Abstract
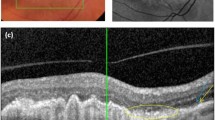
Prolonged life expectancies contribute to the increasing prevalence of age-related macular degeneration (AMD) that is already the leading cause of severe vision loss among the elderly in developed countries. In dry AMD, the disease culminates into vast retinal atrophy, whereas the wet form is characterized by retinal edema and sudden vision loss due to neovascularization originating from the choroid beneath the Bruch’s membrane. There is no treatment for dry AMD and despite intravitreal injections of anti-vascular endothelial growth factor (VEGF) that suppress the neovessel formation, also wet AMD needs new therapies to prevent the disease progression and to serve patients lacking of positive response to current medicines. Knowledge on disease mechanisms is a prerequisite for the drug development, which is hindered by the multifactorial nature of AMD. Numerous distinguished publications have revealed AMD mechanisms at the cellular and molecular level and in this multi-author review, we take a bit broader look at the topic with some novel aspects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Age-related macular degeneration (AMD) is an ocular disease localizing mainly at the macular area, which is responsible for central and sharp vision at the posterior part of the eye. The disease impairs, e.g. abilities to read, dial numbers, recognize faces and thereby, it severely compromises independency in daily tasks [3]. Loss of photoreceptors is preceded by the dysfunctionality and death of retinal pigment epithelium (RPE) cells that normally form a solid single-cell layer between photoreceptors and the Bruch’s membrane. Reasons for the RPE degeneration are diverse but immune dysfunction, oxidative stress, mitochondrial damage, disturbed proteostasis, complement activation, and inflammation constantly recur in publications [1, 3, 6, 8,9,10,11,12, 16, 19]. Despite the central role of the RPE, cells of innate and adaptive immunity are also involved in the pathogenesis of AMD. Chemokines secreted upon retinal damage recruit resident microglia as well as systemic leukocytes to the subretinal area [3]. Here, Verena Behnke et al. provide insight into the role of immune cells in AMD.
In a systematic meta-analysis with 16 identified risk factors, aging, current smoking, cataract surgery, and a family history were strongly associated with late AMD that can be divided into dry and wet forms [4, 5]. Also, cardiovascular disease-related factors, such as hypertension, and a history with cardiovascular disease were observed as significant risk factors for AMD [5]. Aging is a strong prerequisite for AMD, the prevalence of which is low in people under 60 years [20]. Aging is associated with cellular senescence [7] that is contemplated in this multi-author review (MAR) by Janusz Błasiak in relation to premises of RPE cells upon stressful conditions.
In addition to environmental risk factors, genetic predisposition is associated with AMD and especially immune modulation and complement system are represented among susceptibility genes [15]. It has been observed that the role of genetic factors ranges from 46 to 71% in AMD [17, 20]. Nowadays, it is known that in addition to inherited genes, epigenetic modulation can change gene activity and expression without altering the DNA sequence [21]. Contribution of epigenetics is a very current topic in which interest also in relation to AMD is increasing, and that subject is covered here by Maria Gemenetzi and Andrew Lotery.
Intracellular accumulation of lipofuscin in lysosomes and extracellular drusen deposits between the RPE and the Bruch’s membrane are the first clinical signs observed upon diagnosis of AMD [14]. Drusen and retinal edema are included in factors resulting in hypoxia found in AMD eyes [18]. The role of hypoxia in ocular neovascularization has recently been reviewed elsewhere [2] and in this MAR, hypoxia is considered from the perspective of gene therapy by Parviz Mammadzada et al.
Lipocalin-2 (LCN-2) belongs to the lipocalin protein family, the members of which share evolutionarily conserved eight-stranded antiparallel β-sheet “barrel” structure with capacity to bind small hydrophobic ligands [13]. LCN-2 is associated with infections, acute inflammation, as well as several chronic diseases [13]. Its role in AMD has not gained much attention but is now being compiled by Sayan Ghosh et al.
RPE cells are in the central role in the pathogenesis of AMD but several important players beyond them must also be taken into account when considering this multifactorial disease. This multi-author review presents AMD from other perspectives deepening the understanding on its pathogenesis and providing views for new therapy options.
References
Akhtar-Schafer I, Wang L, Krohne TU, Xu H, Langmann T (2018) Modulation of three key innate immune pathways for the most common retinal degenerative diseases. EMBO Mol Med. https://doi.org/10.15252/emmm.201708259
Alizadeh E, Mammadzada P, Andre H (2018) The different facades of retinal and choroidal endothelial cells in response to hypoxia. Int J Mol Sci. https://doi.org/10.3390/ijms19123846
Ambati J, Atkinson JP, Gelfand BD (2013) Immunology of age-related macular degeneration. Nat Rev Immunol 13:438–451
Ardeljan D, Chan CC (2013) Aging is not a disease: distinguishing age-related macular degeneration from aging. Prog Retin Eye Res 37:68–69
Chakravarthy U, Wong TY, Fletcher A, Piault E, Evans C, Zlateva G, Buggage R, Pleil A, Mitchell P (2010) Clinical risk factors for age-related macular degeneration: a systematic review and meta-analysis. BMC Ophthalmol 10:31
Chen M, Luo C, Zhao J, Devarajan G, Xu H (2019) Immune regulation in the aging retina. Prog Retin Eye Res 69:159–172
Childs BG, Durik M, Baker DJ, van Deursen JM (2015) Cellular senescence in aging and age-related disease: from mechanisms to therapy. Nat Med 21:1424–1435
Copland DA, Theodoropoulou S, Liu J, Dick AD (2018) A perspective of AMD through the eyes of immunology. Investig Ophthalmol Vis Sci 59:AMD83–AMD92
Ferrington DA, Sinha D, Kaarniranta K (2016) Defects in retinal pigment epithelial cell proteolysis and the pathology associated with age-related macular degeneration. Prog Retin Eye Res 51:69–89
Kauppinen A, Paterno JJ, Blasiak J, Salminen A, Kaarniranta K (2016) Inflammation and its role in age-related macular degeneration. Cell Mol Life Sci 73:1765–1786
Kauppinen A (2017) Mitochondria-associated inflammasome activation and its impact on aging and age-related diseases. In: Fulop T, Franceschi C, Hirokawa K, Pawelec G (eds) Handbook of immunosenescence: basic understanding and clinical implications. Springer International Publishing, Cham, pp 1–20
Lefevere E, Toft-Kehler AK, Vohra R, Kolko M, Moons L, Van Hove I (2017) Mitochondrial dysfunction underlying outer retinal diseases. Mitochondrion 36:66–76
Li D, Yan Sun W, Fu B, Xu A, Wang Y (2019) Lipocalin-2—the myth of its expression and function. Basic Clin Pharmacol Toxicol. https://doi.org/10.1111/bcpt.13332
Lim LS, Mitchell P, Seddon JM, Holz FG, Wong TY (2012) Age-related macular degeneration. Lancet 379:1728–1738
Mousavi M, Armstrong RA (2013) Genetic risk factors and age-related macular degeneration (AMD). J Optom 6:176–184
Salminen A, Ojala J, Kaarniranta K, Kauppinen A (2012) Mitochondrial dysfunction and oxidative stress activate inflammasomes: impact on the aging process and age-related diseases. Cell Mol Life Sci 69:2999–3013
Seddon JM, Ajani UA, Mitchell BD (1997) Familial aggregation of age-related maculopathy. Am J Ophthalmol 123:199–206
Stefansson E, Geirsdottir A, Sigurdsson H (2011) Metabolic physiology in age related macular degeneration. Prog Retin Eye Res 30:72–80
Sugita S, Horie S, Yamada Y, Mochizuki M (2010) Inhibition of B-cell activation by retinal pigment epithelium. Investig Ophthalmol Vis Sci 51:5783–5788
Warwick A, Lotery A (2018) Genetics and genetic testing for age-related macular degeneration. Eye (Lond) 32:849–857
Weinhold B (2006) Epigenetics: the science of change. Environ Health Perspect 114:A160–A167
Acknowledgements
Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kauppinen, A. Introduction to the multi-author review on macular degeneration. Cell. Mol. Life Sci. 77, 779–780 (2020). https://doi.org/10.1007/s00018-019-03418-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-019-03418-5