Abstract
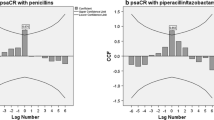
The approximate situation of the spread of antimicrobial-resistant bacteria can be estimated by the use of the cross-resistance rate (CRR). In our previous study, we reported some interesting features of the CRR that the pharmaceutical prescription of antibiotic drugs to patients reflects the asymmetric behavior of the pharmacists. Those behaviors can be represented by asymmetric data of the drugs, and we could gain new insights into that matter by applying the radius-distance model (Okada and Imaizumi in Behaviormetrika 14:81–96, 1987). This model was developed for evaluating the similarity of asymmetric data, and the degree of the similarity can be visualized by a configuration with points and the radii of circles in a multidimensional Euclidean space. We adopted the data of CRR of Pseudomonas aeruginosa as the first attempt to demonstrate the practical utility of this model. As a result, the same strains of antibiotics were distributed closely on the two-dimensional configuration. Even with different groups of antibiotics, the classification was found to be identical to the drugs’ mechanism of action. We clarified from the results of one month of chronological monitoring that the radii of the circles were influenced by a change in the environment, i.e., the hospital relocation. In conclusion, the radius-distance model has the potential for discovering new characteristics or specific features of the data from a new perspective in the fields of medical and pharmaceutical research.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Ahmad, S. I., Malak, H. A., & Abulreesh, H. H. (2021). Environmental antimicrobial resistance and its drivers: A potential threat to public health. Journal of Global Antimicrobial Resistance, 27, 101–111.
Aitken, C., & Jeffries, D. J. (2001). Nosocomial spread of viral disease. Clinical Microbiology Reviews, 14(3), 528–546.
Antimicrobial resistance: no action today, no cure tomorrow, Remarks at a high-level panel on World Health Day 2011, World Health Organization, 7 April 2011. https://www.who.int/director-general/speeches/detail/antimicrobial-resistance-no-action-today-no-cure-tomorrow
Bove, G., Okada, A., & Vicari, D. (2021). Methods for the analysis of asymmetric proximity data. Springer Nature.
Cell wall synthesis inhibitors: Penicillins, OSMOSIS from ELSEVIER. https://www.osmosis.org/learn/Cell_wall_synthesis_inhibitors:_Penicillins
“Cephalosporin” from Wikipedia, the free encyclopedia. https://en.wikipedia.org/wiki/Cephalosporin
Cuttelod, M., Senn, L., & Terletskiy V., et al. (2011). Molecular epidemiology of Pseudomonas aeruginosa in intensive care units over a 10-year period (1998–2007). Clinical Microbiology and Infection, 17(1), 57–62. https://doi.org/10.1111/j.1469-0691.2010.03164.x
Drugs. Com. (2022). Drug Interactions between amikacin and gentamicin, https://www.drugs.com/drug-interactions/amikacin-with-gentamicin-153-0-1168-0.html#:~:text=Using%20gentamicin%20together%20with%20amikacin,or%20have%20preexisting%20kidney%20disease
European Medicines Agency. (2018). Disabling and potentially permanent side effects lead to suspension or restrictions of quinolone and fluoroquinolone antibiotics, EMA 795349. https://www.ema.europa.eu/en/news/disabling-potentially-permanent-side-effects-lead-suspension-restrictions-quinolone-fluoroquinolone#:~:text=These%20serious%20side%20effects%20include,and%20altered%20taste%20and%20smell.
Fazeli, H., Akbari, R., Moghim, S., et al. (2012). Pseudomonas aeruginosa infections in patients, hospital means, and personnel’s specimens. Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences, 17(4), 332–337.
Godijk, N. G., Bootsma, M. C. J., & Bonten, M. J. M. (2022). Transmission routes of antibiotic resistant bacteria: A systematic review. BMC Infectious Diseases, 22, 482. https://doi.org/10.1186/s12879-022-07360-z
Guerrini, V., Rosa, M. D., & Pasquini, S., et al. (2013). New fluoroquinolones active against fluoroquinolones-resistant Mycobacterium tuberculosis strains. Tuberculosis (Edinb), 93(4), 405–411. https://doi.org/10.1016/j.tube.2013.02.017
Hatsuda, Y., Maki, S., Ishimaki, Y., et al. (2019). Development of a new correlation diagram to visualize the trends of antimicrobial cross-resistance. Journal of Biomedical Soft Computing and Human Sciences, 24(1), 39–48.
Hatsuda, Y., Ishizaka, T., Koizumi, N., et al. (2020). Monitoring antimicrobial cross-resistance with cross-resistance rate correlation diagrams: Changes in antibiotic susceptibility of Pseudomonas aeruginosa due to hospital relocation. Journal of Clinical Pharmacy and Therapeutics, 45, 13296. https://doi.org/10.1111/jcpt.13296
Hatsuda, Y., Maki, S., & Ishizaka, T., et al. (2021). Visualization of cross-resistance between antimicrobials by asymmetric multidimensional scaling. Journal of Clinical Pharmacy and Therapeutics, 46, 13564. https://doi.org/10.1111/jcpt.13564
Kapoor, G., Saigal, S., & Elongavan, A. (2017). Action and resistance mechanisms of antibiotics: A guide for clinicians. Journal of Anaesthesiology, Clinical Pharmacology, 33(3), 300–305. https://doi.org/10.4103/joacp.JOACP_349_15, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5672523/
Kovačević, T., Avram, S., & Milaković, D. et al (2016). Therapeutic monitoring of amikacin and gentamicin in critically and noncritically ill patients. Journal of Basic and Clinical Pharmacy, 7(3), 65–69. https://doi.org/10.4103/0976-0105.183260, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4910469/#:~:text=Results%3A,patients%20(P%20%3D%200.457
Moradali, M. F., Ghods S., & Rehm B. H. A. (2017). Pseudomonas aeruginosa lifestyle: a paradigm for adaptation, survival, and persistence. Frontiers in Cellular and Infection Microbiology, 7, 39. https://doi.org/10.3389/fcimb.2017.00039
Mukae, H., Kawanami, T., & Yatera, K., et al. (2014). Efficacy and safety of levofloxacin in patients with bacterial pneumonia evaluated according to the new Clinical Evaluation Methods for New Antimicrobial Agents to Treat Respiratory Infections (Second Version). Journal of Infection and Chemotherapy, 20(7), 417–422. https://doi.org/10.1016/j.jiac.2014.03.009
Nielsen, S. S., Bicout, D. J., & Calistri, P., et al. (2022). Assessment of listing and categorisation of animal diseases within the framework of the Animal Health Law (Regulation (EU) No 2016/429): antimicrobial-resistant Pseudomonas aeruginosa in dogs and cats. EFSA Journal, 20(5), 7310. https://doi.org/10.2903/j.efsa.2022.7310
Lila, G., Mulliqi, G., Raka, L., et al. (2018). Molecular epidemiology of Pseudomonas aeruginosa in university clinical center of Kosovo. Infection and Drug Resistance, 11, 2039–2046.
Okada, A., & Imaizumi, T. (1987). Nonmetric multidimensional scaling of asymmetric proximities. Behaviormetrika, 14(21), 81–96.
Okada, A., & Imaizumi, T. (1994). Method of PC multidimensional scaling configuration (pp. 10–29). Kyoritsu Shuppan Co., Ltd. (in Japanese). ISBN4–320–01472–3.
Okada, A., & Imaizumi, T. (1997). Asymmetric multidimensional scaling of two-mode three-way proximities. Journal of Classification, 14, 195–224.
Okada, A., & Imaizumi, T. (2003). Developing a layout of a supermarket through asymmetric multidimensional scaling and cluster analysis of purchase data between data science and applied data analysis (pp. 587–594). Springer.
Okada, A. (2011). Supekutoru bunnkai niyoru gaikokujinn ni taisuru shinnkinnkann no bunnseki [Analyzing social affinity for foreigners by spectral decomposition: Asymmetric multidimensional scaling of EASS 2008 Data]. GSS Research Series, 11, 119–128. (In Japanese).
Okada, A., & Tsurumi, H. (2012). Asymmetric multidimensional scaling of brand switching among margarine brands. Behaviormetrika, 39, 111–126.
Pham, T. M., Kretzschmar, M., Bertrand, X., & Bootsma, M. (2019). Tracking Pseudomonas aeruginosa transmissions due to environmental contamination after discharge in ICUs using mathematical models. PLoS Computational Biology, 15(8), e1006697. https://doi.org/10.1371/journal
Pham, T. D. M., Ziora, Z. M., & Blaskovich, M. A. T. (2019). Quinolone antibiotics. Medicinal Chemistry Communication, 10, 1719–1739. https://doi.org/10.1039/C9MD00120D, https://pubs.rsc.org/en/content/articlehtml/2019/md/c9md00120d#:~:text=The%20quinolone%20class%20of%20antibiotics,supercoiling%20required%20for%20DNA%20synthesis
Pham, T. M., Büchler, A. C., & Voor in ‘t holt, A. F., et al. (2022). Routes of transmission of VIM-positive Pseudomonas aeruginosa in the adult intensive care unit-analysis of 9 years of surveillance at a university hospital using a mathematical model. Antimicrobial Resistance and Infection Control, 11, 55. https://doi.org/10.1186/s13756-022-01095-x
Poole, K. (2005). Aminoglycoside resistance in Pseudomonas aeruginosa. Antimicrobial Agents and Chemotherapy, 49(2), 479–487. https://doi.org/10.1128/AAC.49.2.479-487.2005, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC547279/
Public Awareness Council for Promotion of Antimicrobial Resistance (AMR) Countermeasures, International Infectious Disease Control Coordination Office, Japan Cabinet, October 18, 2016. (in Japanese). https://www.kantei.go.jp/jp/singi/kokusai_kansen/amr_taisaku/dai1/gijiroku.pdf, https://www.kantei.go.jp/jp/singi/kokusai_kansen/amr_taisaku/dai4/index.html
Queenan, A. M., & Bush, K. (2007). Carbapenemases: the versatile β-Lactamases. Clinical Microbiology Reviews, 20(3), 440–458. https://doi.org/10.1128/CMR.00001-07, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1932750/
Reuter, S., Sigge, A., Wiedeck, H., & Trautmann, M. (2002). Analysis of transmission pathways of Pseudomonas aeruginosa between patients and tap water outlets. Critical Care Medicine, 30 (10), 2222–2228. https://doi.org/10.1097/00003246-200210000-00008
Safeyah, A., Maqbul, M. S., & Safeyah, M. (2018). Role of Pseudomonas aeruginosa in nosocomial infection. International Journal of Health Sciences, 6(1), 211–217.
Schmidt T. M. (Eds.). (2019). Encyclopedia of microbiology (4th ed., pp. 127–139). Elsevier. ISBN 978–0–12–811737–8
Spagnolo, A. M., Sartini, M., & Cristina, M. L. (2021). Pseudomonas aeruginosa in the healthcare facility setting. Reviews in Medical Microbiology, 32, 169–175.
The Society for Bacterial Drug Resistance, Gunma University Graduate School of Medicine, Japan. http://yakutai.dept.med.gunma-u.ac.jp/society/QandA.html
Website of “Shiny from R studio”. https://shiny.rstudio.com
Willmann, M., Bezdan, D., & Zapata, L., et al. (2015). Analysis of a long-term outbreak of XDR Pseudomonas aeruginosa: a molecular epidemiological study. Journal of Antimicrobial Chemotherapy, 70(5), 1322–1330. https://doi.org/10.1093/jac/dku546
Acknowledgements
This research was supported by the research funding of the Institute of Frontier Science and Technology, Okayama University of Science. This paper was proofread in English by Prof. Christopher Carman of the University of Occupational and Environmental Health. Akinori Okada, Prof. Emeritus of the Rikkyo University, gave us advice on an earlier version of this paper. We would like to express our deepest gratitude for their support.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Maki, S. et al. (2023). Chronological Monitoring of the Cross-Resistance Rate of Pseudomonas Aeruginosa Classified by the Radius-Distance Model. In: Okada, A., Shigemasu, K., Yoshino, R., Yokoyama, S. (eds) Facets of Behaviormetrics. Behaviormetrics: Quantitative Approaches to Human Behavior, vol 4. Springer, Singapore. https://doi.org/10.1007/978-981-99-2240-6_11
Download citation
DOI: https://doi.org/10.1007/978-981-99-2240-6_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-2239-0
Online ISBN: 978-981-99-2240-6
eBook Packages: Mathematics and StatisticsMathematics and Statistics (R0)