Abstract
Objective and design
The aim of this study was to determine whether different generations (G) polyamidoamine (PAMAM) dendrimers possess proinflammatory activities in vivo.
Material or subjects
Several hundred female CD-1 mice were used to test four different PAMAM dendrimers using the murine air pouch model.
Treatment
Mice received appropriate negative and positive controls or G0-G3 PAMAM nanoparticles at 100 and 500 µg/ml into air pouches.
Methods
Exudates were harvested after 3, 6, 24 and 48 h. Cell pellets and supernatants were used to determine the number of total leukocytes and neutrophils and to detect the production of several analytes by an antibody array approach, respectively. One-way analysis of variance was used for statistical analysis.
Results
PAMAM dendrimers rapidly increased a leukocyte influx after 3 h, the vast majority of cells being neutrophils. This was also observed after 6 and 24 h, and resolution of inflammation was noted after 48 h. In general, the increased production of a greater number of analytes detected in the exudates after 6 h correlated with the number of dendrimer generations (G3 > G2 > G1 > G0).
Conclusions
PAMAM dendrimers devoid of any delivering molecules possess proinflammatory activities in vivo by themselves, probably via the production of different chemokines released by air pouch lining cells.






Similar content being viewed by others
References
Labieniec-Watala M, Watala C. PAMAM dendrimers: destined for success or doomed to fail? Plain and modified PAMAM dendrimers in the context of biomedical applications. J Pharm Sci. 2015;104:2–14.
Mintzer MA, Grinstaff MW. Biomedical applications of dendrimers: a tutorial. Chem Soc Rev. 2011;40:173–90.
Eichman JD, Bielinska AU, Kukowska-Latallo JF, Baker JR Jr. The use of PAMAM dendrimers in the efficient transfer of genetic material into cells. Pharm Sci Technol Today. 2000;3:232–45.
Inapagolla R, Guru BR, Kurtoglu YE, Gao X, Lieh-Lai M, Bassett DJ, et al. In vivo efficacy of dendrimer-methylprednisolone conjugate formulation for the treatment of lung inflammation. Int J Pharm. 2010;399:140–7.
Benchaala I, Mishra MK, Wykes SM, Hali M, Kannan RM, Whittum-Hudson JA. Folate-functionalized dendrimers for targeting Chlamydia-infected tissues in a mouse model of reactive arthritis. Int J Pharm. 2014;466:258–65.
Wang S, Li Y, Fan J, Wang Z, Zeng X, Sun Y, et al. The role of autophagy in the neurotoxicity of cationic PAMAM dendrimers. Biomaterials. 2014;35:7588–97.
Uram L, Szuster M, Gargasz K, Filipowicz A, Walajtys-Rode E, Wolowiec S. In vitro cytotoxicity of the ternary PAMAM G3-pyridoxal-biotin bioconjugate. Int J Nanomed. 2013;8:4707–20.
Ozturk K, Erturk AS, Sarisozen C, Tulu M, Calis S. Cytotoxicity and in vitro characterization studies of synthesized Jeffamine-cored PAMAM dendrimers. J Microencapsul. 2014;31:127–36.
Goncalves M, Castro R, Rodrigues J, Tomas H. The effect of PAMAM dendrimers on mesenchymal stem cell viability and differentiation. Curr Med Chem. 2012;19:4969–75.
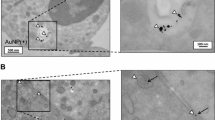
Vandooren J, Berghmans N, Dillen C, Van Aelst I, Ronsse I, Israel LL, et al. Intradermal air pouch leukocytosis as an in vivo test for nanoparticles. Int J Nanomed. 2013;8:4745–56.
Girard D. Using the air pouch model for assessing in vivo inflammatory activity of nanoparticles. Int J Nanomed. 2014;9:1105–7.
Goncalves DM, Girard D. Titanium dioxide (TiO(2)) nanoparticles induce neutrophil influx and local production of several proinflammatory mediators in vivo. Int Immunopharmacol. 2011;21:21.
Goncalves DM, Girard D. Evidence that polyhydroxylated C60 fullerenes (fullerenols) amplify the effect of lipopolysaccharides to induce rapid leukocyte infiltration in vivo. Chem Res Toxicol. 2013;26:1884–92.
Babin K, Antoine F, Goncalves DM, Girard D. TiO2, CeO2 and ZnO nanoparticles and modulation of the degranulation process in human neutrophils. Toxicol Lett. 2013;221:57–63.
Ratthe C, Ennaciri J, Garces Goncalves DM, Chiasson S, Girard D. Interleukin (IL)-4 induces leukocyte infiltration in vivo by an indirect mechanism. Mediators Inflamm 2009; 2009:193970.
Dobrovolskaia MA, Neun BW, Clogston JD, Ding H, Ljubimova J, McNeil SE. Ambiguities in applying traditional Limulus amebocyte lysate tests to quantify endotoxin in nanoparticle formulations. Nanomedicine (London, England) 2010; 5:555–62.
Moisan E, Chiasson S, Girard D. The intriguing normal acute inflammatory response in mice lacking vimentin. Clin Exp Immunol. 2007;150:158–68.
Ratthe C, Ennaciri J, Garces Goncalves DM, Chiasson S, Girard D. Interleukin (IL)-4 induces leukocyte infiltration in vivo by an indirect mechanism. Mediators Inflamm. 2009;193970:10.
Pelletier M, Bouchard A, Girard D. In vivo and in vitro roles of IL-21 in inflammation. J Immunol. 2004;173:7521–30.
Antoine F, Simard JC, Girard D. Curcumin inhibits agent-induced human neutrophil functions in vitro and lipopolysaccharide-induced neutrophilic infiltration in vivo. Int Immunopharmacol. 2013;17:1101–7.
Lavastre V, Cavalli H, Ratthe C, Girard D. Anti-inflammatory effect of Viscum album agglutinin-I (VAA-I): induction of apoptosis in activated neutrophils and inhibition of lipopolysaccharide-induced neutrophilic inflammation in vivo. Clin Exp Immunol. 2004;137:272–8.
Pelletier M, Girard D. Biological functions of interleukin-21 and its role in inflammation. Sci World J. 2007;7:1715–35.
Escribano E, Fernandez-Pacheco R, Valdivia JG, Ibarra MR, Marquina C, Queralt J. Effect of magnet implant on iron biodistribution of Fe@C nanoparticles in the mouse. Arch Pharm Res. 2012;35:93–100.
Kroll A, Pillukat MH, Hahn D, Schnekenburger J. Interference of engineered nanoparticles with in vitro toxicity assays. Arch Toxicol. 2012;86:1123–36.
Oh SJ, Kim H, Liu Y, Han HK, Kwon K, Chang KH, et al. Incompatibility of silver nanoparticles with lactate dehydrogenase leakage assay for cellular viability test is attributed to protein binding and reactive oxygen species generation. Toxicol Lett. 2014;225:422–32.
Neun BW, Dobrovolskaia MA. Detection and quantitative evaluation of endotoxin contamination in nanoparticle formulations by LAL-based assays. Methods Mol Biol. 2011;697:121–30.
Goncalves DM, Girard D. Zinc oxide nanoparticles delay human neutrophil apoptosis by a de novo protein synthesis-dependent and reactive oxygen species-independent mechanism. Toxicol In Vitro. 2014;28:926–31.
Ledall J, Fruchon S, Garzoni M, Pavan GM, Caminade AM, Turrin CO, et al. Interaction studies reveal specific recognition of an anti-inflammatory polyphosphorhydrazone dendrimer by human monocytes. Nanoscale. 2015;7:17672–84.
Qi R, Majoros I, Misra AC, Koch AE, Campbell P, Marotte H, et al. Folate receptor-targeted dendrimer-methotrexate conjugate for inflammatory arthritis. J Biomed Nanotechnol. 2015;11:1431–41.
Fruchon S, Mouriot S, Thiollier T, Grandin C, Caminade AM, Turrin CO, et al. Repeated intravenous injections in non-human primates demonstrate preclinical safety of an anti-inflammatory phosphorus-based dendrimer. Nanotoxicology. 2015;9:433–41.
Fruchon S, Caminade AM, Abadie C, Davignon JL, Combette JM, Turrin CO, et al. An azabisphosphonate-capped poly(phosphorhydrazone) dendrimer for the treatment of endotoxin-induced uveitis. Molecules. 2013;18:9305–16.
Neibert K, Gosein V, Sharma A, Khan M, Whitehead MA, Maysinger D, et al. “Click” dendrimers as anti-inflammatory agents: with insights into their binding from molecular modeling studies. Mol Pharm. 2013;10:2502–8.
Bosch X. Dendrimers to treat rheumatoid arthritis. ACS Nano. 2011;5:6779–85.
Hayder M, Fruchon S, Fournie JJ, Poupot M, Poupot R. Anti-inflammatory properties of dendrimers per se. Sci World J. 2011;11:1367–82.
Blattes E, Vercellone A, Eutamene H, Turrin CO, Theodorou V, Majoral JP, et al. Mannodendrimers prevent acute lung inflammation by inhibiting neutrophil recruitment. Proc Natl Acad Sci USA. 2013;110:8795–800.
Liu X, Hao W, Lok CN, Wang YC, Zhang R, Wong KK. Dendrimer encapsulation enhances anti-inflammatory efficacy of silver nanoparticles. J Pediatr Surg. 2014;49:1846–51.
Tang Y, Han Y, Liu L, Shen W, Zhang H, Wang Y, et al. Protective effects and mechanisms of G5 PAMAM dendrimers against acute pancreatitis induced by caerulein in mice. Biomacromolecules. 2015;16:174–82.
Iezzi R, Guru BR, Glybina IV, Mishra MK, Kennedy A, Kannan RM. Dendrimer-based targeted intravitreal therapy for sustained attenuation of neuroinflammation in retinal degeneration. Biomaterials. 2012;33:979–88.
Chauhan AS, Diwan PV, Jain NK, Tomalia DA. Unexpected in vivo anti-inflammatory activity observed for simple, surface functionalized poly(amidoamine) dendrimers. Biomacromolecules. 2009;10:1195–202.
Wang B, Navath RS, Romero R, Kannan S, Kannan R. Anti-inflammatory and anti-oxidant activity of anionic dendrimer-N-acetyl cysteine conjugates in activated microglial cells. Int J Pharm. 2009;377:159–68.
Naha PC, Davoren M, Lyng FM, Byrne HJ. Reactive oxygen species (ROS) induced cytokine production and cytotoxicity of PAMAM dendrimers in J774A.1 cells. Toxicol Appl Pharmacol. 2010;246:91–9.
Neves SA, Dias-Baruff M, Freitas AL, Roque-Barreira MC. Neutrophil migration induced in vivo and in vitro by marine algal lectins. Inflamm Res Off J Eur Histamine Research Soc [et al]. 2001;50:486–90.
Pelletier M, Roberge CJ, Gauthier M, Vandal K, Tessier PA, Girard D. Activation of human neutrophils in vitro and dieldrin-induced neutrophilic inflammation in vivo. J Leukoc Biol. 2001;70:367–73.
Tessier PA, Naccache PH, Clark-Lewis I, Gladue RP, Neote KS, McColl SR. Chemokine networks in vivo: involvement of C-X-C and C-C chemokines in neutrophil extravasation in vivo in response to TNF-alpha. J Immunol. 1997;159:3595–602.
Mukherjee SP, Byrne HJ. Polyamidoamine dendrimer nanoparticle cytotoxicity, oxidative stress, caspase activation and inflammatory response: experimental observation and numerical simulation. Nanomedicine. 2013;9:202–11.
Acknowledgments
The study was supported by grants from the Institut de recherche Robert-Sauvé en santé et en sécurité du travail (IRSST).
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: John Di Battista.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Durocher, I., Girard, D. In vivo proinflammatory activity of generations 0–3 (G0–G3) polyamidoamine (PAMAM) nanoparticles. Inflamm. Res. 65, 745–755 (2016). https://doi.org/10.1007/s00011-016-0959-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-016-0959-5