Abstract
A puzzling aspect of India's nutrition story is that deficiencies in calorie intake and anthropometric health outcomes across states are not significantly correlated. One potential explanation is inaccurate accounting of the calorie needs of people living in different states of India. There are significant variations in the disease environments, health infrastructure, and mechanization of economies across states which necessitate different levels of calorie consumption. Using consumption survey data collected by the National Sample Survey Office in 2011–2012, and utilizing multilevel models, we show that these factors are important determinants of calorie intakes across states. Then we calculate state-adjusted calorie norm for Indian states and use them to recalibrate their prevalence of undernourishment (PoU). In addition, we show that the correlations between calorie intakes, determined by the state-adjusted calorie norms and anthropometric health outcomes, are strong and significant. Our findings suggest that for a diverse country like India, a uniform national calorie intake norm is inappropriate, leading to inaccurate estimates of calorie intake deficiencies across states.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
1 Introduction
India's nutrition intake faces several paradoxical empirical phenomena. First, there is a consistent temporal decline in per capita calorie intake in India while the per capita individual income has been increasing. A significant amount of academic effort has been devoted to rationalizing it (e.g. Deaton & Dreze, 2009; Gaiha et al., 2013; Desai & Thorat, 2013; Eli & Li, 2013; Basole & Basu, 2015, Duh & Spears, 2017; Siddiqui et al., 2019). Second, calorie intake varies significantly across Indian states and is in a counterintuitive direction: the states with better health and nutritional outcomes have lower per capita calorie intakes, while the states with poor health and nutritional outcomes have higher per capita calorie intakes. Third, the states with lower prevalence of nutritional deficiencies have higher prevalence of calorie deficiency.
Thus, the input measures of nutrition (i.e. calorie intake) and nutritional outcomes for Indian states are not strongly correlated (Meenakshi, 2012; Meenakshi & Viswanathan, 2017). While it is understood that caloric intake is not the sole factor behind the anthropometric indicators of the nutritional outcomes, very weak positive correlations between them pose a challenging phenomenon for researchers. Further, if sufficiency in calorie intake is indeed relevant for determining nutritional outcome, as many would agree, then there is a problem in the way calorie deficiency is being measured in India. In this study, we focus on this measurement problem.
Developing an appropriate measurement of calorie deficiency that is responsive to the anthropometric outcomes of the population is important for a variety of reasons, including for a better understanding of the nutritional challenges that we face in India. In addition, it has implication for global reporting on nutrition and health. Prevalence of Undernutrition (PoU), or calorie intake deficiency, is one of the key indicators that the Food and Agriculture Organization (FAO) of the United Nations reports in its flagship publication, The State of Food Security and Nutrition in the World (SOFI). PoU is also used in Global Hunger Index with one-third of the weight assigned to it. Also, it is one of the indicators for sustainable development goals (SDG 2.1.1), relating to achieving the goal of zero hunger (SDG2). India accounted for 27.2% of the world population with calorie deficiency in 2018–20 (SOFI, 2021). As a result, the global estimate of PoU is expected to be highly sensitive to India’s level of PoU. Therefore, it is important that PoU in India is estimated appropriately.
The puzzling aspect of Indian nutrition story is that states such as Kerala and Tamil Nadu, that are among the better performing Indian states in terms of health and economic outcomes, have higher PoU compared to states such as Bihar and Uttar Pradesh that are among the worst performing states of India. In 2011–12, the per capita daily calorie intakes in Bihar and Uttar Pradesh were 2057 and 2116 Kcals, respectively. The corresponding rates in Tamil Nadu and Kerala were 1925 and 1974 Kcals, respectively (NSSO 2014). This is contrary to the conventional wisdom that, by standard of nationally determined minimum dietary energy requirement (MDER), the states with lower per capita calorie intakes should have higher prevalence of PoU and they should have increased over time given that the per capita calorie intake has been declining. These complex features of calorie intake in India have been described as the Indian calorie consumption ‘puzzle’ (Deaton & Dreze, 2009).
1.1 Potential Explanations
A growing body of literature suggests that the environmental or contextual factors can partly explain the spatial and temporal variations in caloric intakes in India. Such factors may include differences in the epidemiological environment, health infrastructure, and mechanization of state economies. For instance, people living in less healthy environment generally consume more calories even if they are poor (Duh & Spears, 2017; Siddiqui et al., 2019).
Approximately 10% of the total variation in the per capita calorie intake across Indian states can be attributed to the interstate variations in disease environment and health infrastructure (Siddiqui et al., 2019). In other words, people residing in the states with better health infrastructure and epidemiological environment have lower calorie intakes, which is consistent with the biomedical literature that suggest that people living in infectious environments may suffer from intestinal health, necessitating higher calories for a given level of effective calorie need (Duh & Spears, 2017). For example, people living in infectious environment likely suffer more from a sub-clinical (undetected) medical condition known as Environmental Enteric Dysfunction (EED), where villi or tentacles of small intestine responsible for absorbing nutrition from food are damaged, resulting in reduced absorption efficiency. Interestingly, EED is also responsible for stunting among young children (Budge et al., 2019).
Therefore, calorie needs of population may vary according to their epidemiological environments. Indian states, especially since 1990s, have witnessed divergent economic and health outcomes (Pingali & Aiyar, 2018). Therefore, it is plausible that they also differ significantly in their epidemiological environments. If this is the case, it will be contrary to the uniform MDER prescribed by Indian Council of Medical Research (ICMR). That is, the uniform calorie norm currently in practice in India does not account for the regional variation in calorie needs and requirements.
Another factor that may explain the regional variation in calorie intake is the variation in mechanization of state economies. Studies have shown that one-third of the decline in the calorie intake in India can be attributed to the reduced physical activity and mechanization of work environment (Eli & Li, 2013, 2021). While this finding is temporal, given the stark variation in economic growth rates across Indian states, variation in mechanization of state economies cannot be ruled out.
In fact, regional variation in various dimensions of development in India is a less studied area. Since the introduction of economic liberalization policy in 1990s, the state economies have diverged widely in terms of economic growth and per capita income (Cherodian & Thrilwall, 2015; Ahluwalia, 2000; Baddeley et al., 2006; Sanga & Shaban, 2017). Therefore, it is reasonable to assume that Indian states have also diverged in their contextual factors (e.g. epidemiological environment, health infrastructure, and mechanization), which also determine calorie intakes.
The remainder of this study is organized as follows. In Sect. 2, we present an empirical strategy to identify the importance of contextual factors in determining per capita calorie intakes across Indian states. We also describe a methodology for recalibrating the national-level MDER to impute state-specific MDER, accounting for the calorie intake that can be attributed to the contextual factors. In Sect. 3, we discuss our results and their implications. Concluding remarks are provided in Sect. 4.
2 Empirical Strategy
Our objective here is to address nutrition ‘puzzle’ of the prima facie lack of correlation between deficiencies in nutritional intake and health outcomes in Indian states. Meenakshi and Viswanathan (2017) and Meenakshi (2012) find that PoU or the deficiencies in nutritional (caloric) intake have no relationship with the anthropometric measures of health such as prevalence of wasting and stunting among children under 5 years, anaemia rates among women of reproductive age, and prevalence of adult undernutrition (i.e. adults with g BMI < 18.5).
2.1 Relationship Between Deficiencies in Nutritional Intake and Health Outcomes
We re-examine the findings of Meenakshi and Viswanathan (2017) to re-establish the prima facie lack of correlation between the deficiencies in nutritional intake and outcomes based on the uniform calorie norm-based measure of PoU, as is the practice of FAO and Indian agencies. National Institute of Nutrition operating under the umbrella of ICMR prescribes MDER for individuals based on their age, sex, and activity status roughly after every 10-year period (ICMR-NIN, 2009, 2020). Irrespective of the state of residence, the prescription is uniformly applicable to all individuals in India. Viswanathan and Meenakshi (2006) propose a method that permits conversion of the individual-level MDER to household level, using age and sex of the household members and the activity status of the household (also see Chand & Jumrani, 2013). The method can be expressed as follows:
Note that MDER of an individual in a household depends on age and sex and activity status of the household. All individuals in a household are assumed to have same activity status, according to the principal economic activity of the household. This assumption is mainly due to lack of data on individual-level activity status.
Using Eq. 1, we calculate each household’s aggregate MDER (\({MDER}_{h}\)) and compare it with the actual calorie consumption of the household to check whether the household is deficient in calorie consumption. For this, we utilize data from Consumption Expenditure Survey (CES), conducted by National Sample Survey Office (NSSO) during 2011–12. The CES data is nationally representative and it provides information on quantity and expenditure on approximately 450 items. Given the calorie, fat, and protein contents of the food items and their quantities consumed, a household’s total calorie, fat, or protein intake can be estimated.
Then we examine if PoU measured using \({MDER}_{h}\) is correlated with the anthropometric outcomes. For this purpose, we use district-level aggregation to ensure a reasonable sample size. We use micro-data from the National Family Health Survey 2015–16 to compute the anthropometric outcomes, which is the closest available survey to 2011–12 CES data. We note that this analysis is based on the uniform national MDER norm and thus we are yet to account for the regional differences in MDER that can occur due to the regional differences in households’ contextual environments. This is our next task.
2.2 The Roles of Contextual Factors
We examine the potential independent roles of contextual factors in determining the calorie intake across Indian states. Our goal is to estimate the variation in per capita calorie intakes across Indian states that can be attributed to the prevailing state-level contextual factors. Thus, in addition to household socio-economic and demographic determinants of calorie intake, we account for factors at neighbourhood (meso) and state (macro) level. For example, households from a particular village may have common food consumption practices that affect their calorie intake. Similarly, households from a particular state may be sharing some common characteristics that affect their calorie intakes.
To account for such influences, a multilevel model is more appropriate, which allows for exploring the independent but unobserved effects of neighbourhood (meso)- and state (macro)-level factors on calorie intakes. Also, a multilevel model allows for additional random components based on assumption of spatial clustering of observations at different levels, expressed below:
\({C}_{hjk}\) is per capita per day calorie intake of household \(h\) in village \(j\) in state \(k\), \({\alpha }_{0}\) is the India-level intercept term, \(X\) s are socio-economic and demographic factors that can affect calorie intake of households, \(\beta\) s are their corresponding effects, and \({\varepsilon }_{hjk}\) is household-specific idiosyncratic error term. The model in Eq. 2 differs from the standard regression model because of \({\alpha }_{k}\) and \({\gamma }_{jk}\). \({\alpha }_{k}\) is the random intercept term that captures intercept deviation of a particular state from the national-level intercept (\({\alpha }_{0}\)). Therefore, the intercept for state \(k\) is \({\alpha }_{0}+{\alpha }_{k}\).
While we have not discussed any issue concerning village-level calorie intake pattern, it is important to account for potential village-level clustering of the households. \({\gamma }_{jk}\) is an additional random intercept term that accounts for intercept variation by village \(j\) situated in state \(k\). Thus, the intercept for village \(j\) is \({\alpha }_{0}+{\alpha }_{k}\)+\({\gamma }_{jk}\). The estimate of variances associated with the contextual random intercept terms (\({\alpha }_{k}\) and \({\gamma }_{jk}\)), expressed as share of the total variance in calorie intake, will indicate their relative importance.
Further, another benefit of using a multilevel model is that we can introduce independent variables at meso- and macro-levels. After estimating Eq. 2 and the variances of the random components, we also estimate the following specification:
Equation 3 is essentially same as Eq. 2 except for additional independent variables operating at state level (\(S)\). We note that \(S\) variables are invariant for all households from a particular state. In other words, the values of \(S\) change for states and not for households within a state.
We are interested in the values of variance of state-level random component, i.e. \(Var({\alpha }_{k}\)) in Eqs. 2 and 3 to examine the roles of \(S\) variables in determining the calorie intakes. If \(S\) variables are successful in significantly reducing \(Var({\alpha }_{k}\)) from Eqs. 2 to 3, we can establish that \(S\) variables are indeed the contextual factors that also determine calorie intake of households. Since \(S\) variables are above and beyond the individual household influences, they are exogenous to households and are affecting their calorie intakes. Therefore, presence or absence of these environmental factors will necessitate households to consume higher or lower calorie.
To estimate Eqs. 2 and 3, we utilize data on household- and state-level characteristics, which are below.
Household characteristics: We use monthly per capita consumption expenditure (MPCE) as a measure of the economic status of a household. In the absence of income or asset information in CES data, MPCE is the best available measure of a household’s economic status. It is well known that economic status measures are often skewed in distribution. As a result, we apply a compression of the order of 0.4 (i.e. \({\mathrm{MPCE}}^{0.4}\)) and use it instead of MPCE. Further, given a non-linear relationship between economic status and calorie intake, we include a square term for \({\mathrm{MPCE}}^{0.4}\). We use mean years of schooling of adults in a household as proxy of its educational status. Physical nature of occupation of a household may be an important determinant in its calorie intake. Households with occupations demanding physical exertion are expected to have higher calorie intake. Therefore, we account for physical nature of occupation, which is captured by a binary variable that takes the value 1 if the household’s major source of income is a physically demanding occupation, otherwise it takes the value 0. Information on physical activity status of a household is derived from the household’s principal occupation reported in the form of National Classification of Occupation (NCO-2004) category codes.
Among demographic characteristics of a household, we use household size, and household head’s gender and age. We also control for socio-religious status of a household. For Hindus, we use caste categories such as SC, ST, and other-Hindus. For Muslims, Sikhs, and Christians, we include separate dummy variables. According to the existing literature, household size is inversely related to calorie intake. Household head’s age is expected to be positively related to calorie intake. Further, a positive association between calorie intakes and female-headed households has been documented. We also account for two additional factors that may have direct positive effects on calorie intakes (i.e. possession of cultivable land and access to PDS).
Contextual factors: To capture environmental determinants of calorie intake, we use state-level rural/urban-specific prevalence rate of stomach problems, malaria, skin disease, and fever due to a disease other than malaria experienced within 365 days as proxy measures for an infectious environment. These variables have been calculated using micro-data from the ‘Drinking Water, Sanitation, Hygiene and Housing Condition’ survey, conducted by NSSO in 2012. We have also account for health infrastructure and mechanization of state economies. However, the latter are expected to be highly correlated with each other. As a result, including them separately in Eq. 3 may produce imprecise estimates. Thus, we use state-level MPCE, calculated separately for rural and urban areas, as the composite index for health infrastructure and mechanization of a state economy.
2.3 Adjustment of the MDER
We adjust the MDER to account for the variation in the contextual environments of the states, using the following procedure:
where \(\overline{{S }_{1}}\) is rural (or urban) India-level mean prevalence rate of infections; \(\overline{{S }_{2}}\) is rural (or urban) mean MPCE of India, representing national-level mean of contextual or macro-environment variables; \({S}_{1k}\) and \({S}_{2k}\). \(HHSize\) is household size. Multiplication of \(\left[{\pi }_{1}\left({S}_{1k}-\overline{{S }_{1}}\right)+{\pi }_{2}\left({S}_{2k}-\overline{{S }_{2}}\right)\right]\) with household size is required because regression co-efficient is derived using per capita calorie intake as dependent variable. \({StateAdjustedMDER}_{h}\) computed in this manner is likely to be higher than the \({MDER}_{h}\) for households in the states with worse than average levels of S and vice versa. Accordingly, PoU measures will also be impacted. States where \({StateAdjustedMDER}_{h}\) is greater than the \({MDER}_{h}\), PoU will increase, while the opposite is expected for the states where \({StateAdjustedMDER}_{h}\) is less than \({MDER}_{h}\).
Finally, we examine if PoU measured using \({StateAdjustedMDER}_{h}\) is correlated with the anthropometric outcomes. For this also, we use district-level data.
3 Results
3.1 Correlation Between the Conventional Measure of PoU and Anthropometric Outcomes
We first re-establish that the conventional measure of PoU is not strongly correlated with the anthropometric outcomes, such as the prevalence of stunting, wasting, under-5 mortality rate, and the prevalence of adult underweight (BMI < 18.5), shown in Fig. 1. While the measures of the anthropometric outcomes are objective and do not suffer from serious measurement errors, the measurement of PoU involves assumptions about caloric requirements of the relevant population which may often be subjective. The choice of a benchmark or MDER is critical to the measurement of PoU, which differs across countries. Given significant variations in socio-economic and demographic characteristics across Indian states, as discussed earlier, it is likely that the uniform national norm for MDER is mistaken.
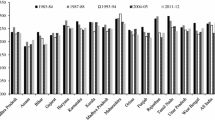
Figures 2 and 3 clearly show that Kerala and Tamil Nadu, despite having higher levels of economic affluence and superior anthropometric outcomes, have lower per capita calorie intake compared to the poorer states of India, Bihar and Odisha. This result lends credence to the idea that the lower per capita calorie intake is perhaps driven more by the lower calorie needs in these states rather than the economic circumstances that could constrain household food expenditure.
This is further corroborated by significant difference in the calorie consumed in different regions. Figure 4 shows that the share of fat and protein (non-carbohydrate) in total calorie intake is higher, on average, in the states that have lower calorie intake, and this applies to economic deciles as well. Moreover, the states with lower calorie intakes also have higher expenditure on per unit calorie for every economic class in the rural areas. These results provide strong support for the argument that lower calorie intake in Kerala and Tamil Nadu is because of lower needs rather than economic constraints.
Next, using multivariate statistical analysis, we further reaffirm the calorie consumption ‘Puzzle’ in India. Also, we establish the extent to which calorie consumption can be attributed to macro-environmental factors (e.g. disease environment, health infrastructure and level of mechanization in the economy).
3.2 Contribution of Macro-environmental Factors
We estimate and examine effects of macro-environment factors on calorie intake, separately for the rural and urban India. We estimate two specifications for rural India and two specifications for urban India. In the first specification, we do not account for the variation across Indian states in their macro-environments, but we do so in the second specification.
Table 1 provides component-wise variances and their relative shares in the total variance of the calorie intake. Importance of the contextual or macro-environmental factors can be inferred from the fact that the variance of random intercept for states is approximately 8.3% of the total variance of per capita per day calorie intake in rural India (Model 1.1). Even in urban India, the share of state random intercept variance is approximately 5.13% (Model 2.1). Interestingly, with the inclusion of macro-environment factors (i.e. infectiousness of environment and state average MPCE), the variance of state-level intercept reduces to less than 1% without having any major effect on PSU and individual-level random components’ variance share (Models 1.2 and 2.2). This implies that our macro-environment variables capture the variance at state level.
Table 2 presents the results from the estimation of Eqs. 2 and 3 in Sect. 2. We present the results separately for the rural and urban India. The results are broadly consistent across two specifications and rural/urban India. As expected, the economic status of a household, captured by MPCE, has a strong non-linear positive effect on its calorie intake, but with a decreasing marginal effect. Note that MPCE has been compressed to the degree of 0.4 to treat the skewness in its distribution. Interestingly, when MPCE is aggregated at state level, it has the opposite effect. Recall that we use state average MPCE as the proxy for state health infrastructure and mechanization level of state economy. While other socio-economic factors such as physical nature of occupation of the households necessitate higher calorie consumption, the higher levels of education of households are negatively associated with their calorie intakes.
Among demographic factors, household size has an inverse relationship with calorie intake, which is consistent with the previous findings (Deaton & Paxson, 1998). Female-headed households have significantly higher calories than male-headed households. Age of the head of household has a positive and significant effect on calorie intake. Among the socio-religious groups, we find that Scheduled Tribes (STs) and Scheduled Castes (SCs), Sikhs, and Muslims have significantly higher calorie intakes than the upper-caste Hindus. However, the later results are limited only to the rural areas.
We also control for other two important factors that can have direct effects on calorie intakes (e.g. access to ration card for accessing food from public distribution system and availability of cultivable land). As expected, both have positive and significant effects on calorie intake. Naturally, we do not control for the availability of cultivable land for the urban households.
While the individual economic status has a strong positive effect on calorie intake, the state economic status has a negative effect on calorie intake. This is primarily because state-level improvement in economic status is strongly correlated with the improvements in health-related infrastructure and mechanization of state economy. Infectiousness of environment, our key contextual variable, measured as the prevalence rate of infectious diseases, in a state has a strong positive effect on calorie intake. This suggests that state-level disease prevalence is an important predictor of a household’s calorie intake.
In sum, from Table 2, the macro-level context of the calorie intake in India is attributable to the macro-level environmental context.
This is key to our argument that a large proportion of regional variation in calorie intake is driven by differences in disease environment and level of health infrastructure and mechanization of the regional economy. Thus, the use of a nationally uniform MDER to assess the prevalence or intensity of calorie deficiency across states is bound to give a distorted picture of the reality.
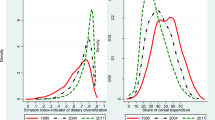
3.3 Adjusted MDER
An advantage of multilevel models is that they allow us to estimate different intercepts corresponding to different levels of factors. To our analysis, macro-level intercept deviations are of particular interest because they show the relative position of each state after accounting for household-level covariates of calorie intake (see Fig. 5, i.e. predicted random intercepts for states from Models 1.1. and 2.1). That is, a state’s higher negative (positive) intercept deviation from the overall (national) intercept indicates the prevalent macro-environmental context in state, which necessitates lower (higher) calorie intake. Also, as discussed in Sect. 3.2, we examine the extent of compression in bandwidth of intercept deviations after we adjust for macro-environment factors operating at state level (i.e. infectiousness and state of health infrastructure and mechanization) in addition to household covariates from Models 1.2. and 2.2.

Note ANP = Andhra Pradesh, ASS = Assam, BIH = Bihar, CHT = Chhattisgarh, GUJ = Gujarat, HAR = Haryana, JHK = Jharkhand, KAR = Karnataka, KER = Kerala, MAP = Madhya Pradesh, MHR = Maharashtra, ORS = Orissa, PUN = Punjab, RAJ = Rajasthan, TAN = Tamil Nadu, UTP = Uttar Pradesh, WEB = West Bengal. Source Derived from the in Table 2
Random intercept deviation of states from national-level intercept.
Figure 5 shows the random intercept deviations of each state from the national-level intercept, both for rural and urban. In both rural and urban areas of Kerala and Tamil Nadu, we find that their macro-environmental context induces households to consume fewer calories than the national average. On other hand, the situation is the exact opposite in Bihar, Uttar Pradesh, and Orissa. For instance, in rural (urban) Kerala, an average household consumes 388 (204) fewer calories than the national average. In contrast, in rural (urban) Bihar, an average household consumes about 191 (288) more calories than the national average. However, once we adjust for the macro-environment of the states, the deviations become insignificant for many of the states, which are reflected in significant compressions of the bandwidths of the intercept deviations of states. This implies that the macro-environment of a state has a significant effect on household calorie intake. Therefore, the uniform MDER needs to be adjusted for a more accurate estimate of prevalence or intensity of calorie deficiency.
Using the formula in Eq. 4 in Sect. 2.3, we arrive at the state-adjusted MDER. We calculate PoU using both the uniform national MDER and our state-adjusted MDER to examine the change in rank order of states. We rank the states in the increasing order of PoU levels, assigning the first rank to the state with the lowest PoU.
In Table 3, we present the result. Accordingly, Kerala, Tamil Nadu, Karnataka, Gujarat, and Telangana have the highest level PoU if we consider the uniform national MDER. However, their ranks improve if we use our state-adjusted MDER. In contrast, ranks of Bihar, Uttar Pradesh, Jharkhand, and Chhattisgarh become worse when we move from the uniform MDER to the state-adjusted MDER. Thus, the measure of PoU aligns better with the realities of everyday life across Indian states.
To test the correlation of PoU, based on the two alternative MDERs, with various anthropometric outcomes, we estimate district-level PoU using the state-adjusted MDER. Then we combine this data with the district-level data on the anthropometric or nutritional outcomes. Figure 6 presents scatter plot and Pearson’s correlation coefficients between alternative PoU measures and respective prevalence of deficiencies in anthropometric measures. Correlations between the uniform national MDER-based PoU with the anthropometric health measures are statistically insignificant. In contrast, the corresponding correlations are statistically significant for the state-adjusted MDER except for prevalence of wasting (body mass faltering). Wasting of children has been a blind spot in India’s nutrition story, as we have high prevalence of wasting even in the states that perform better in terms of stunting (height faltering). India has consistently remained an outlier nation with regard to wasting, performing worse than most Central African countries (Siddiqui et al., 2021).
Given our analysis and results, it is clear that the uniform calorie norm or MDER standard in India needs to be corrected for accurately estimating PoU.
4 Conclusions
In this study, we attempt to provide a better measurement of PoU by proposing and using a state-adjusted measure of MDER. We start by highlighting the Indian calorie consumption ‘puzzle’, which has three distinct aspects. First, while per capita individual income has been increasing in India, the per capita calorie intake has been declining over time. Second, the states with better health and nutritional outcomes have lower per capita calorie intakes, and vice versa. Third, the states with lower nutritional outcome deficiencies have higher calorie deficiencies.
In recent years, studies have attempted to explain this puzzle. Among the alternative explanations, the roles of spatial variations in the environmental or contextual factors appear to be compelling. For instance, it has been argued that people living in less healthy environment consume more calories even if they are poor. More specifically, it has been documented that about 8–10% of the total variation in the per capita calorie intake across Indian states can be explained by the interstate variations in disease environment and health infrastructure. Another explanation for the Indian calorie consumption puzzle is the role of mechanization of state economies. Studies have shown that one-third of the decline in the calorie intake in India can be attributed to the reduced physical activity and mechanization of work environment. This means that calorie needs of people may vary according to the epidemiological environments in which they live, which will be contrary to the uniform MDER prescribed by ICMR.
In this study, we revisit the Indian calorie consumption puzzle, and conduct the following analyses. First, we present and utilize an empirical strategy to examine the roles of the contextual factors in determining per capita calorie intakes across states. Second, we describe and utilize a methodology to recalibrate the uniform national MDER to impute state-specific MDER, by accounting for the calorie intake that can be attributed to the contextual factors.
Our important findings are as follows. First, we confirm the Indian calorie consumption puzzle. Second, we replicate the finding in the literature that the measure of PoU using the uniform MDER is not significantly correlated with the anthropometric health outcomes. Third, we show that the variations in the contextual macro-environment significantly explain the variation in calorie intakes across states. Fourth, we show that the state-adjusted MDER is significantly and strongly correlated with the anthropometric health outcomes.
There are several implications of our findings. First, the uniform national MDER needs to be revised to reflect state-level variations of the contextual macro-environments (e.g. disease environment, health infrastructure, and mechanization of economies). Second, the Indian calorie consumption puzzle is not really a puzzle, because it can be significantly explained by regional variations in the contextual environments for calorie consumption needs. Finally, to estimate a more accurate estimate of PoU in India and the world, we recommend that state-adjusted MDER is used by Indian agencies and FAO.
References
Ahluwalia, M. S. (2000). Economic performance of states in post-reforms period. Economic and Political Weekly, 35(19), 1637–1648.
Baddeley, M., McNay, K., & Cassen, R. (2006). Divergence in India: Income differentials at the state level, 1970–97. The Journal of Development Studies, 42(6), 1000–1022.
Basole, A., & Basu, D. (2015). Fuelling calorie intake decline: Household-level evidence from rural India. World Development, 68, 82–95. https://doi.org/10.1016/j.worlddev.2014.11.020
Budge, S., Parker, A. H., Hutchings, P. T., & Garbutt, C. (2019). Environmental enteric dysfunction and child stunting. Nutrition Reviews, 77(4), 240–253.
Chand, R., & Jumrani, J. (2013). Food security and undernutrition in India: Assessment of alternative norms and the income effect. Indian Journal of Agricultural Economics, 68(1), 39–53.
Cherodian, R., & Thirlwall, A. P. (2015). Regional disparities in per capita income in India: Convergence or divergence? Journal of Post Keynesian Economics, 37(3), 384–407.
Deaton, A., & Dreze, J. (2009). Food and nutrition in India: Facts and interpretations. Economic and Political Weekly, 44(7), 42–65.
Deaton, A., & Paxson, C. (1998). Economies of scale, household size and the demand for food. The Journal of Political Economy, 106(5), 897–930. https://doi.org/10.1086/250035
Desai, S., & Thorat, A. (2013). Beyond the great Indian calorie nutrition debate. Economic and Political Weekly, 38(45–46), 18–22.
Duh, J., & Spears, D. (2017). Health and hunger: Disease, energy needs, and the Indian calorie consumption puzzle. The Economic Journal, 127(606), 2378–2409.
Eli, S., & Li, N. (2013). Can caloric needs explain three food consumption puzzle? Evidence from India. https://www.dartmouth.edu/neudc2012/docs/paper_263.pdf.
Eli, S., & Li, N. (2021). Caloric intake and energy expenditures in India. The World Bank Economic Review, 35(4), 1057–1075.
Gaiha, R., Jha, R., & Kulkarni, V. (2013). Demand for nutrients in India: 1993 to 2004. Applied Economics, 45(14), 1869–1886.
ICMR-NIN. (2009). Nutrient requirements and recommended dietary allowances for Indians. ICMR-National Institute of Nutrition.
ICMR-NIN. (2020). Nutrient Requirements for Indians, Recommended Dietary Allowances (RDA) and estimated average requirements. ICMR-National Institute of Nutrition.
Meenakshi, J. V. (2012). Undernutrition. In K. Basu & A. Maertens (Eds.), The New Oxford Companion to Economics in India. Oxford University Press.
Meenakshi, J. V., & Viswanathan, B. (2017). Estimation of calorie norms and measurement of food intakes: Some implications for the magnitudes of the prevalence of undernutrition in India. In Perspectives on Economic Development and Policy in India (pp. 169–189). Springer.
National Sample Survey Office (NSSO). (2014). Nutritional intake in India, 2011–12, NSS 68th round, report no. 560(68/1.0/3). Ministry of Statistics and Programme Implementation, Government of India.
Pingali, P., & Aiyar, A. (2018). Diversity in development: Inter-state differences in the India growth story. World Food Policy, 4(2), 57–77.
Sanga, P., & Shaban, A. (2017). Regional divergence and inequalities in India. Economic & Political Weekly, 52(1), 103.
Siddiqui, M. Z., Biswas, S., & Jose, S. (2021). Alarming hunger in India. Economic & Political Weekly, 56(50), 13–17.
Siddiqui, M. Z., Donato, R., & Jumrani, J. (2019). Looking past the Indian calorie debate: What is happening to nutrition transition in India. The Journal of Development Studies, 55(11), 2440–2459.
SOFI. (2021). The state of food security and nutrition in the world 202: Transforming food systems for food security, improved nutrition and affordable healthy diets for all. Rome, FAO. Food and Agriculture Organisation of United Nations.
Viswanathan, B., & Meenakshi, J. (2006). The changing pattern of undernutrition in India: A comparative analysis across regions (Research Paper no. 2006/118). UNU World Institute for Development Economics Research.
Acknowledgements
This research was financially supported by SPANDAN (System of Promoting Appropriate National Dynamism for Agriculture and Nutrition) housed at Indira Gandhi Institute of Development Research Mumbai (IGIDR). The SPANDAN initiative is supported by Bill and Melinda Gates Foundation.
Professor Manoj Panda, Prof. Brinda Viswanathan, and Prof. Mahadera Dev have commented on the earlier versions of the paper during three presentations that were made at IGIDR. These comments have improved our understanding and draft of the paper significantly.
Authors are also thankful to Ronald Donato and Jaya Jumrani as a significant progress on this line of research was made during a collaborative work on calorie puzzle.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Siddiqui, M.Z., Rahman, T. (2024). In the Pursuit of an Appropriate Calorie Intake Norm for Indian States. In: Dev, S.M., Ganesh-Kumar, A., Pandey, V.L. (eds) Achieving Zero Hunger in India. India Studies in Business and Economics. Springer, Singapore. https://doi.org/10.1007/978-981-99-4413-2_3
Download citation
DOI: https://doi.org/10.1007/978-981-99-4413-2_3
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-4412-5
Online ISBN: 978-981-99-4413-2
eBook Packages: Economics and FinanceEconomics and Finance (R0)