Abstract
Introduction
Autoinflammatory diseases (AIDs) constitute several disorders that are characterized by the presence of recurrent episodes of unprovoked inflammation due to dysregulated innate immune system in the absence of autoantibodies or infections. Most of them have a strong genetic background, with mutations in single genes involved in inflammation referred to monogenic AIDs. In this article, we will review the cardiac manifestations in various monogenic AIDs.
Areas covered
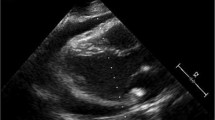
Various cardiac manifestations can be seen in various monogenic AIDs, including pericarditis, valvular diseases, coronary diseases, cardiomyopathies, and pulmonary hypertension, especially in Familial Mediterranean fever (FMF).
Expert commentary
Monogenic AIDs can manifest a variety of cardiac lesions, the most common of which is pericardial effusion, which may be local pericardial inflammation secondary to systemic inflammatory responses. While, the pathogenesis and incidence are still unclear. More research is still needed to explore the relationship between monogenic AIDs and cardiac damage for better understanding these diseases.

Similar content being viewed by others
Data availability
Not applicable.
References
Krainer J, Siebenhandl S, Weinhäusel A. Systemic autoinflammatory diseases. J Autoimmun. 2020;109:102421. https://doi.org/10.1016/j.jaut.2020.102421. (Epub 2020 Feb 1. PMID: 32019685; PMCID: PMC7610735).
Di Donato G, d’Angelo DM, Breda L, Chiarelli F. Monogenic autoinflammatory diseases: state of the art and future perspectives. Int J Mol Sci. 2021;22(12):6360. https://doi.org/10.3390/ijms22126360. (PMID: 34198614; PMCID: PMC8232320).
Tangye SG, Al-Herz W, Bousfiha A, Chatila T, Cunningham-Rundles C, Etzioni A, Franco JL, Holland SM, Klein C, Morio T, Ochs HD, Oksenhendler E, Picard C, Puck J, Torgerson TR, Casanova JL, Sullivan KE. Human inborn errors of immunity: 2019 update on the classification from the International Union of Immunological Societies Expert Committee. J Clin Immunol. 2020;40(1):24–64. https://doi.org/10.1007/s10875-019-00737-x. (Epub 2020 Jan 17. Erratum in: J Clin Immunol. 2020 Feb 22; PMID: 31953710; PMCID: PMC7082301).
Theofilopoulos AN, Gonzalez-Quintial R, Lawson BR, Koh YT, Stern ME, Kono DH, Beutler B, Baccala R. Sensors of the innate immune system: their link to rheumatic diseases. Nat Rev Rheumatol. 2010;6(3):146–56. https://doi.org/10.1038/nrrheum.2009.278. (Epub 2010 Feb 9. PMID: 20142813; PMCID: PMC4437225).
Shen M, Wu D, Zeng X. Clinical and genetic phenotypes of Chinese patients with adult autoinflammatory diseases: report from an adult reference centre. Chin J Allergy Clin Immunol. 2016;10(04):325–33.
Qijiao W, Hongmei S. Progress of inflammasome disease. Chin J Rheumatol. 2018;22(12):847–51.
Shin JI, Lee KH, Joo YH, Lee JM, Jeon J, Jung HJ, Shin M, Cho S, Kim TH, Park S, Jeon BY, Jeong H, Lee K, Kang K, Oh M, Lee H, Lee S, Kwon Y, Oh GH, Kronbichler A. Inflammasomes and autoimmune and rheumatic diseases: a comprehensive review. J Autoimmun. 2019;103:102299. https://doi.org/10.1016/j.jaut.2019.06.010. (Epub 2019 Jul 17. PMID: 31326231).
Ozen S. Update in familial Mediterranean fever. Curr Opin Rheumatol. 2021;33(5):398–402. https://doi.org/10.1097/BOR.0000000000000821. (PMID: 34397603).
Alsarah A, Alsara O, Laird-Fick HS. Cardiac manifestations of Familial Mediterranean fever. Avicenna J Med. 2017;7(4):158–63. https://doi.org/10.4103/ajm.AJM_78_17. (PMID: 29119082; PMCID: PMC5655646).
Erken E, Erken E. Cardiac disease in familial Mediterranean fever. Rheumatol Int. 2018;38(1):51–8. https://doi.org/10.1007/s00296-017-3853-8. (Epub 2017 Oct 20; PMID: 29051974).
Shohat M. Familial Mediterranean fever. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Mirzaa GM, Amemiya A, editors. GeneReviews® [Internet]. Seattle: University of Washington; 2000. p. 1993–2022 (PMID: 20301405; updated 2016 Dec 15).
Imazio M, Brucato A, Pluymaekers N, Breda L, Calabri G, Cantarini L, Cimaz R, Colimodio F, Corona F, Cumetti D, Cuccio CD, Gattorno M, Insalaco A, Limongelli G, Russo MG, Valenti A, Finkelstein Y, Martini A. Recurrent pericarditis in children and adolescents: a multicentre cohort study. J Cardiovasc Med (Hagerstown). 2016;17(9):707–12. https://doi.org/10.2459/JCM.0000000000000300. (PMID: 27467459).
Kilic A, Varkal MA, Durmus MS, Yildiz I, Yıldırım ZN, Turunc G, Oguz F, Sidal M, Omeroglu RE, Emre S, Yilmaz Y, Kelesoglu FM, Gencay GA, Temurhan S, Aydin F, Unuvar E. Relationship between clinical findings and genetic mutations in patients with familial Mediterranean fever. Pediatr Rheumatol Online J. 2015;12(13):59. https://doi.org/10.1186/s12969-015-0057-1. (PMID: 26759267; PMCID: PMC4711108).
Basar N, Kisacik B, Ercan S, Pehlivan Y, Yilmaz S, Simsek I, Erdem H, Ozer O, Pay S, Onat AM, Dinc A. Familial Mediterranean fever gene mutations as a risk factor for early coronary artery disease. Int J Rheum Dis. 2017;20(12):2113–7. https://doi.org/10.1111/1756-185X.12356. (Epub 2014 Apr 7 PMID: 24702757).
Gendelman O, Shapira R, Tiosano S, Pras E, Comaneshter D, Cohen A, Amital H. Familial Mediterranean fever is associated with increased risk for ischaemic heart disease and mortality—perspective derived from a large database. Int J Clin Pract. 2020;74(5):e13473. https://doi.org/10.1111/ijcp.13473. (Epub 2020 Jan 13. PMID: 31909853).
Malik J, Shabbir A, Nazir A. Cardiovascular sequelae and genetics of familial mediterranean fever: a literature review. Pulse (Basel). 2021;8(3–4):78–85. https://doi.org/10.1159/000516182. (Epub 2021 Jun 3. PMID: 34307203; PMCID: PMC8280401).
Ceylan Ö, Ceylan Y. Intermittent right bundle branch block in a child with familial mediterranean fever. Cardiol J. 2018;25(6):753–5. https://doi.org/10.5603/CJ.2018.0154. (PMID: 30600838).
Ambartsymian SV. Myocardial infarction in patients with familial Mediterranean fever and cardiac lesions. Georgian Med News. 2012;204:62–6 (PMID: 22573751).
Johnson WJ, Lie JT. Pulmonary hypertension and familial Mediterranean fever: a previously unrecognized association. Mayo Clin Proc. 1991;66(9):919–25. https://doi.org/10.1016/s0025-6196(12)61579-1. (PMID: 1921502).
Salah S, Hegazy R, Ammar R, Sheba H, Abdelrahman L. MEFV gene mutations and cardiac phenotype in children with familial Mediterranean fever: a cohort study. Pediatr Rheumatol Online J. 2014;16(12):5. https://doi.org/10.1186/1546-0096-12-5. (PMID: 24433404; PMCID: PMC3931676).
Sözeri B, Gerçeker-Türk B, Yıldız-Atıkan B, Mir S, Berdeli A. A novel mutation of interleukin-1 receptor antagonist (IL1RN) in a DIRA patient from Turkey: diagnosis and treatment. Turk J Pediatr. 2018;60(5):588–92. https://doi.org/10.24953/turkjped.2018.05.020. (PMID: 30968643).
Hospach T, Glowatzki F, Blankenburg F, Conzelmann D, Stirnkorb C, Müllerschön CS, von den Driesch P, Köhler LM, Rohlfs M, Klein C, Hauck F. Scoping review of biological treatment of deficiency of interleukin-36 receptor antagonist (DITRA) in children and adolescents. Pediatr Rheumatol Online J. 2019;17(1):37. https://doi.org/10.1186/s12969-019-0338-1. (PMID: 31286990; PMCID: PMC6615208).
Zhi Y, Jun Y. Research progress in haploinsufficiency of A20. Chin J Pediatr. 2019;57(12):970–3.
Cudrici C, Deuitch N, Aksentijevich I. Revisiting TNF receptor-associated periodic syndrome (TRAPS): current perspectives. Int J Mol Sci. 2020;21(9):3263. https://doi.org/10.3390/ijms21093263. (PMID: 32380704; PMCID: PMC7246474).
Rigante D, Capoluongo E. The plodding diagnosis of monogenic autoinflammatory diseases in childhood: from the clinical scenery to laboratory investigation. Clin Chem Lab Med. 2011;49(5):783–91. https://doi.org/10.1515/CCLM.2011.127. (Epub 2011 Jan 31; PMID: 21275813).
Torrelo A. CANDLE syndrome as a paradigm of proteasome-related autoinflammation. Front Immunol. 2017;9(8):927. https://doi.org/10.3389/fimmu.2017.00927. (PMID: 28848544; PMCID: PMC5552674).
Torrelo A, Patel S, Colmenero I, Gurbindo D, Lendínez F, Hernández A, López-Robledillo JC, Dadban A, Requena L, Paller AS. Chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature (CANDLE) syndrome. J Am Acad Dermatol. 2010;62(3):489–95. https://doi.org/10.1016/j.jaad.2009.04.046. (PMID: 20159315).
Chouk H, Ben Rejeb M, Boussofara L, Elmabrouk H, Ghariani N, Sriha B, Saad A, H’Mida D, Denguezli M. Phenotypic intrafamilial variability including H syndrome and Rosai-Dorfman disease associated with the same c.1088G > a mutation in the SLC29A3 gene. Hum Genomics. 2021;15(1):63. https://doi.org/10.1186/s40246-021-00362-z. (PMID: 34657628; PMCID: PMC8522101).
El-Bassyouni HT, Thomas MM, Tosson AMS. Mutation in the SLC29A3 gene in an Egyptian patient with H syndrome: a case report and review of literature. J Pediatr Genet. 2020;9(2):109–13. https://doi.org/10.1055/s-0039-1697900. (Epub 2019 Sep 30. PMID: 32341814; PMCID: PMC7183402).
Meena D, Chauhan P, Hazarika N, Kansal NK. H syndrome: a case report and review of literature. Indian J Dermatol. 2018;63(1):76–8. https://doi.org/10.4103/ijd.IJD_264_17. (PMID: 29527032; PMCID: PMC5838761).
Tekin B, Atay Z, Ergun T, Can M, Tuney D, Babay S, Turan S, Bereket A, Zlotogorski A, Molho-Pessach V. H syndrome: a multifaceted histiocytic disorder with hyperpigmentation and hypertrichosis. Acta Derm Venereol. 2015;95(8):1021–3. https://doi.org/10.2340/00015555-2145. (PMID: 26015165).
Zhongxun Yu, Hongmei S. Elucidate on type I interferonopathies. Chin J Appl Clin Pediatr. 2022;37(01):2–5.
Jun JU, Li-Ping ZOU. Research progress of correlation between adenosine deaminase 2 (ADA2) and Vasculiti. Chin J Stroke. 2014;9(10):864–8.
Caorsi R, Penco F, Schena F, Gattorno M. Monogenic polyarteritis: the lesson of ADA2 deficiency. Pediatr Rheumatol Online J. 2016;14(1):51. https://doi.org/10.1186/s12969-016-0111-7. (PMID: 27609179; PMCID: PMC5015262).
Riazi AM, Van Arsdell G, Buchwald M. Transgenic expression of CECR1 adenosine deaminase in mice results in abnormal development of heart and kidney. Transgenic Res. 2005;14(3):333–6. https://doi.org/10.1007/s11248-005-1174-2. (PMID: 16145841).
Tingyan He, Jun Y. Aicardi–Goutières syndrome. Chin J Pract Pediatr. 2018;33(01):29–33. https://doi.org/10.19538/j.ek2018010609.
Livingston JH, Crow YJ. Neurologic phenotypes associated with mutations in TREX1, RNASEH2A, RNASEH2B, RNASEH2C, SAMHD1, ADAR1, and IFIH1: Aicardi–Goutières syndrome and beyond. Neuropediatrics. 2016;47(6):355–60. https://doi.org/10.1055/s-0036-1592307. (Epub 2016 Sep 19 PMID: 27643693).
King KR, Aguirre AD, Ye YX, Sun Y, Roh JD, Ng RP Jr, Kohler RH, Arlauckas SP, Iwamoto Y, Savol A, Sadreyev RI, Kelly M, Fitzgibbons TP, Fitzgerald KA, Mitchison T, Libby P, Nahrendorf M, Weissleder R. IRF3 and type I interferons fuel a fatal response to myocardial infarction. Nat Med. 2017;23(12):1481–7. https://doi.org/10.1038/nm.4428. (Epub 2017 Nov 6. PMID: 29106401; PMCID: PMC6477926).
Frémond ML, Crow YJ. STING-mediated lung inflammation and beyond. J Clin Immunol. 2021;41(3):501–14. https://doi.org/10.1007/s10875-021-00974-z. (Epub 2021 Feb 2; PMID: 33532887).
Frémond ML, Hadchouel A, Berteloot L, Melki I, Bresson V, Barnabei L, Jeremiah N, Belot A, Bondet V, Brocq O, Chan D, Dagher R, Dubus JC, Duffy D, Feuillet-Soummer S, Fusaro M, Gattorno M, Insalaco A, Jeziorski E, Kitabayashi N, Lopez-Corbeto M, Mazingue F, Morren MA, Rice GI, Rivière JG, Seabra L, Sirvente J, Soler-Palacin P, Stremler-Le Bel N, Thouvenin G, Thumerelle C, Van Aerde E, Volpi S, Willcocks S, Wouters C, Breton S, Molina T, Bader-Meunier B, Moshous D, Fischer A, Blanche S, Rieux-Laucat F, Crow YJ, Neven B. Overview of STING-associated vasculopathy with onset in infancy (SAVI) among 21 patients. J Allergy Clin Immunol Pract. 2021;9(2):803-818.e11. https://doi.org/10.1016/j.jaip.2020.11.007. (Epub 2020 Nov 18; PMID: 33217613).
Funding
No funding is available.
Author information
Authors and Affiliations
Contributions
WQ drafted the article. SL approved the final version of manuscript. She also revised the manuscript carefully.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Responsible Editor: John Di Battista.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wei, Q., Sun, L. Monogenic autoinflammatory disease-associated cardiac damage. Inflamm. Res. 72, 1689–1693 (2023). https://doi.org/10.1007/s00011-023-01771-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-023-01771-7