) and WM (by 8.4%, P = 0.009) were reduced in boxers. Deep grey matter showed statistically lower volumes of the thalamus (by 8.1%, P = 0.006), caudate nucleus (by 11.1%, P = 0.004), putamen (by 8.1%, P = 0.011), globus pallidus (by 9.6%, P = 0.017) and nucleus accumbens (by 13.9%, P = 0.007) but not the amygdala (by 5.5%, P = 0.221), in boxers compared to HC.
Conclusion
Several deep grey matter structures were reduced in volume in the amateur boxer group. Furthermore, longitudinal studies are needed to determine the damage pattern affecting deep grey matter structures and its neuropsychological relevance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mild traumatic brain injury (mTBI) is very common among athletes performing contact sports, like amateur boxing, but also military personnel and older people can be affected, with an estimated number of 42 million cases worldwide each year [1]. The evidence concerning supposed mTBI in amateur boxers has been inconsistent and previous studies have delivered contradictory findings; some reported diminishing of cognitive functions [2, 3], some proved through the analysis of biomarkers in cerebrospinal fluid (CSF) strong evidence of traumatic axonal injury even without measurable cognitive impairment [4], whereas others were skeptical about the presence of credible evidence connecting amateur boxers to chronic brain injury [5,6,7].
During the acute phase after mTBI, following the definition of Orman et al. [8], loss of consciousness should not be longer than 30 min, post-traumatic amnesia should not last longer than 1 day, and the Glasgow Coma Scale (GCS) cannot be below 13. In terms of imaging criteria, it is commonly acknowledged that to fulfill the definition of mTBI only minor or no structural changes, like contusions or microhemorrhages, should be detectable on conventional CT or MRI (magnetic resonance imaging) after the traumatic incident [9]. Instead of obvious structural changes, more subtle changes occur in mTBI, such as diffuse axonal injury, which can be detected by diffusion tensor imaging (DTI) after mTBI [10, 11] also in amateur boxers [12], and cortical thinning, assessed by high-resolution (HR) structural MRI [13, 14]. Also, deep grey matter structures were shown to be affected by volume loss after repeated head trauma in professional fighters. Lower brain volumes in the thalamus and caudate nucleus and less pronounced in the putamen were associated with years of fighting and fight exposure [15]. There is only a limited number of studies exploring the affection of deep grey matter after traumatic brain injuries let alone mTBI. Nevertheless, in recent years mTBI has gained the spotlight for its role in initiating long-term neurodegeneration cascades which result in neurodegenerative diseases also affecting the basal ganglia like Parkinson’s disease [16].
The main objective of this study is to evaluate the effect of amateur boxing on deep grey matter volumes compared to age-matched healthy controls.
Subjects and Methods
Study Design and Subjects
This prospective study was approved by the institutional ethics board and written informed consent was obtained from all participants prior to the examinations.
Included in this study were 19 male amateur boxers recruited from the local Olympic base as well as 19 male healthy control subjects (HC) with no history of any sort of contact sport or boxing. Boxers and HC were chosen from a previously published cohort [17] and matched for age and intelligence quotient (IQ). Participant recruitment, imaging and neuropsychological data collection took place in 2005 [17]. Amateur boxers have full contact in training whilst wearing protective headgear. Exclusion criteria for boxers and HC were anamnestic or imaging evidence for previous moderate or severe traumatic brain injury as defined by Orman et al. [8], participation in any other forms of contact sports (e.g., American football, soccer), any neurological or psychiatric diseases, metabolic diseases, arterial hypertension, substance abuse or any accidental findings which may have interfered with or influenced brain volumetry (e.g., arachnoid cyst and intercranial masses). Subjects with MRI contraindications (e.g., body implants not considered to be 3T MRI-safe) were also excluded.
The revised Hamburg Wechsler Intelligence Examination (HAWIE-R) [18] was performed and referred to as the intelligence quotient (IQ). In addition, planning, alertness and memory performances were assessed using the subtest “alertness” from the “test of attentional performance” (TAPAL) [19, 20], parts A and B of the trail making test (TMT‑A and TMT‑B, respectively) and the verbal learning and memory test (VLMT) [21].
Weight and BMI (body mass index) were assessed for all study subjects. Total number of fights as well as time extent of boxing (since beginning of training) were assessed for boxers.
MR Data Acquisition
All subjects underwent the same MRI protocol on a 3T MR scanner (TRIO; Siemens, Erlangen, Germany) with an 8‑channel head coil. The MRI protocol consisted of transverse dual spin-echo MR imaging sequence (TR/TE, 5850/10.90 ms; section thickness, 6 mm; flip angle, 149°; acquisition matrix, 256 × 256; FOV, 200 mm), a 3D sagittal magnetization-prepared rapid acquisition of gradient echo (MPRAGE) sequence (TR/TE, 2250/3 ms; section thickness, 1 mm; flip angle, 9°; acquisition matrix, 256 × 256; FOV, 245 mm), a coronal T2*-weighted sequence (TR/TE, 599/20 ms; section thickness, 6 mm; flip angle, 20°; acquisition matrix, 256 × 256; FOV, 200 mm), and an axial time-of-flight (TOF) MR angiography sequence (TR/TE, 42/4.67 ms; section thickness, 0.8 mm; flip angle, 25°; acquisition matrix, 512 × 512; FOV, 200 mm).
MR Image Volumetry
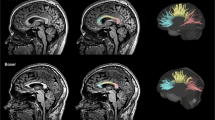
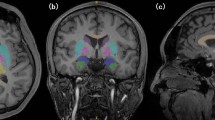
Each set of 3D MPRAGE images was converted from digital imaging and communication in medicine (DICOM) into Neuroimaging Informatics Technology Institute (NIFTI) format and uploaded onto the pipeline volBrain (https://volbrain.upv.es) [22]. It is based on the following preprocessing steps: denoising using the spatially adaptive non-local-means (SANLM) filter [23], coarse inhomogeneity correction [24], registration to Montreal Neurological Institute (MNI) space [25], fine inhomogeneity correction using statistical parametric mapping (SPM) [26], intensity normalization [27]. After that, further steps follow to aid the estimation of brain volumes at different scales: non-local intracranial cavity extraction (NICE) [28], tissue classification [29], non-local hemisphere segmentation (NABS) [30] and non-local subcortical structure segmentation [31].
For this investigation we measured total intracranial volume (TIV), defined as the sum of intracranial grey matter (GM), white matter (WM) and cerebrospinal fluid (CSF), normalized brain volume (NBV), defined as the sum of GM and WM divided by TIV, as well as deep grey matter volumes of the thalamus, globus pallidus, putamen, caudate nucleus, nucleus accumbens and amygdala, respectively. Volume values for both sides were added.
Statistical Analysis
All statistical analyses were performed using SPSS (Version 24; SPSS Inc, Chicago, IL, USA).
Subject characteristics were summarized using descriptive statistics and are presented as mean standard deviation (STD). P values ≤ 0.05 were regarded as statistically significant.
Student’s t‑tests were used to assess differences between the boxer and HC group for TIV, GM, WM and NBV. Correlation analyses between BMI and TIV, GM and WM were conducted to assess interactions between those variables.
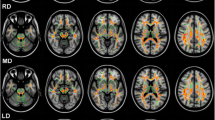
For statistical analysis of the deep grey matter, these structures were set into reference to head size by dividing the volume of the structure by NBV, analogous to the methods used in Ward et al. [32] as presented in Fig. 1. Deep grey matter structures were compared between the boxer and HC groups by applying a multivariate analysis of variance with BMI. Our results were also corrected for effects of age in an analysis of covariance. Linear regression analysis examined the association between number of fights and duration of boxing in years on regional brain volumes of boxers.
Results
Boxer and Healthy Control Subject Characteristics
In the boxer group mean age was 29.1 ± 14.3 years (STD in years; median, 22 years; range, 17–65 years), mean BMI was 23.3 ± 3.4 (STD; median, 22.6; range, 18.8–31.3). For HC mean age was 29.4 ± 12.6 years (STD in years; median, 24 years; range, 16–26 years), mean BMI was 23.5 ± 2.9 (STD; median, 23.0; range, 18.8–29.6).
The mean number of fights in the boxer group was 89.2 ± 62.1 (STD; median, 76; range, 0–216). The mean time extent of boxing was 8.9 ± 4.8 years (STD in years; median, 10 years; range, 3–22 years).
Results of the neuropsychological testing are presented in Table 1. There were no significant differences in testing results between the boxer and HC group.
Structural MRI and MR-Volumetry Results
In our amateur boxer group, no subject showed signs of intracranial traumatic brain injuries, like microhemorrhages or parenchymal lesions. One boxer subject had a small (2 mm) aneurysm located at the anterior communicating artery.
Kolmogorov-Smirnov and Shapiro Wilk tests confirmed the normal distribution of our volumetric measurements.
The TIV, GM and WM volumes were significantly lower in the boxer group than in the HC group. Means and standard deviations as well as the mean difference in percent and the results of the statistical comparison by Student’s t‑test can be found in Table 2.
The BMI significantly correlated with TIV (Pearson’s r = 0.42, P = 0.009), with NBV (r = 0.46, P = 0.003) as well as with total WM volume (r = 0.38, P = 0.019), but not with total GM volume (r = 0.06; P = 0.721).
A multivariate analysis of deep grey matter structure volumes with BMI as a covariate and post hoc testing revealed significantly lower volumes in the boxer group for the caudate nucleus, the putamen, the globus pallidus and the nucleus accumbens but not for the amygdala. In absolute values the difference in volume was most pronounced for the nucleus accumbens with 13.9% less volume in the boxer group compared to the HC group. Results of the analysis are summarized in Table 3. In addition, our results retained significance when corrected for the effect of age.
Linear regression analysis indicated significant associations of duration of boxing in years and right thalamus volume (β = −0.811, P = 0.049). Effects regarding right globus pallidus almost achieved significance with (β = −0.765, P = 0.066). The predictor variables exhibited no significant effects on the remaining volumetric measurements in boxers, see Table 4. Also, there were no significant associations between number of fights and volumetric measurements.
Discussion
We investigated differences in deep grey matter structures between amateur boxers and healthy control subjects. A significantly lower volume for amateur boxers was found in the thalamus, the caudate nucleus, the putamen and globus pallidus as well as the nucleus accumbens, but not the amygdala. The largest significant volume difference of 13.9% between amateur boxers and healthy controls in absolute numbers, was detected in the nucleus accumbens, closely followed by the caudate nucleus with a difference of 11.1% and the globus pallidus with a difference of 9.6%. Bendlin et al. showed a decline in volume over the course of a year after the acute mTBI event affecting, among others, the nucleus accumbens, the putamen and the thalamus [33].The volume loss of basal ganglia and the nucleus accumbens was in line with previous studies in moderate to severe TBI [33,34,35,36,37,38] and has been associated with a progression of neurodegenerative diseases [39, 40], also comprising Parkinson’s disease [41, 42]. Thalamic volume reduction was also apparent in our boxer study group, which supplements the finding of previous studies in TBI [34, 35, 43]. It is noteworthy that head collusions were replicated in a biomechanical investigation using finite element modelling and revealed that the thalamus and midbrain experience the highest shearing stress [44]. The thalamus serves as a sensory relay center which transfers information from the limbic system, basal ganglia and cerebellum to the cerebral cortex [45]. We can assume that this atrophy is attributed to the large number of white matter tracts connected to the thalamus. In the present study, we did not find a significant volume difference in the amygdala volume between our study groups, this is opposed to previous investigations in TBI [36, 46]. On the other hand, the lack of significance might be due to a small study sample in our study.
Of note is our finding that TIV was lower in boxers than in healthy controls. Yet, we are hesitant to draw conclusions of the possible causes. Many potentially confounding factors, among them differences in upbringing, nurture and genetic profile between boxers and healthy controls are imaginable and might influence head size and total intracranial volume.
In mTBI, cortical GM atrophy is more likely to be happening secondary to underlying WM damage, possibly due to retrograde cell death after axonal injury rather than to damage acquired from the direct impact on brain parenchyma. This might explain the time delay in the detection of cortical GM loss before the occurrence of microstructural changes in WM. Several publications showed in longitudinal studies that degenerative adaptation of the brain takes place long after the acute injury, resulting in volume loss of WM and then GM, preceded by an increasing derangement of WM microstructural integrity measurements [33, 47, 48]. Markers for disturbances of WM microstructural integrity are decreased fractional anisotropy (FA) and increased mean diffusivity (MD) in WM structures and were found to be associated with traumatic brain injury in mTBI [49, 50]. It should be noted that the amateur boxers in our study would have been excluded if their brain scans revealed any signs of visible cortical or subcortical contusions, so we assume that the differences in deep GM structure volumes reflect chronic brain damage. Also, in a previous publication, examining a cohort from which our boxers and healthy controls were derived, only 3 of 42 boxers included in that study showed microbleeds that might be associated with traumatic brain injury [17]. Therefore, only a small fraction of the boxers in the study showed traumatic brain changes visible in our conventional MRI protocols.
We found that years of boxing had a significant association with the reduction of right-sided thalamic volume in boxers. This is in line with previous prospective studies that reported greater decline in thalamic volume with increased fight exposure [15, 51]; however, unlike in the aforementioned study by Bray et al. we were not able to test the interaction between weight class and fight exposure regarding different brain volumes due to our small study group. We were also not able to reproduce other significant effects on the remaining brain volumetric measurements, such as the right putamen as reported by Bray et al. In our analysis the number of fights did not predict volumetric differences.
In the study cohort of Bendlin et al. patients after traumatic brain injury even improved in their neuropsychological test performance between 2 months and 1 year post-injury [33], suggesting an acute neuropsychological deterioration after the injury, which can be compensated for after some time despite the progression of microstructural and macrostructural changes. This is in line with the lack of significant differences in neuropsychological measures between our amateur boxer and healthy control group. As we did not consider the timing of potential traumatic brain injuries in the scheduling of our MR imaging and neuropsychological testing appointments, we assume that most boxers in our study group were not most recently affected by traumatic brain injury but rather exposed to potential mTBI over the time of boxing years which might be a mostly compensated state. Nevertheless, other longitudinal studies correlated brain atrophy in mTBI [52] to poorer vocational outcome, as well as in moderate to severe TBI to increased disability and worse neuropsychological outcome [46]. It is an intriguing paradox that even though the brains of the amateur boxers showed seemingly disadvantageous differences, namely deep GM volume loss, neuropsychological testing could not distinguish the boxers and controls in our study. This might be due to methodological issues, such as the heterogeneity of neuropsychological tests or there must be some brain mechanisms that compensates, at least in the beginning, the worsening of neuropsychological functioning.
Limitations
While our study provides some important insights into the brain of amateur boxers, exposed to mTBI, there are several limitations. First, as discussed above, time of injury has an impact on volumetric as well as neuropsychological results, but the time of potential injury was not assessed in our amateur boxer group which might add inaccuracies in the data. Instead, we assumed continuous possible injuries acquired over time of boxing years and only excluded the occurrence of moderate and severe traumatic brain injury via the assessment of conventional MRI imaging and questioning the boxers about the occurrence of long-lasting neurological deficits after fights in the past. Another important caveat is the lack of longitudinal imaging and neuropsychological data acquisition, which limits our ability to understand causative association between mTBI and regional brain atrophy as well as the timing of the atrophy progress. Furthermore, the study could have benefitted from a larger sample size, which especially for the regression analysis might have led to higher statistical power and revealed more associations between volumetric changes and behavioral measures.
Conclusion
In this study exploring the brains of amateur boxers, our findings indicate that atrophy is not a uniformly diffuse process that affects WM and GM, but rather has predilection for various subcortical structures which may be more vulnerable than others, such as nucleus accumbens, thalamus, caudate nucleus, putamen and globus pallidus. Further studies will be needed to determine the impact and progression of regional atrophy on particular neuropsychological outcomes, and it would be worthwhile to incorporate the volumetric data with parameters of axonal integrity in order to understand the relationship between acute white matter injury and volume loss in adjacent grey matter.
References
Gardner RC, Yaffe K. Epidemiology of mild traumatic brain injury and neurodegenerative disease. Mol Cell Neurosci. 2015;66(Pt B):75–80. https://doi.org/10.1016/j.mcn.2015.03.001.
Matser EJ, Kessels AG, Lezak MD, Troost J, Jordan BD. Acute traumatic brain injury in amateur boxing. Phys Sportsmed. 2000;28(1):87–92. https://doi.org/10.3810/psm.2000.01.645.
Moriarity JM, Pietrzak RH, Kutcher JS, Clausen MH, McAward K, Darby DG. Unrecognised ringside concussive injury in amateur boxers. Br J Sports Med. 2012;46(14):1011–5. https://doi.org/10.1136/bjsports-2011-090893.
Neselius S, Brisby H, Marcusson J, Zetterberg H, Blennow K, Karlsson T. Neurological assessment and its relationship to CSF biomarkers in amateur boxers. PLoS One. 2014;9(6):e99870. https://doi.org/10.1371/journal.pone.0099870.
Loosemore M, Knowles CH, Whyte GP. Amateur boxing and risk of chronic traumatic brain injury: systematic review of observational studies. BMJ. 2007;335(7624):809. https://doi.org/10.1136/bmj.39342.690220.55.
Ross DE, Seabaugh JD, Seabaugh JM, Alvarez C, Ellis LP, Powell C, Hall C, Reese C, Cooper L, Ochs AL. Patients with chronic mild or moderate traumatic brain injury have abnormal brain enlargement. Brain Inj. 2020;34(1):11–9. https://doi.org/10.1080/02699052.2019.1669074.
Hart MG, Housden CR, Suckling J, Tait R, Young A, Muller U, Newcombe VFJ, Jalloh I, Pearson B, Cross J, Trivedi RA, Pickard JD, Sahakian BJ, Hutchinson PJ. Advanced magnetic resonance imaging and neuropsychological assessment for detecting brain injury in a prospective cohort of university amateur boxers. Neuroimage Clin. 2017;15:194–9. https://doi.org/10.1016/j.nicl.2017.04.026.
Silver JM, McAllister TW, Arciniegas DB. Textbook of traumatic brain injury. American Psychiatric; 2018.
Koerte IK, Hufschmidt J, Muehlmann M, Lin AP, Shenton ME. Advanced Neuroimaging of mild traumatic brain injury. In: Laskowitz D, Grant G, editors. Translational research in traumatic brain injury. Frontiers in neuroscience. 2016.
Shenton ME, Hamoda HM, Schneiderman JS, Bouix S, Pasternak O, Rathi Y, Vu MA, Purohit MP, Helmer K, Koerte I, Lin AP, Westin CF, Kikinis R, Kubicki M, Stern RA, Zafonte R. A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging Behav. 2012;6(2):137–92. https://doi.org/10.1007/s11682-012-9156-5.
Shin W, Mahmoud SY, Sakaie K, Banks SJ, Lowe MJ, Phillips M, Modic MT, Bernick C. Diffusion measures indicate fight exposure-related damage to cerebral white matter in boxers and mixed martial arts fighters. AJNR Am J Neuroradiol. 2014;35(2):285–90. https://doi.org/10.3174/ajnr.A3676.
Herweh C, Hess K, Meyding-Lamade U, Bartsch AJ, Stippich C, Jost J, Friedmann-Bette B, Heiland S, Bendszus M, Hahnel S. Reduced white matter integrity in amateur boxers. Neuroradiology. 2016;58(9):911–20. https://doi.org/10.1007/s00234-016-1705-y.
Tremblay S, De Beaumont L, Henry LC, Boulanger Y, Evans AC, Bourgouin P, Poirier J, Theoret H, Lassonde M. Sports concussions and aging: a neuroimaging investigation. Cereb Cortex. 2013;23(5):1159–66. https://doi.org/10.1093/cercor/bhs102.
Govindarajan KA, Narayana PA, Hasan KM, Wilde EA, Levin HS, Hunter JV, Miller ER, Patel VK, Robertson CS, McCarthy JJ. Cortical thickness in mild traumatic brain injury. J Neurotrauma. 2016;33(20):1809–17. https://doi.org/10.1089/neu.2015.4253.
Bernick C, Banks S. What boxing tells us about repetitive head trauma and the brain. Alzheimers Res Ther. 2013;5:23.
Washington PM, Villapol S, Burns MP. Polypathology and dementia after brain trauma: Does brain injury trigger distinct neurodegenerative diseases, or should they be classified together as traumatic encephalopathy? Exp Neurol. 2016;275(Pt 3):381–8. https://doi.org/10.1016/j.expneurol.2015.06.015.
Hahnel S, Stippich C, Weber I, Darm H, Schill T, Jost J, Friedmann B, Heiland S, Blatow M, Meyding-Lamade U. Prevalence of cerebral microhemorrhages in amateur boxers as detected by 3T MR imaging. AJNR Am J Neuroradiol. 2008;29(2):388–91. https://doi.org/10.3174/ajnr.A0799.
Tewes U. HAWIE-R: Hamburg-Wechsler-Intelligenztest für Erwachsene, Revision 1991; Handbuch und Testanweisung. Bern: Huber; 1994.
Leclercq M, Zimmerman P. Applied neuropsychology of attention. 2002.
Reitan RM. The relation of the trail making test to organic brain damage. J Consult Psychol. 1955;19(5):393–4. https://doi.org/10.1037/h0044509.
Helmstaedter C, Durwen H. VLMT: Verbaler Lern-und Merkfähigkeitstest: Ein praktikables und differenziertes Instrumentarium zur Prüfung der verbalen Gedächtnisleistungen. Schweizer Archiv für Neurologie, Neurochirurgie und Psychiatrie; 1990.
Manjon JV, Coupe P. volBrain: an online MRI brain volumetry system. Front Neuroinform. 2016;10:30. https://doi.org/10.3389/fninf.2016.00030.
Manjon JV, Coupe P, Marti-Bonmati L, Collins DL, Robles M. Adaptive non-local means denoising of MR images with spatially varying noise levels. J Magn Reson Imaging. 2010;31(1):192–203. https://doi.org/10.1002/jmri.22003.
Tustison NJ, Avants BB, Cook PA, Zheng Y, Egan A, Yushkevich PA, Gee JC. N4ITK: improved N3 bias correction. IEEE Trans Med Imaging. 2010;29(6):1310–20. https://doi.org/10.1109/TMI.2010.2046908.
Avants BB, Tustison N, Song G. Advanced normalization tools (ANTS). Insight j. 2009;2(365):1–35.
Ashburner J, Friston KJ. Unified segmentation. Neuroimage. 2005;26(3):839–51. https://doi.org/10.1016/j.neuroimage.2005.02.018.
Lotjonen JM, Wolz R, Koikkalainen JR, Thurfjell L, Waldemar G, Soininen H, Rueckert D. Alzheimer’s disease neuroimaging I. Fast and robust multi-atlas segmentation of brain magnetic resonance images. Neuroimage. 2010;49(3):2352–65. https://doi.org/10.1016/j.neuroimage.2009.10.026.
Manjon JV, Eskildsen SF, Coupe P, Romero JE, Collins DL, Robles M. Nonlocal intracranial cavity extraction. Int J Biomed Imaging. 2014;2014:820205. https://doi.org/10.1155/2014/820205.
Manjon JV, Tohka J, Garcia-Marti G, Carbonell-Caballero J, Lull JJ, Marti-Bonmati L, Robles M. Robust MRI brain tissue parameter estimation by multistage outlier rejection. Magn Reson Med. 2008;59(4):866–73. https://doi.org/10.1002/mrm.21521.
Romero JE, Manjon JV, Tohka J, Coupe P, Robles M. NABS: non-local automatic brain hemisphere segmentation. Magn Reson Imaging. 2015;33(4):474–84. https://doi.org/10.1016/j.mri.2015.02.005.
Coupe P, Manjon JV, Fonov V, Pruessner J, Robles M, Collins DL. Patch-based segmentation using expert priors: application to hippocampus and ventricle segmentation. Neuroimage. 2011;54(2):940–54. https://doi.org/10.1016/j.neuroimage.2010.09.018.
Ward MA, Carlsson CM, Trivedi MA, Sager MA, Johnson SC. The effect of body mass index on global brain volume in middle-aged adults: a cross sectional study. BMC Neurol. 2005;5:23. https://doi.org/10.1186/1471-2377-5-23.
Bendlin BB, Ries ML, Lazar M, Alexander AL, Dempsey RJ, Rowley HA, Sherman JE, Johnson SC. Longitudinal changes in patients with traumatic brain injury assessed with diffusion-tensor and volumetric imaging. Neuroimage. 2008;42(2):503–14. https://doi.org/10.1016/j.neuroimage.2008.04.254.
Leunissen I, Coxon JP, Caeyenberghs K, Michiels K, Sunaert S, Swinnen SP. Subcortical volume analysis in traumatic brain injury: the importance of the fronto-striato-thalamic circuit in task switching. Cortex. 2014;51:67–81. https://doi.org/10.1016/j.cortex.2013.10.009.
Gooijers J, Chalavi S, Beeckmans K, Michiels K, Lafosse C, Sunaert S, Swinnen SP. Subcortical volume loss in the thalamus, putamen, and pallidum, induced by traumatic brain injury, is associated with motor performance deficits. Neurorehabil Neural Repair. 2016;30(7):603–14. https://doi.org/10.1177/1545968315613448.
Wilde EA, Bigler ED, Hunter JV, Fearing MA, Scheibel RS, Newsome MR, Johnson JL, Bachevalier J, Li X, Levin HS. Hippocampus, amygdala, and basal ganglia morphometrics in children after moderate-to-severe traumatic brain injury. Dev Med Child Neurol. 2007;49(4):294–9. https://doi.org/10.1111/j.1469-8749.2007.00294.x.
Kim J, Avants B, Patel S, Whyte J, Coslett BH, Pluta J, Detre JA, Gee JC. Structural consequences of diffuse traumatic brain injury: a large deformation tensor-based morphometry study. Neuroimage. 2008;39(3):1014–26. https://doi.org/10.1016/j.neuroimage.2007.10.005.
Bigler ED. Volumetric MRI findings in mild traumatic brain injury (mTBI) and neuropsychological outcome. Neuropsychol Rev. 2021; https://doi.org/10.1007/s11065-020-09474-0.
Yi HA, Moller C, Dieleman N, Bouwman FH, Barkhof F, Scheltens P, van der Flier WM, Vrenken H. Relation between subcortical grey matter atrophy and conversion from mild cognitive impairment to Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2016;87(4):425–32. https://doi.org/10.1136/jnnp-2014-309105.
van den Bogaard SJ, Dumas EM, Ferrarini L, Milles J, van Buchem MA, van der Grond J, Roos RA. Shape analysis of subcortical nuclei in Huntington’s disease, global versus local atrophy—Results from the TRACK-HD study. J Neurol Sci. 2011;307(1–2):60–8. https://doi.org/10.1016/j.jns.2011.05.015.
Mavridis IN. Is nucleus accumbens atrophy correlated with cognitive symptoms of Parkinson’s disease? Brain. 2015;138(Pt 1):e319. https://doi.org/10.1093/brain/awu197.
Pitcher TL, Melzer TR, Macaskill MR, Graham CF, Livingston L, Keenan RJ, Watts R, Dalrymple-Alford JC, Anderson TJ. Reduced striatal volumes in Parkinson’s disease: a magnetic resonance imaging study. Transl Neurodegener. 2012;1(1):17. https://doi.org/10.1186/2047-9158-1-17.
Anderson CV, Wood DM, Bigler ED, Blatter DD. Lesion volume, injury severity, and thalamic integrity following head injury. J Neurotrauma. 1996;13(2):59–65. https://doi.org/10.1089/neu.1996.13.59.
Zhang L, Yang KH, King AI. A proposed injury threshold for mild traumatic brain injury. J Biomech Eng. 2004;126(2):226–36. https://doi.org/10.1115/1.1691446.
Haber SN, Calzavara R. The cortico-basal ganglia integrative network: the role of the thalamus. Brain Res Bull. 2009;78(2–3):69–74. https://doi.org/10.1016/j.brainresbull.2008.09.013.
Warner MA, Marquez de la Plata C, Spence J, Wang JY, Harper C, Moore C, Devous M, Diaz-Arrastia R. Assessing spatial relationships between axonal integrity, regional brain volumes, and neuropsychological outcomes after traumatic axonal injury. J Neurotrauma. 2010;27(12):2121–30. https://doi.org/10.1089/neu.2010.1429.
Ruet A, Joyeux F, Segobin S, Jokic C, Desgranges B, Eustache F, Pitel AL. Severe traumatic brain injury patients without focal lesion but with behavioral disorders: shrinkage of gray matter nuclei and thalamus revealed in a pilot Voxel-based MRI study. J Neurotrauma. 2018;35(13):1552–6. https://doi.org/10.1089/neu.2017.5242.
Palacios EM, Owen JP, Yuh EL, Wang MB, Vassar MJ, Ferguson AR, Diaz-Arrastia R, Giacino JT, Okonkwo DO, Robertson CS, Stein MB, Temkin N, Jain S, McCrea M, MacDonald CL, Levin HS, Manley GT, Mukherjee P, Investigators T‑T. The evolution of white matter microstructural changes after mild traumatic brain injury: A longitudinal DTI and NODDI study. Sci Adv. 2020;6(32):eaaz6892. https://doi.org/10.1126/sciadv.aaz6892.
Miles L, Grossman RI, Johnson G, Babb JS, Diller L, Inglese M. Short-term DTI predictors of cognitive dysfunction in mild traumatic brain injury. Brain Inj. 2008;22(2):115–22. https://doi.org/10.1080/02699050801888816.
Douglas DB, Iv M, Douglas PK, Anderson A, Vos SB, Bammer R, Zeineh M, Wintermark M. Diffusion tensor imaging of TBI: potentials and challenges. Top Magn Reson Imaging. 2015;24(5):241–51. https://doi.org/10.1097/RMR.0000000000000062.
Bray MJC, Tsai J, Bryant BR, Narapareddy BR, Richey LN, Krieg A, Tobolowsky W, Jahed S, Shan G, Bernick CB, Peters ME. Effect of weight class on regional brain volume, cognition, and other neuropsychiatric outcomes among professional fighters. Neurotrauma Rep. 2021;2(1):169–79. https://doi.org/10.1089/neur.2020.0057.
Ross DE, Ochs AL, Zannoni MD, Seabaugh JM. Back to the future: estimating pre-injury brain volume in patients with traumatic brain injury. Neuroimage. 2014;102(Pt 2):565–78. https://doi.org/10.1016/j.neuroimage.2014.07.043.
Acknowledgements
No acknowledgments.
Funding
No funding.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Mousa Zidan: methodology, data curation, formal analysis, writing-original draft preparation. Jessica Jesser: conceptualization, validation. Christian Herweh, Uta Meyding-Lamadé: investigation, validation. Sabine Heiland, Joachim Jost: supervision, Martin Bendszus: project administration, supervision. Stefan Haehnel: methodology, writing-reviewing and editing.
Corresponding author
Ethics declarations
Conflict of interest
M. Zidan, J. Jesser, C. Herweh, J. Jost, S. Heiland, U. Meyding-Lamadé, M. Bendszus and S. Haehnel declare that they have no competing interests.
Ethical standards
We declare that all human studies have been approved by the ethics committee of the University of Heidelberg and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed, written consent prior to inclusion in this study.
Additional information
The authors Mousa Zidan and Jessica Jesser contributed equally to the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zidan, M., Jesser, J., Herweh, C. et al. Deep Grey Matter Volume is Reduced in Amateur Boxers as Compared to Healthy Age-matched Controls. Clin Neuroradiol 33, 475–482 (2023). https://doi.org/10.1007/s00062-022-01233-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-022-01233-3