Abstract
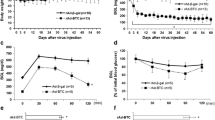
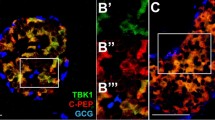
Insulin deficiency may be due to the reduced proliferation capacity of islet β-cell, contributing to the onset of diabetes. It is therefore imperative to investigate the mechanism of the β-cell regeneration in the islets. NKX6.1, one of the critical β-cell transcription factors, is a pivotal element in β-cell proliferation. The ubiquitin-binding enzyme 2C (UBE2C) was previously reported as one of the downstream molecules of NKX6.1 though the exact function and mechanism of UBE2C in β-cell remain to be elucidated. Here, we determined a subpopulation of islet β-cells highly expressing UBE2C, which proliferate actively. We also discovered that β-cell compensatory proliferation was induced by UBE2C via the cell cycle renewal pathway in weaning and high-fat diet (HFD)-fed mice. Moreover, the reduction of β-cell proliferation led to insulin deficiency in βUbe2cKO mice and, therefore, developed type 2 diabetes. UBE2C was found to regulate PER1 degradation through the ubiquitin–proteasome pathway via its association with a ubiquitin ligase, CUL1. PER1 inhibition rescues UBE2C knockout-induced β-cell growth inhibition both in vivo and in vitro. Notably, overexpression of UBE2C via lentiviral transduction in pancreatic islets was able to relaunch β-cell proliferation in STZ-induced diabetic mice and therefore partially alleviated hyperglycaemia and glucose intolerance. This study indicates that UBE2C positively regulates β-cell proliferation by promoting ubiquitination and degradation of the biological clock suppressor PER1. The beneficial effect of UBE2C on islet β-cell regeneration suggests a promising application in treating diabetic patients with β-cell deficiency.
Graphical abstract









Similar content being viewed by others
Data availability
The scRNA-seq analysis datasets during the current study are available in the Gene Expression Omnibus (GEO) repository under the accession number GSE203376 (mouse) and GSE148073 (human). Other datasets are available from the corresponding author upon reasonable request.
References
Sims EK, Carr ALJ, Oram RA, DiMeglio LA, Evans-Molina C (2021) 100 years of insulin: celebrating the past, present and future of diabetes therapy. Nat Med 27(7):1154–1164. https://doi.org/10.1038/s41591-021-01418-2
Mathieu C, Martens PJ, Vangoitsenhoven R (2021) One hundred years of insulin therapy. Nat Rev Endocrinol 17(12):715–725. https://doi.org/10.1038/s41574-021-00542-w
Eizirik DL, Pasquali L, Cnop M (2020) Pancreatic Î2-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat Rev Endocrinol 16(7):349–362. https://doi.org/10.1038/s41574-020-0355-7
Hudish LI, Reusch JE, Sussel L (2019) Î2 Cell dysfunction during progression of metabolic syndrome to type 2 diabetes. J Clin Investig 129(10):4001–4008. https://doi.org/10.1172/jci129188
Halban PA, Polonsky KS, Bowden DW et al (2014) Î2-cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment. Diabetes Care 37(6):1751–1758. https://doi.org/10.2337/dc14-0396
Samnegård B, Jacobson SH, Jaremko G, Johansson BL, Sjöquist M (2001) Effects of C-peptide on glomerular and renal size and renal function in diabetic rats. Kidney Int 60(4):1258–1265. https://doi.org/10.1046/j.1523-1755.2001.00964.x
Al-Rasheed NM, Willars GB, Brunskill NJ (2006) C-peptide signals via Galpha i to protect against TNF-α-mediated apoptosis of opossum kidney proximal tubular cells. J Am Soc Nephrol 17(4):986–995. https://doi.org/10.1681/asn.2005080797
Li J, Zhang Y, Ye Y et al (2021) Pancreatic Î2 cells control glucose homeostasis via the secretion of exosomal miR-29 family. J Extracell Vesicles 10(3):e12055. https://doi.org/10.1002/jev2.12055
Poy MN, Hausser J, Trajkovski M et al (2009) miR-375 maintains normal pancreatic alpha- and beta-cell mass. Proc Natl Acad Sci USA 106(14):5813–5818. https://doi.org/10.1073/pnas.0810550106
Dor Y, Brown J, Martinez OI, Melton DA (2004) Adult pancreatic β-cells are formed by self-duplication rather than stem-cell differentiation. Nature 429(6987):41–46
Parsons JA, Brelje TC, Sorenson RL (1992) Adaptation of islets of Langerhans to pregnancy: increased islet cell proliferation and insulin secretion correlates with the onset of placental lactogen secretion. Endocrinology 130(3):1459–1466
Klöppel G, Löhr M, Habich K, Oberholzer M, Heitz PU (1985) Islet pathology and the pathogenesis of type 1 and type 2 diabetes mellitus revisited. Surv Synth Pathol Res 4(2):110–125
Sorenson RL, Brelje TC (1997) Adaptation of islets of Langerhans to pregnancy: beta-cell growth, enhanced insulin secretion and the role of lactogenic hormones. Horm Metab Res 29(6):301–307. https://doi.org/10.1055/s-2007-979040
Hu FB, Manson JE, Stampfer MJ et al (2001) Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 345(11):790–797. https://doi.org/10.1056/NEJMoa010492
Stott NL, Marino JS (2020) High fat rodent models of type 2 diabetes: from rodent to human. Nutrients. https://doi.org/10.3390/nu12123650
Hudish LI, Reusch J, Sussel L (2019) β Cell dysfunction during progression of metabolic syndrome to type 2 diabetes. J Clin Investig 129(10):4001–4008
Avrahami D, Klochendler A, Dor Y, Glaser B (2017) Beta cell heterogeneity: an evolving concept. Diabetologia 60(8):1363–1369
Liu PF, Chen CF, Shu CW et al (2020) UBE2C is a potential biomarker for tumorigenesis and prognosis in tongue squamous cell carcinoma. Diagnostics (Basel). https://doi.org/10.3390/diagnostics10090674
Chiang AJ, Li CJ, Tsui KH, Chang C, Sheu JC (2020) UBE2C drives human cervical cancer progression and is positively modulated by mTOR. Biomolecules 11(1):37
Tessem JS, Moss LG, Chao LC et al (2014) Nkx6.1 regulates islet β-cell proliferation via Nr4a1 and Nr4a3 nuclear receptors. Proc Natl Acad Sci USA 111(14):5242–5247. https://doi.org/10.1073/pnas.1320953111
Gao R, Fu Q, Jiang HM et al (2021) Temporal metabolic and transcriptomic characteristics crossing islets and liver reveal dynamic pathophysiology in diet-induced diabetes. iScience 24(4):102265. https://doi.org/10.1016/j.isci.2021.102265
Xiao X, Guo P, Prasadan K et al (2014) Pancreatic cell tracing, lineage tagging and targeted genetic manipulations in multiple cell types using pancreatic ductal infusion of adeno-associated viral vectors and/or cell-tagging dyes. Nat Protoc 9(12):2719–2724. https://doi.org/10.1038/nprot.2014.183
Wu T, Zhang S, Xu J et al (2020) HRD1, an important player in pancreatic β-cell failure and therapeutic target for type 2 diabetic mice. Diabetes 69(5):940–953. https://doi.org/10.2337/db19-1060
Pagala VR, High AA, Wang X et al (2015) Quantitative protein analysis by mass spectrometry. Methods Mol Biol (Clifton, NJ) 1278:281–305. https://doi.org/10.1007/978-1-4939-2425-7_17
Gao R, Fu Q, Jiang HM et al (2021) Temporal metabolic characteristics and transcriptomic landscape of islets and liver reveal dynamic pathophysiology and interorgan crosstalk in high-fat diet-induced diabetes. iScience 24(4):102265
Fu Q, Jiang H, Qian Y et al (2023) Single-cell RNA sequencing combined with single-cell proteomics identifies the metabolic adaptation of islet cell subpopulations to high-fat diet in mice. Diabetologia 66(4):724–740. https://doi.org/10.1007/s00125-022-05849-5
Kobak D, Berens P (2019) The art of using t-SNE for single-cell transcriptomics. Nat Commun 10(1):5416. https://doi.org/10.1038/s41467-019-13056-x
Subelj L, Bajec M (2011) Unfolding communities in large complex networks: combining defensive and offensive label propagation for core extraction. Phys Rev E Stat Nonlin Soft Matter Phys 83(3 Pt 2):036103. https://doi.org/10.1103/PhysRevE.83.036103
Fu Q, Jiang H, Qian Y et al (2022) Single-cell RNA sequencing combined with single-cell proteomics identifies the metabolic adaptation of islet cell subpopulations to high-fat diet in mice. Diabetologia 66(4):724–740
Fasolino M, Schwartz GW, Patil AR et al (2022) Single-cell multi-omics analysis of human pancreatic islets reveals novel cellular states in type 1 diabetes. Nat Metab 4(2):284–299. https://doi.org/10.1038/s42255-022-00531-x
Oraha J, Enriquez RF, Herzog H, Lee NJ (2022) Sex-specific changes in metabolism during the transition from chow to high-fat diet feeding are abolished in response to dieting in C57BL/6J mice. Int J Obes (2005) 46(10):1749–1758. https://doi.org/10.1038/s41366-022-01174-4
Gery S, Komatsu N, Baldjyan L, Yu A, Koeffler HP (2006) The circadian gene Per1 plays an important role in cell growth and DNA damage control in human cancer cells. Mol Cell 22(3):375–382
Shirogane T, Jin J, Ang XL, Harper JW (2005) SCFβ-TRCP controls clock-dependent transcription via casein kinase 1-dependent degradation of the mammalian period-1 (Per1) proteinm. Jbiolchem 280(29):26863
Zhong F, Jiang Y (2019) Endogenous pancreatic β cell regeneration: a potential strategy for the recovery of β cell deficiency in diabetes. Front Endocrinol 10:101. https://doi.org/10.3389/fendo.2019.00101
Zhao H, Huang X, Liu Z et al (2021) Pre-existing beta cells but not progenitors contribute to new beta cells in the adult pancreas. Nat Metab 3(3):352–365. https://doi.org/10.1038/s42255-021-00364-0
Feng Y, Qiu WL, Yu XX et al (2020) Characterizing pancreatic β-cell heterogeneity in the streptozotocin model by single-cell transcriptomic analysis. Mol Metab 37:100982. https://doi.org/10.1016/j.molmet.2020.100982
Tschen SI, Dhawan S, Gurlo T, Bhushan A (2009) Age-dependent decline in beta-cell proliferation restricts the capacity of beta-cell regeneration in mice. Diabetes 58(6):1312–1320. https://doi.org/10.2337/db08-1651
Dorrell C, Schug J, Canaday PS et al (2016) Human islets contain four distinct subtypes of β cells. Nat Commun 7:11756. https://doi.org/10.1038/ncomms11756
Klochendler A, Caspi I, Corem N et al (2016) The genetic program of pancreatic β-cell replication in vivo. Diabetes 65(7):2081–2093
Ruijtenberg S, Sander VDH (2016) Coordinating cell proliferation and differentiation: antagonism between cell cycle regulators and cell type-specific gene expression. Cell Cycle 15(2):196–212
Ma J, Xing B, Cao Y et al (2021) Menin-regulated Pbk controls high fat diet-induced compensatory beta cell proliferation. EMBO Mol Med 13(5):e13524. https://doi.org/10.1525/emmm.202013524
Ben-Eliezer I, Pomerantz Y, Galiani D, Nevo N, Dekel N (2015) Appropriate expression of Ube2C and Ube2S controls the progression of the first meiotic division. FASEB J 29(11):4670–4681. https://doi.org/10.1096/fj.15-274522
Ye Y, Rape M (2009) Building ubiquitin chains: E2 enzymes at work. Nat Rev Mol Cell Biol 10(11):755–764. https://doi.org/10.1038/nrm2780
Xie J, Jin Y, Wang G (2019) The role of SCF ubiquitin-ligase complex at the beginning of life. Reprod Biol Endocrinol 17(1):101. https://doi.org/10.1186/s12958-019-0547-y
Shirogane T, Jin J, Ang XL, Harper JW (2005) SCFbeta-TRCP controls clock-dependent transcription via casein kinase 1-dependent degradation of the mammalian period-1 (Per1) protein. J Biol Chem 280(29):26863–26872. https://doi.org/10.1074/jbc.M502862200
Reppert SM, Weaver DR (2001) Molecular analysis of mammalian circadian rhythms. Annu Rev Physiol 63(1):647
Yagita K (2001) Molecular mechanisms of the biological clock in cultured fibroblasts. Science 292(5515):278–281
Farshadi E, van der Horst GTJ, Chaves I (2020) Molecular links between the circadian clock and the cell cycle. J Mol Biol 432(12):3515–3524. https://doi.org/10.1016/j.jmb.2020.04.003
Takahashi JS (2017) Transcriptional architecture of the mammalian circadian clock. Nat Rev Genet 18(3):164–179. https://doi.org/10.1038/nrg.2016.150
Ko CH, Takahashi JS (2006) Molecular components of the mammalian circadian clock. Hum Mol Genet 15(Spec No 2):R271–R277. https://doi.org/10.1093/hmg/ddl207
Rakshit K, Hsu TW, Matveyenko AV (2016) Bmal1 is required for beta cell compensatory expansion, survival and metabolic adaptation to diet-induced obesity in mice. Diabetologia 59(4):734–743. https://doi.org/10.1007/s00125-015-3859-2
Marcheva B, Ramsey KM, Buhr ED et al (2010) Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature 466(7306):627–631. https://doi.org/10.1038/nature09253
Zhao Y, Zhang Y, Zhou M, Wang S, Hua Z, Zhang J (2012) Loss of mPer2 increases plasma insulin levels by enhanced glucose-stimulated insulin secretion and impaired insulin clearance in mice. FEBS Lett 586(9):1306–1311. https://doi.org/10.1016/j.febslet.2012.03.034
Wang HL, Wei B, He HJ et al (2022) Smad3 deficiency improves islet-based therapy for diabetes and diabetic kidney injury by promoting β cell proliferation via the E2F3-dependent mechanism. Theranostics 12(1):379–395. https://doi.org/10.7150/thno.67034
Hoshino A, Ariyoshi M, Okawa Y et al (2014) Inhibition of p53 preserves Parkin-mediated mitophagy and pancreatic β-cell function in diabetes. Proc Natl Acad Sci USA 111(8):3116–3121. https://doi.org/10.1073/pnas.1318951111
Acknowledgements
The authors wish to thank all research staff in Department of Endocrinology of the First Affiliated Hospital of Nanjing Medical University who participated in this work. They would like to thank the Core Facility of the First Affiliated Hospital of Nanjing Medical University for its help in the experiment. They would like to thank Professor Hongxing Fu from Shulan (Hangzhou) Hospital Affiliated to Zhejiang Shuren University Shulan International Medical College for providing the human pancreas slice samples.
Funding
This work was supported by the National Natural Science Foundation of China (81830023, 82070803 and 82100837).
Author information
Authors and Affiliations
Contributions
QF and TY directed the study and were responsible for study design and overall project management. HJ, SZ, YQ and YZ performed statistical analyses, participated in study design, and drafted the manuscript. HD, YL, YZ, YH, JZ, ZX, and RG analysed the data. HL, WB, and KX contributed to conception, design, and interpretation of this work. All the authors approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Ethical approval
Animal use procedures were approved (IACUC1804001) by the Medicine Animal Care Committee of Nanjing Medical University. Experiments were conducted in accordance with relevant institutional guidelines and regulations.
Consent for publication
All the authors read and approved the submission and final publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, H., Zheng, S., Qian, Y. et al. Restored UBE2C expression in islets promotes β-cell regeneration in mice by ubiquitinating PER1. Cell. Mol. Life Sci. 80, 226 (2023). https://doi.org/10.1007/s00018-023-04868-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00018-023-04868-8