Abstract
Background
Multiple operations exist to treat haemorrhoids. Although comparisons of conventional excision and other techniques have been performed, there are less comparative outcome data available for stapled haemorrhoidopexy (SH) and radiofrequency haemorrhoidectomy (RFH). Use of a radiofrequency energy device for haemorrhoidectomy is an alternative to standard diathermy, scissors or scalpel. It provides vessel sealing between the jaws of the instrument and aims to minimise wider tissue damage.
Objective
To systematically review the literature comparing SH and RFH, assessing complications, outcomes, patient experience and costs.
Methods
A tailored search of medical databases identified literature containing relevant primary and secondary data comparing SH and RFH. Papers were screened for relevance and completeness of published data. Those missing methodological information, outcome data or statistical analysis were subsequently excluded. A narrative review was then performed.
Results
The primary data in this review originate from six randomised control trials (RCTs) and five meta-analyses. Evidence was conflicting, with a trend towards more early postoperative pain in the RFH vs. the SH group (three RCTs reported increased early pain scores in the RFH group). Significantly higher rates of residual and recurrent haemorrhoids and prolapse in the SH group were observed in two RCTs and four meta-analyses. Bleeding, urinary retention, incontinence and anal stenosis did not significantly differ. No detailed contemporary cost analysis was found.
Conclusion
The trials are small, with significant heterogeneity in the techniques used and outcome data recorded. However, despite the limited available evidence, RFH appears superior to SH due to significantly lower rates of residual and recurrent haemorrhoids and prolapse.
Zusammenfassung
Hintergrund
Es gibt mehrere Operationsverfahren zur Behandlung von Hämorrhoiden. Vergleiche zwischen konventioneller Exzision und anderen Techniken wurden zwar durchgeführt, aber für die Stapler-Hämorrhoidopexie und die Hochfrequenzhämorrhoidektomie (RFH) sind wenig vergleichbare Ergebnisdaten verfügbar. Der Einsatz eines Hochfrequenzenergiegeräts für die Hämorrhoidektomie stellt eine Alternative zu Standarddiathermie, Schere oder Skalpell dar. Es ermöglicht den Gefäßverschluss zwischen den Backen des Instruments und zielt darauf ab, größere Gewebeschädigungen zu minimieren.
Ziel
Ziel war es, einen systematischen Überblick über die Literatur zum Vergleich von SH und RFH zu geben und dabei Komplikationen, Ergebnisse, Erfahrungen der Patienten und Kosten zu beurteilen.
Methoden
Durch eine passgenaue Suche in medizinischen Datenbanken wurden Publikationen mit relevanten Primär- und Sekundärdaten zum Vergleich von SH und RFH ermittelt. Die Arbeiten wurden in Bezug auf Relevanz und Vollständigkeit der veröffentlichten Daten überprüft. Arbeiten, in denen methodologische Informationen, Ergebnisdaten oder statistische Analysen fehlten, wurden anschließend aussortiert. Dann wurde eine narrative Übersicht erstellt.
Ergebnisse
Die primären Daten in der vorliegenden Übersichtsarbeit stammen aus 6 randomisierten kontrollierten Studien (RCT) und Auswertungen. Die Evidenzlage war widersprüchlich, mit einer Tendenz in Richtung größerer früh postoperativer Schmerzen in der RFH- vs. SH-Gruppe (in 3 RCT wurde über steigende früh postoperative Schmerzscores in der RFH-Gruppe berichtet). Signifikant höhere Raten an Residual- und Rezidivhämorrhoiden und -prolapsen in der SH-Gruppe wurden in den beiden RCT und den 4 Metaanalysen festgestellt. Die Daten zu Blutung, Harnretention, Inkontinenz und Analstenose unterschieden sich nicht signifikant. Es fand sich keine detaillierte aktuelle Kostenanalyse.
Schlussfolgerung
Die Studien sind von geringem Umfang, mit signifikanter Heterogenität in den verwendeten Techniken und aufgezeichneten Ergebnisdaten. Jedoch scheint die RFH trotz der begrenzten verfügbaren Evidenz der SH aufgrund signifikant niedrigerer Raten an Residual- und Rezidivhämorrhoiden und -prolapsen überlegen zu sein.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Conventional haemorrhoidectomies are often associated with postoperative pain and bleeding. More recent techniques such as stapled haemorrhoidopexy and radiofrequency haemorrhoidectomy aim to reduce these complications. We systematically compared the evidence on complications, outcomes, patient experiences and costs of these modern methods.
Haemorrhoidectomy is effective and widely used for symptomatic grade 3 and 4 haemorrhoidal disease [16]. Conventional excisional techniques include the Milligan–Morgan [10], Ferguson [6], and Parks procedures [12] performed with diathermy, scissors or scalpels. The most common problems are postoperative pain and bleeding. More recent techniques such as stapled haemorrhoidopexy (SH) and haemorrhoidectomy using a radiofrequency device (RFH) were developed to reduce these complications.
Herein, we aim to look at the evidence comparing SH to RFH with respect to complications, outcomes, patient experiences and costs.
Materials and methods
A literature review was performed using multiple databases: Ovid MEDLINE, CINAHL, SCOPUS, PROSPERO, Cochrane library, EMBASE, World of Knowledge and PubMed. The search strategy was tailored for each database and, where feasible, combined both MeSH terms and keywords. The three components of each search were haemorrhoids, radiofrequency (RF) or named devices and stapled, procedure for prolapse and haemorrhoids (PPH) or Longo procedure.
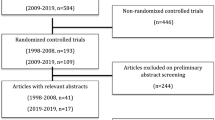
Following the initial searches, references were examined via the abstract. Studies containing primary outcome data or secondary analyses comparing SH with RFH were included and full texts retrieved. The relevance and completeness of the published data were reviewed. Studies with significant missing methodological information, outcome data or statistical analyses were subsequently excluded. The citations and references of included papers were searched for further relevant studies. Fig. 1 shows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) chart for this work.
Results
There were 11 relevant papers in this review, including six randomised controlled trials (RCTs) published between 2005 and 2018 with a total of 457 patients. In addition, there were five systematic reviews and meta-analysis on the subject, one of which is a network meta-analysis included in the discussion.
Primary data
There were six RCTs identified with primary data included in the review, as summarised in Table 1.
Secondary analysis
A total of five systematic reviews and meta-analysis were found to compare SH with RFH, as summarised in Table 2. These all included the relevant studies at the time of their publication; however, none included all six papers.
Intraoperative experience
Two of the studies reported on intraoperative outcomes. Basdanis et al. [2] recorded episodes of intraoperative bleeding, occurring in 36% of stapled procedures compared to 8.8% in the LigaSure (Medtronic, Minneapolis, MN, USA) group, P < 0.05. Kraemer et al. [8] also evaluated the ease of handling and immediate operative result as rated by the operating surgeon. There was no significant difference between the groups (P = 0.5535 for ease of use or P = 0.4384 for immediate results).
Five studies referred to operating times [2, 4, 7, 8, 14]; the findings were conflicting, with studies favouring different groups. The difference between approaches ranged from 2 to 7 min, and is therefore not clinically relevant.
Postoperative complications
Pain
Postoperative pain is a major problem associated with haemorrhoidectomy. Both SH and RFH have demonstrated lower pain scores compared to the conventional approach [15]. The RCTs mainly recorded analgesia use and pain scores on a visual analogue scale (VAS) at selected timepoints. The results are shown in Table 3.
There are three studies that found increased early postoperative pain in the RFH group [2, 4, 7] during the first week after surgery, although no significant difference was identified in the other three trials [1, 8, 14].
The data collected are heterogenous, with variations in technique and endpoints.
In contrast to the other studies, during SH, Kraemer et al. [8] excised the external haemorrhoids with scissors. During haemorrhoidectomy with the radiofrequency device, Sakr et al. [14] used the conventional Milligan and Morgan technique with scissors below the dentate line and only applied the LigaSure device above the dentate line. However, three meta-analyses attempted to pool the data [3, 9, 18], and all found no significant difference in postoperative pain between the two procedures.
The network meta-analysis by Simillis et al. [15] found significantly more postoperative pain following LigaSure haemorrhoidectomy compared to SH at day 14.
Bleeding, urinary retention and incontinence
Common early postoperative complications include bleeding, urinary retention and incontinence in particular; these are summarised in Table 4.
There were no consistent differences between the approaches identified across the studies. The only significant finding was an increase in bleeding in the SH group by Chen et al. [4]. The meta-analyses pooled data across studies and did not identify any significant differences.
Basdanis et al. [2] also looked at anal manometry in postoperative patients, with no significant difference found between groups upon comparing mean resting anal pressures, maximum anal squeeze pressure and rectal compliance immediately postoperatively and after 1 month.
Two studies [4, 14] recorded constipation, wound infection and anal fissures, demonstrating no significant differences between the groups. However, Basdanis et al. [2] reported significantly increased itching and anorectal discharge immediately postoperatively in the radiofrequency device group. These differences were not present 1 month after surgery.
Anal stenosis and recurrence
Longer-term complications include anal stenosis and recurrence of both haemorrhoids and prolapse; these findings are summarised in Table 5.
In two studies [2, 7] there were significantly higher rates of haemorrhoid recurrence and prolapse in the SH group. The meta-analyses by Chen [3] (odds ratio, OR, 0.18 for recurrence in RFH, P = 0.01), Lee [9] (OR 5.53 for recurrence in SH, P = 0.016) and Yang et al. [18] (OR 0.21 for recurrence in RFH, P = 0.003), and the network analysis by Simillis et al. [15] also found significantly higher recurrence rates in the SH compared to the RFH group. Residual prolapse and skin tags were recorded by two studies [1, 14], both of which found a significantly higher incidence in the SH group (P = 0.04 and P = 0.024, respectively).
Life-threatening complications are rare after haemorrhoid surgery. Most case reports are associated with SH [13]. Rectal perforation, rectovaginal fistulae and sepsis have been reported, and there is an estimated 10% risk of mortality if the sepsis is secondary to SH [5]. None of these complications were identified in the presented studies.
Patient experience
Three studies referred to length of hospital stay [2, 7, 14]. There was no significant difference between the two groups, with results ranging from 20 h to 2.44 days. Four studies [1, 2, 7, 14] provided time to return to work or normal activities. The range of values lay between 6 days and 3 weeks, but none of these studies demonstrated a significant difference between the techniques.
Kraemer [8] and Chen et al. [4] both refer to patient satisfaction, with seemingly high self-reported scores and no significant differences between groups.
Costs
In 2004, Basdanis et al. [2] reports a surgical cost of 1175 Euros for SH and 780 Euros for RFH using the LigaSure device. With the addition of length of stay and medications, the costs were 1504 and 1268 Euros, respectively. Chen et al. [4] estimated the average costs for SH to be 748 Euros and for LigaSure to be 464 Euros (P < 0.05) in 2007 (converted from Yuan based on 1 Yuan to 0.096 Euros). These are not contemporary prices; the range of products available has expanded and although the evidence presented is limited to the LigaSure device, cheaper devices and staplers are available. In view of this, without an up-to-date cost analysis, it is difficult to draw any conclusions.
Discussion
In this review, SH was associated with significantly higher rates of residual and recurrent haemorrhoids during follow-up compared to RFH, although RFH appeared to show higher early pain scores compared to the stapled group. The eTHoS trial [17] established the superiority of conventional haemorrhoidectomy over SH, illustrating a similar picture of lower recurrence rates for the conventional technique, albeit with higher pain scores.
There were no significant differences in terms of hospital stay, return to work or normal activities and patient satisfaction, although no detailed quality of life data were recorded by any of the studies. Two studies compared costs; however, both are over 10 years old, and it is therefore unclear which procedure would be considered most cost-effective nowadays.
There are a number of limitations of the six RTCs included, particularly the small size, significant variation in techniques and heterogeneity of the outcomes measured. The only radiofrequency device used was the LigaSure.
Conclusion
Despite the limited evidence currently available, radiofrequency haemorrhoidectomy appears to be superior to stapled haemorrhoidopexy.
References
Arslani N, Patrlj L, Rajkovi ÄZ, Pape ÅD, Altarac S (2012) A randomized clinical trial comparing ligasure versus stapled hemorrhoidectomy. Surg Laparosc Endosc Percutan Tech 22(1):58–61
Basdanis G, Papadopoulos VN, Michalopoulos A, Apostolidis S, Harlaftis N (2005) Randomized clinical trial of stapled hemorrhoidectomy vs open with Ligasure for prolapsed piles. Surg Endosc Interv Tech 19(2):235–239
Chen HL, Woo XB, Cui J, Chen CQ, Peng JS (2014) Ligasure versus stapled hemorrhoidectomy in the treatment of hemorrhoids: a meta-analysis of randomized control trials. Surg Laparosc Endosc Percutan Tech 24(4):285–289
Chen S, Lai D, Yang B, Zhang L, Zhou T, Chen G (2007) Therapeutic comparison between procedure for prolapse and hemorrhoids and Ligasure technique for hemorrhoids. Chin J Gastrointest Surg 10(4):342–345
Faucheron JL, Voirin D, Abba J (2012) Rectal perforation with life-threatening peritonitis following stapled haemorrhoidopexy. Br J Surg 99(6):746–753
Ferguson JA, Heaton JR (1959) Closed hemorrhoidectomy. Dis Colon Rectum 2(176):179
Ibrahim I, Metwalli A, Goda A (2018) LigaSure hemorrhoidectomy compared with stapled hemorrhoidopexy for management of grade III and IV hemorrhoids: A prospective randomized study. Life Sci J 15(4):92–99
Kraemer M, Parulava T, Roblick M, Duschka L, Muller-Lobeck H (2005) Prospective, randomized study: proximate PPH stapler vs. LigaSure for hemorrhoidal surgery. Dis Colon Rectum 48(8):1517–1522
Lee KC, Chen HH, Chung KC, Hu WH, Chang CL, Lin SE, Tsai KL, Lu CC (2013) Meta-analysis of randomized controlled trials comparing outcomes for stapled hemorrhoidopexy versus LigaSure hemorrhoidectomy for symptomatic hemorrhoids in adults. Int J Surg 11(9):914–918
Milligan ETC, Morgan CN, Jones LE, Officer R (1937) Surgical anatomy of the anal canal and the operative treatment of hemorrhoids. Lancet 2:1119–1124
Milito G, Cadeddu F, Muzi MG, Nigro C, Farinon AM (2010) Haemorrhoidectomy with LigasureTM vs conventional excisional techniques: meta-analysis of randomized controlled trials. Colorectal Dis 12(2):85–93
Parks AG (1956) The surgical treatment of haemorrhoids. Br J Surg 43:337–351
Porrett LJ, Porrett JK, Ho YH (2015) Documented complications of staple hemorrhoidopexy: a systematic review. Int Surg 100(1):44–57
Sakr MF, Moussa MM (2010) LigaSure hemorrhoidectomy versus stapled hemorrhoidopexy: a prospective, randomized clinical trial. Dis Colon Rectum 53(8):1161–1167
Simillis C, Thoukididou SN, Slesser AAP, Rasheed S, Tan E, Tekkis PP (2015) Systematic review and network meta-analysis comparing clinical outcomes and effectiveness of surgical treatments for haemorrhoids. Br J Surg 102(13):1603–1618
van Tol RR, Bruijnen MPA, Melenhorst J, van Kuijk SMJ, Stassen LPS, Breukink SO (2018) A national evaluation of the management practices of hemorrhoidal disease in the Netherlands. Int J Colorectal Dis 33(5):577–588
Watson AJ, Hudson J, Wood J, Kilonzo M, Brown SR, McDonald A, Norrie J, Bruhn H, Cook JA, eTHoS study group (2016) Comparison of stapled haemorrhoidopexy with traditional excisional surgery for haemorrhoidal disease (eTHoS): a pragmatic, multicentre, randomised controlled trial. Lancet 388(10058):2375–2385
Yang J, Cui PJ, Han HZ, Tong DN (2013) Meta-analysis of stapled hemorrhoidopexy vs LigaSure hemorrhoidectomy. World J Gastroenterol 19(29):4799–4807
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Sunny, H. Sellars, G. Ramsay, R. Polson and A.J.M. Watson declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sunny, A., Sellars, H., Ramsay, G. et al. Who needs a stapling device for haemorrhoidectomy, if one has the radiofrequency device?. coloproctology 42, 24–29 (2020). https://doi.org/10.1007/s00053-019-00420-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00053-019-00420-0