Abstract
Purpose
To assess the effects of rapid maxillary expansion (RME) treatment on the zygomatic bone complex (ZBC).
Methods
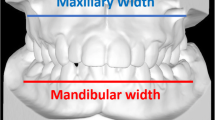
In this single-center retrospective study, pre- and posttreatment cone-beam computed tomography (CBCT) images of 38 patients treated with RME were analyzed to investigate changes in the coordinates of the ZBC landmarks. At the start of treatment (T0), the patients’ mean age was 11.1 ± 3.8 years (range 8.3–14.9 years). Cohen’s d test was used to evaluate statistical differences.
Results
There were statistically significant differences between T0 and T1 (P < 0.01) in the measurement values for the maxillary transverse width (ΔT: 3.18 ± 2.58, d: 1.23), frontozygomatic sutures (ΔT: 1.09 ± 0.56, d: 0.43), lowest point of the zygomaticomaxillary sutures (ΔT: 3.16 ± 1.78, d: 0.78), frontomaxillary angular parameter (right side ΔT: 2.81 ± 1.63, d: 1.73; left side ΔT: 2.52 ± 1.20, d: 2.10), frontozygomatic angular parameter (right side ΔT: 2.81 ± 1.63 d: 1.07; left side ΔT: 2.21 ± 2.79, d: 0.61), anterior intermaxillary distance (ΔT: 2.11 ± 1.42, d: 0.99), interzygomaticotemporal distance (ΔT: 2.00 ± 2.42, d: 0.99), and zygomatic angular parameter (right side ΔT: 2.06 ± 1.29, d: 1.6; left side ΔT: 2.02 ± 1.86, d: 1.09).
Conclusions
After RME in growing patients, the zygomatic bone showed pyramidal expansion in the coronal plane and parallel palatal expansion in the axial plane. In addition, significant lateral relocation of the zygomatic bone occurred. The zygomatic bone tended to rotate outward in conjunction with the maxilla, with a typical center of rotation close to the superior side of the frontozygomatic suture. These results shed light on the patterns of skeletal expansion in the zygomatic bone associated with RME in growing patients.
Zusammenfassung
Zielsetzung
Untersucht werden sollten die Auswirkungen einer RME(„rapid maxillary expansion“)-Behandlung auf den Jochbeinkomplex (ZBC).
Methoden
In dieser retrospektiven Studie wurden die DVT(digitale Volumentomographie)-Aufnahmen von 38 mit RME behandelten Patienten vor und nach der Behandlung ausgewertet, um Veränderungen in den Koordinaten von ZBC-Referenzpunkten zu untersuchen. Zu Behandlungsbeginn (T0) betrug das Durchschnittsalter der Patienten 11,1 ± 3,8 Jahre (Range 8,3–14,9). Zur Auswertung der statistischen Unterschiede wurde der Cohen d-Test verwendet.
Ergebnisse
Es gab statistisch signifikante Unterschiede zwischen T0 und T1 (p < 0,01) bei den Messwerten für die maxilläre Transversalbreite (ΔT: 3,18 ± 2,58, d: 1,23), die frontozygomatischen Nähte (ΔT: 1,09 ± 0,56, d: 0,43), den tiefsten Punkt der zygomaticomaxillären Nähte (ΔT: 3,16 ± 1,78, d: 0,78), die frontomaxillären Winkelparameter (rechts ΔT: 2,81 ± 1,63, d: 1,73, links ΔT: 2,52 ± 1,20, d: 2,10), den frontozygomatischen Winkelparameter (rechts ΔT: 2,81 ± 1,63, d: 1,07, links ΔT: 2,21 ± 2,79, d: 0,61), den anterioren intermaxillären (ΔT: 2,11 ± 1,42, d: 0,99) und den interzygomatotemporalen Abstand (ΔT: 2,00 ± 2,42, d: 0,99), sowie den zygomatischen Winkelparameter (rechts ΔT: 2,06 ± 1,29, d: 1,6, links ΔT: 2,02 ± 1,86, d: 1,09).
Schlussfolgerungen
Nach RME bei wachsenden Patienten zeigte das Jochbein eine pyramidale Expansion in der koronalen Ebene und eine parallele palatinale Expansion in der axialen Ebene. Ferner kam es zu einer signifikanten lateralen Verlagerung des Jochbeins. Tendenziell rotierte das Jochbein in Verbindung mit dem Oberkiefer nach außen, mit einem typischen Rotationszentrum nahe der oberen Seite der frontozygomatischen Naht. Diese Resultate vermitteln einen Eindruck von den Mustern der skelettalen Jochbeinexpansion im Kontext mit einer RME bei wachsenden Patienten.




Similar content being viewed by others
References
Baccetti T, Franchi L, Cameron CG, McNamara JA (2001) Treatment timing for rapid maxillary expansion. Angle Orthod 71:343–350. https://doi.org/10.1043/0003-3219(2001)071〈0343:TTFRME〉2.0.CO;2
Baldawa RS, Bhad WA (2011) Stress distribution analysis during an intermaxillary dysjunction: a 3‑D FEM study of an adult human skull. Ann Maxillofac Sur 1:19. https://doi.org/10.4103/2231-0746.83148
Baldini A, Nota A, Santariello C, Caruso S, Assi V, Ballanti F, Gatto R, Cozza P (2018) Sagittal dentoskeletal modifications associated with different activation protocols of rapid maxillary expansion. Eur J Paediatr Dent 19:151–155. https://doi.org/10.23804/ejpd.2018.19.02.10
Baydas B, Yavuz I, Uslu H, Dagsuyu IM, Ceylan I (2006) Nonsurgical rapid maxillary expansion effects on craniofacial structures in young adult females. A bone scintigraphy study. Angle Orthod 76:759–767. https://doi.org/10.1043/0003-3219(2006)076[0759:NRMEEO]2.0.CO;2
Bazargani F, Feldmann I, Bondemark L (2013) Three-dimensional analysis of effects of rapid maxillary expansion on facial sutures and bones. Angle Orthod 83:1074–1082. https://doi.org/10.2319/020413-103.1
Berger JL, Pangrazio-Kulbersh V, Borgula T, Kaczynski R (1998) Stability of orthopedic and surgically assisted rapid palatal expansion over time. Am J Orthod Dentofacial Orthop 114:638–645. https://doi.org/10.1016/S0889-5406(98)70195-7
Braun S, Bottrel JA, Lee K‑G, Lunazzi JJ, Legan HL (2000) The biomechanics of rapid maxillary sutural expansion. Am J Orthod Dentofacial Orthop 118:257–261. https://doi.org/10.1067/mod.2000.108254
Brunetto DP, Sant’Anna EF, Machado AW, Moon W (2017) Non-surgical treatment of transverse deficiency in adults using microimplant-assisted rapid palatal expansion (MARPE). Dental Press J Orthod 22:110–125. https://doi.org/10.1590/2177-6709.22.1.110-125.sar
Bucci R, D’Antò V, Rongo R, Valletta R, Martina R, Michelotti A (2016) Dental and skeletal effects of palatal expansion techniques: a systematic review of the current evidence from systematic reviews and meta-analyses. J Oral Rehabil 43:543–564. https://doi.org/10.1111/joor.12393
Cantarella D, Dominguez-Mompell R, Mallya SM, Moschik C, Pan HC, Miller J, Moon W (2017) Changes in the midpalatal and pterygopalatine sutures induced by micro-implant-supported skeletal expander, analyzed with a novel 3D method based on CBCT imaging. Prog Orthod 18:34. https://doi.org/10.1186/s40510-017-0188-7
Cantarella D, Dominguez-Mompell R, Moschik C, Mallya SM, Pan HC, Alkahtani MR, Elkenawy I, Moon W (2018) Midfacial changes in the coronal plane induced by microimplant-supported skeletal expander, studied with cone-beam computed tomography images. Am J Orthod Dentofacial Orthop 154:337–345. https://doi.org/10.1016/j.ajodo.2017.11.033
Carlson C, Sung J, McComb RW, Machado AW, Moon W (2016) Microimplant-assisted rapid palatal expansion appliance to orthopedically correct transverse maxillary deficiency in an adult. Am J Orthod Dentofacial Orthop 149:716–728. https://doi.org/10.1016/j.ajodo.2015.04.043
Cevidanes LHC, Heymann G, Cornelis MA, DeClerck HJ, Tulloch JFC (2009) Superimposition of 3‑dimensional cone-beam computed tomography models of growing patients. Am J Orthod Dentofacial Orthop 136:94–99. https://doi.org/10.1016/j.ajodo.2009.01.018
Dejak B, Mlotkowski A, Romanowicz M (2005) Finite element analysis of mechanism of cervical lesion formation in simulated molars during mastication and parafunction. J Prosthet Dent 94:520–529. https://doi.org/10.1016/j.prosdent.2005.10.001
Gardner GE, Kronman JH (1971) Cranioskeletal displacements caused by rapid palatal expansion in the rhesus monkey. Am J Orthod 59:146–155. https://doi.org/10.1016/0002-9416(71)90046-7
Garib DG, Henriques JFC, Janson G, Freitas MR, Coelho RA (2005) Rapid maxillary expansion—tooth tissue-borne versus tooth-borne expanders: a computed tomography evaluation of dentoskeletal effects. Angle Orthod 75:548–557. https://doi.org/10.1043/0003-3219(2005)75[548:RMETVT]2.0.CO;2
Gautam P, Valiathan A, Adhikari R (2007) Stress and displacement patterns in the craniofacial skeleton with rapid maxillary expansion: a finite element method study. Am J Orthod Dentofacial Orthop 132:5.e1–5.e11. https://doi.org/10.1016/j.ajodo.2006.09.044
Ghoneima A, Abdel-Fattah E, Hartsfield J, El-Bedwehi A, Kamel A, Kula K (2011) Effects of rapid maxillary expansion on the cranial and circummaxillary sutures. Am J Orthod Dentofacial Orthop 140:510–519. https://doi.org/10.1016/j.ajodo.2010.10.024
Haas AJ (1965) The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod 35:200–217. https://doi.org/10.1043/0003
Holberg C (2005) Effects of rapid maxillary expansion on the cranial base—an FEM-analysis. J Orofac Orthop 66:54–66. https://doi.org/10.1007/s00056-005-0439-y
Işeri H, Tekkaya AE, Öztan Ö, Bilgiç S (1998) Biomechanical effects of rapid maxillary expansion on the craniofacial skeleton, studied by the finite element method. Eur J Orthod 20:347–356. https://doi.org/10.1093/ejo/20.4.347
Jafari A, Shetty KS, Kumar M (2003) Study of stress distribution and displacement of various craniofacial structures following application of transverse orthopedic forces—a three-dimensional FEM study. Angle Orthod 73:12–20. https://doi.org/10.1043/0003-3219(2003)073〈0012:SOSDAD〉2.0.CO;2
Jain V, Shyagali TR, Kambalyal P, Rajpara Y, Doshi J (2017) Comparison and evaluation of stresses generated by rapid maxillary expansion and the implant-supported rapid maxillary expansion on the craniofacial structures using finite element method of stress analysis. Prog Orthod 18:3. https://doi.org/10.1186/s40510-016-0157-6
Krishnan V, Davidovitch Z (2006) Cellular, molecular, and tissue-level reactions to orthodontic force. Am J Orthod Dentofacial Orthop 129:469.e1–469.e32. https://doi.org/10.1016/j.ajodo.2005.10.007
Lee K‑G, Ryu Y‑K, Park Y‑C, Rudolph DJ (1997) A study of holographic interferometry on the initial reaction of maxillofacial complex during protraction. Am J Orthod Dentofacial Orthop 111:623–632. https://doi.org/10.1016/S0889-5406(97)70314-7
Leonardi R, Muraglie S, Bennici O, Cavallini C, Spampinato C (2019) Three-dimensional analysis of mandibular functional units in adult patients with unilateral posterior crossbite: a cone beam study with the use of mirroring and surface-to-surface matching techniques. Angle Orthod 89:590–596. https://doi.org/10.2319/081718-607.1
Leonardi R, Sicurezza E, Cutrera A, Barbato E (2011) Early post-treatment changes of circumaxillary sutures in young patients treated with rapid maxillary expansion. Angle Orthod 81:36–41. https://doi.org/10.2319/050910-250.1
Lux CJ (2004) Transverse development of the craniofacial skeleton and dentition between 7 and 15 years of age—a longitudinal postero-anterior cephalometric study. Eur J Orthod 26:31–42. https://doi.org/10.1093/ejo/26.1.31
Melsen B, Melsen F (1982) The postnatal development of the palatomaxillary region studied on human autopsy material. Am J Orthod 82:329–342. https://doi.org/10.1016/0002-9416(82)90467-5
Ong SC, Khambay BS, McDonald JP, Cross DL, Brocklebank LM, Ju X (2015) The novel use of three-dimensional surface models to quantify and visualise the immediate changes of the mid-facial skeleton following rapid maxillary expansion. Surgeon 13:132–138. https://doi.org/10.1016/j.surge.2013.10.012
Paredes N, Colak O, Sfogliano L, Elkenawy I, Fijany L, Fraser A, Zhang B, Moon W (2020) Differential assessment of skeletal, alveolar, and dental components induced by microimplant-supported midfacial skeletal expander (MSE), utilizing novel angular measurements from the fulcrum. Prog Orthod 21:18. https://doi.org/10.1186/s40510-020-00320-w
Priyadarshini J, Mahesh CM, Chandrashekar BS, Sundara A, Arun AV, Reddy VP (2017) Stress and displacement patterns in the craniofacial skeleton with rapid maxillary expansion—a finite element method study. Prog Orthod 18:17. https://doi.org/10.1186/s40510-017-0172-2
Proffit WR, Turvey TA, Phillips C (1996) Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg 11:191–204
Resnick CM, Daniels KM, Vlahos M (2018) Does Andrews facial analysis predict esthetic sagittal maxillary position? Oral Surg Oral Med Oral Pathol Oral Radiol 125:376–381. https://doi.org/10.1016/j.oooo.2018.01.012
Seong E‑H, Choi S‑H, Kim H‑J, Yu H‑S, Park Y‑C, Lee K‑J (2018) Evaluation of the effects of miniscrew incorporation in palatal expanders for young adults using finite element analysis. Korean J Orthod 48:81. https://doi.org/10.4041/kjod.2018.48.2.81
Shetty V, Caridad J, Caputo AA, Chaconas SJ (1994) Biomechanical rationale for surgical-orthodontic expansion of the adult maxilla. J Oral Maxillofac Surg 52:742–749. https://doi.org/10.1016/0278-2391(94)90492-8
da Silva Filho OG, do Prado Montes LA, Torelly LF (1995) Rapid maxillary expansion in the deciduous and mixed dentition evaluated through posteroanterior cephalometric analysis. Am J Orthod Dentofacial Orthop 107:268–275. https://doi.org/10.1016/S0889-5406(95)70142-7
Starnbach H, Bayne D, Cleall J, Subtelny JD (1966) Facioskeletal and dental changes resulting from rapid maxillary expansion. Angle Orthod 36:152–164. https://doi.org/10.1043/0003-3219(1966)036〈0152:FADCRF〉2.0.CO;2
Stepanko LS, Lagravère MO (2016) Sphenoid bone changes in rapid maxillary expansion assessed with cone-beam computed tomography. Korean J Orthod 46:269. https://doi.org/10.4041/kjod.2016.46.5.269
Timms DJ (1980) A study of basal movement with rapid maxillary expansion. Am J Orthod 77:500–507. https://doi.org/10.1016/0002-9416(80)90129-3
Wertz R, Dreskin M (1977) Midpalatal suture opening: a normative study. Am J Orthod 71:367–381. https://doi.org/10.1016/0002-9416(77)90241-X
Wikiversity (2021) Cohen’s d. https://en.m.wikiversity.org/wiki/Cohen%27s_d. Accessed 27 July 2021
Woller JL, Kim KB, Behrents RG, Buschang PH (2014) An assessment of the maxilla after rapid maxillary expansion using cone beam computed tomography in growing children. Dental Press J Orthod 19:26–35. https://doi.org/10.1590/2176-9451.19.1.026-035.oar
Funding
Research for this study did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors read and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
U. Ok, E. Kayalar and S. Sadry declare that they have no competing interests.
Ethical standards
Ethical approval for the study was received from the Istanbul Aydin University ethics committee (approval number 2021/356). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from all of the individual participants or their family included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Availability of Data and Materials
The data that support the findings of this study are available from the corresponding author upon reasonable request
Rights and permissions
About this article
Cite this article
Ok, U., Kayalar, E. & Sadry, S. Three-dimensional zygomatic changes after rapid maxillary expansion in growing patients. J Orofac Orthop 84, 147–156 (2023). https://doi.org/10.1007/s00056-021-00348-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-021-00348-5