Abstract
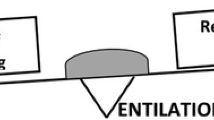
Neuromuscular disease (NMD) is a diverse group of hereditary or acquired conditions involving the anterior horn cells, nerves, neuromuscular junction or muscles. Sleep-disordered breathing (SDB) is common in children and adults with NMD with an estimated prevalence exceeding 40%. Characteristics of NMD like progressive neuromuscular weakness of respiratory and diaphragmatic muscles, anatomic or neurologic propensity to upper airway obstruction during sleep, and/or cardiomyopathy contribute to the development of SDB. Prevalence and pattern of SDB vary with different types of NMD, depending on the features of the disease and the tempo of progression to respiratory muscle impairment. Importantly, sleep-disordered breathing (SDB) and nocturnal hypoventilation are often the first signs of respiratory muscle weakness in patients with NMD. The imbalance between respiratory capacity and respiratory loads usually first manifests during sleep, if not acutely during respiratory decompensation in respiratory infection. In patients with NMD, SDB typically first develops in rapid-eye-movement sleep when muscle atonia occurs, followed by continuous nocturnal hypoventilation through the night and eventually by progression into daytime respiratory failure. Untreated SDB and hypoventilation in NMD carries high respiratory morbidity and mortality. Therefore, screening for SDB and nocturnal hypoventilation is a vital part of long-term management of NMD and to detect patients at risk for respiratory failure. Anticipatory approach with regular assessment of symptoms, pulmonary function and sleep in children affected by NMD can aid early diagnosis and management of SDB. Timely provision of respiratory care and non-invasive ventilation are essential components of a multi-disciplinary care to improve quality of life and survival of patients with NMD.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Deenen JCW, Horlings CGC, Verschuuren JJGM, Verbeek ALM, van Engelen BGM. The epidemiology of neuromuscular disorders: a comprehensive overview of the literature. J Neuromuscul Dis. 2015;2(1):73–85.
Chan SHS, Lo IFM, Cherk SWW, Cheng WW, Fung ELW, Yeung WL, et al. Prevalence and characteristics of Chinese patients with Duchenne and Becker muscular dystrophy. Child Neurol Open [Internet]. 2015 May 26 [cited 2021 Feb 22];2(2). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5417024/
Woodcock IR, Fraser L, Norman P, Pysden K, Manning S, Childs AM. The prevalence of neuromuscular disease in the paediatric population in Yorkshire, UK; variation by ethnicity and deprivation status. Dev Med Child Neurol. 2016;58(8):877–83.
Theadom A, Rodrigues M, Poke G, O’Grady G, Love D, Hammond-Tooke G, et al. A nationwide, population-based prevalence study of genetic muscle disorders. Neuroepidemiology. 2019;52(3–4):128–35.
Labanowski M, Schmidt-Nowara W, Guilleminault C. Sleep and neuromuscular disease: Frequency of sleep-disordered breathing in a neuromuscular disease clinic population. Neurology. 1996;47(5):1173–80.
Gozal D. Pulmonary manifestations of neuromuscular disease with special reference to Duchenne muscular dystrophy and spinal muscular atrophy. Pediatr Pulmonol. 2000;29(2):141–50.
Katz SL. Assessment of sleep-disordered breathing in pediatric neuromuscular diseases. Pediatrics. 2009;123(Suppl 4):S222–5.
Aboussouan LS. Sleep-disordered breathing in neuromuscular disease. Am J Respir Crit Care Med. 2015;191(9):979–89.
Gurbani N, Pascoe JE, Katz S, Sawnani H. Sleep disordered breathing: Assessment and therapy in the age of emerging neuromuscular therapies. Pediatr Pulmonol. 2021;56(4):700–9.
LoMauro A, D’Angelo MG, Aliverti A. Sleep disordered breathing in Duchenne muscular dystrophy. Curr Neurol Neurosci Rep. 2017;17(5):44.
Khan Y, Heckmatt JZ. Obstructive apnoeas in Duchenne muscular dystrophy. Thorax. 1994;49(2):157–61.
Suresh S, Wales P, Dakin C, Harris MA, Cooper DGM. Sleep-related breathing disorder in Duchenne muscular dystrophy: disease spectrum in the paediatric population. J Paediatr Child Health. 2005;41(9–10):500–3.
Simonds AK. Chronic hypoventilation and its management. Eur Respir Rev. 2013;22(129):325–32.
Grychtol R, Abel F, Fitzgerald DA. The role of sleep diagnostics and non-invasive ventilation in children with spinal muscular atrophy. Paediatr Respir Rev. 2018;28:18–25.
Panitch HB. Respiratory implications of pediatric neuromuscular disease. Respir Care. 2017;62(6):23.
Young HK, Lowe A, Fitzgerald DA, Seton C, Waters KA, Kenny E, et al. Outcome of noninvasive ventilation in children with neuromuscular disease. Neurology. 2007;68(3):198–201.
Chatwin M, Tan HL, Bush A, Rosenthal M, Simonds AK. Long term non-invasive ventilation in children: impact on survival and transition to adult care. PLoS One. 2015;10(5):e0125839.
Mellies U, Ragette R, Schwake CD, Boehm H, Voit T, Teschler H. Longterm noninvasive ventilation in children and adolescents with neuromuscular disorders. Eur Respir J. 2003;22(4):631–6.
Panitch HB. Respiratory issues in the management of children with neuromuscular disease. Respir Care. 2006;51(8):885–93. discussion 894-895
Aboussouan LS, Mireles-Cabodevila E. Sleep-disordered breathing in neuromuscular disease: diagnostic and therapeutic challenges. Chest. 2017;152(4):880–92.
Tabachnik E, Muller NL, Bryan AC, Levison H. Changes in ventilation and chest wall mechanics during sleep in normal adolescents. J Appl Physiol Respir Environ Exerc Physiol. 1981;51(3):557–64.
Culebras A. Sleep disorders and neuromuscular disease. Semin Neurol. 2005;25(1):33–8.
Birnkrant DJ, Bushby K, Bann CM, Alman BA, Apkon SD, Blackwell A, et al. Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol. 2018;17(4):347–61.
Ragette R, Mellies U, Schwake C, Voit T, Teschler H. Patterns and predictors of sleep disordered breathing in primary myopathies. Thorax. 2002;57(8):724–8.
Dohna-Schwake C, Ragette R, Mellies U, Straub V, Teschler H, Voit T. Respiratory function in congenital muscular dystrophy and limb girdle muscular dystrophy 2I. Neurology. 2004;62(3):513–4.
Hukins CA, Hillman DR. Daytime predictors of sleep hypoventilation in Duchenne muscular dystrophy. Am J Respir Crit Care Med. 2000;161(1):166–70.
Hull J, Aniapravan R, Chan E, Chatwin M, Forton J, Gallagher J, et al. British Thoracic Society guideline for respiratory management of children with neuromuscular weakness. Thorax. 2012;67(Suppl 1):i1–40.
Bianchi C, Baiardi P. Cough peak flows: standard values for children and adolescents. Am J Phys Med Rehabil. 2008;87(6):461–7.
Kotwal N, Shukla PJ, Perez GF. Peak cough flow in children with neuromuscular disorders. Lung. 2020;198(2):371–5.
Fishman H, Massicotte C, Li R, Zabih W, McAdam LC, Al-Saleh S, et al. The accuracy of an ambulatory level III sleep study compared to a level I sleep study for the diagnosis of sleep-disordered breathing in children with neuromuscular disease. J Clin Sleep Med. 2018;14(12):2013–20.
Chatwin M, Ross E, Hart N, Nickol AH, Polkey MI, Simonds AK. Cough augmentation with mechanical insufflation/exsufflation in patients with neuromuscular weakness. Eur Respir J. 2003;21(3):502–8.
Fauroux B, Khirani S, Griffon L, Teng T, Lanzeray A, Amaddeo A. Non-invasive ventilation in children with neuromuscular disease. Front Pediatr. 2020;8:482.
Chatwin M, Bush A, Simonds AK. Outcome of goal-directed non-invasive ventilation and mechanical insufflation/exsufflation in spinal muscular atrophy type I. Arch Dis Child. 2011;96(5):426–32.
Ward S, Chatwin M, Heather S, Simonds A. Randomised controlled trial of non-invasive ventilation (NIV) for nocturnal hypoventilation in neuromuscular and chest wall disease patients with daytime normocapnia. Thorax. 2005;60(12):1019–24.
Berry RB, Chediak A, Brown LK, Finder J, Gozal D, Iber C, et al. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6(5):491–509.
Caldarelli V, Borel JC, Khirani S, Ramirez A, Cutrera R, Pépin JL, et al. Polygraphic respiratory events during sleep with noninvasive ventilation in children: description, prevalence, and clinical consequences. Intensive Care Med. 2013;39(4):739–46.
Gonzalez-Bermejo J, Perrin C, Janssens JP, Pepin JL, Mroue G, Léger P, et al. Proposal for a systematic analysis of polygraphy or polysomnography for identifying and scoring abnormal events occurring during non-invasive ventilation. Thorax. 2012;67(6):546–52.
Pepin JL, Borel JC, Contal O, Gonzalez-Bermejo J, Rabec C, Tamisier R, et al. Scoring abnormal respiratory events on polysomnography during noninvasive ventilation. Sleep Med Clin. 2014;9(3):327–39.
Finkel RS, Mercuri E, Darras BT, Connolly AM, Kuntz NL, Kirschner J, et al. Nusinersen versus sham control in infantile-onset spinal muscular atrophy. N Engl J Med. 2017;377(18):1723–32.
LoMauro A, Mastella C, Alberti K, Masson R, Aliverti A, Baranello G. Effect of nusinersen on respiratory muscle function in different subtypes of type 1 spinal muscular atrophy. Am J Respir Crit Care Med. 2019;200(12):1547–50.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Chan, K.CC. (2022). Sleep and Neuromuscular Diseases: Management and Use of NIV. In: Li, A.M., Chan, K.Cc. (eds) Paediatric Sleep Disorders. Springer, Singapore. https://doi.org/10.1007/978-981-19-5791-8_19
Download citation
DOI: https://doi.org/10.1007/978-981-19-5791-8_19
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-5790-1
Online ISBN: 978-981-19-5791-8
eBook Packages: MedicineMedicine (R0)