Abstract
Gastrointestinal stromal tumor (GIST) is the most common mesenchymal tumor originating in the gastrointestinal tract, originating from the interstitial cells of Cajal. GISTs occur most commonly in the stomach (60%), followed by the small intestine (30%) [1].
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Introduction
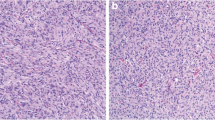
Gastrointestinal stromal tumor (GIST) is the most common mesenchymal tumor originating in the gastrointestinal tract, originating from the interstitial cells of Cajal. GISTs occur most commonly in the stomach (60%), followed by the small intestine (30%) [1].
The standard of care for localized GISTs is complete surgical resection without dissection of clinically negative lymph nodes [2]. Any GIST is considered potentially malignant, indications for surgery for gastric GISTs are as listed below. For non-gastric GISTs, surgical resection is recommended regardless of tumor size or morphology [3].
Indications for Surgery for Gastric GISTs
-
1.
Tumor >2 cm.
-
2.
Increase in size on follow-up.
-
3.
Signs of malignancy; irregular margins, cystic changes, necrosis, and heterogenous echogenicity.
-
4.
Symptomatic; ulceration and bleeding, gastric outlet obstruction (large antral GISTs).
The goal of surgery is R0 surgery (i.e., excision margins are clear of tumor cells). While laparoscopic surgery for gastric GISTs resection is associated with superior postoperative outcomes, the decision to undertake laparoscopic versus open surgery should be made at the discretion of the surgeon. The European Society for Medical Oncology (ESMO) guidelines discourage laparoscopy for patients with large tumors due to the risk of tumor rupture [2], while Otani et al. [4] suggest 5 cm as the limit for laparoscopic wedge resection. Intraoperative tumor rupture is associated with a very high risk of peritoneal relapse [5].
The initial diagnosis of a GIST is usually suggested by endoscopy, endoscopic ultrasound (EUS), or computed tomography (CT) of the abdomen. Preoperative histological diagnosis is not necessary unless considering neoadjuvant imatinib therapy [3]. Neoadjuvant imatinib therapy should be considered for localized GISTs when R0 resection is not feasible or for organ preservation [3]. En bloc resection of a GIST that has invaded surrounding organs may be necessary to achieve negative margins and to avoid tumor rupture [6]. The principles of surgery for GIST are negative margins, and resection without rupture of the tumor.
Surgical Technique
Instruments
-
12 mm ports, 5 mm ports
-
Nathanson retractor (for proximal gastric GISTs if liver retraction is required. Alternative methods of liver retraction may be used).
-
10 mm 30° laparoscope
-
Advanced energy device—author preference is the Harmonic 1000I.
-
Atraumatic graspers.
-
Clip applicator.
-
Suction/irrigation device.
-
Laparoscopic stapler.
Operating Room Setup and Patient Position
The patient is placed in the supine position with both arms out and a footboard. The laparoscopic stack is placed on the patient’s left, the machines for the energy devices are placed at the patient’s feet, and the suction machines are placed on the patient’s right.
The main surgeon stands on the patient’s right along with the camera assistant, while the first assistant stands on the patient’s left.
After the subumbilical port is placed, the abdominal cavity is inspected for evidence of peritoneal metastasis. Pneumoperitoneum is maintained at 12 mmHg. Location of the ports depends on the location of the tumor, but is generally similar to that used in laparoscopic gastrectomy.
Operative Steps
Stapled wedge resection can be easily performed for most anterior wall gastric GISTs. Tumor rupture must be avoided at all cost. The tumor should be handled gently if at all, while and the surrounding tissues can be sutured or handled for traction. To avoid stenosis, the tumor should be elevated and the stapler fired perpendicular to the long axis of the stomach. An extraction bag is recommended for retrieval of the specimen.
For tumors in the posterior gastric wall, the greater omentum may need to be incised in the avascular portion away from the gastroepiploic arcade in order to enter the lesser sac to reach the tumor.
For tumors near the greater or lesser curve, the omentum and feeding vessels will need to be ligated and dissected free in order to perform a wedge resection. This is best done with an energy device.
The most challenging gastric GIST surgeries are for endophytic tumors, or tumors located in the fundus, lesser curve, and the antrum.
Endophytic Gastric GIST on the Anterior Gastric Wall
Endophytic Tumors Located on the Anterior Gastric Wall (Fig. 1)
-
An incision is made on the anterior gastric wall adjacent to the tumor.
-
The tumor is then everted through the gastrostomy and lifted anteriorly (Fig. 2).
-
Lift both edges of the gastrostomy and staple across, resecting the tumor and stapling close the gastrostomy at the same time. Alternatively, the tumor can be excised with a stapler and the gastrostomy subsequently closed with sutures.
Endophytic Gastric GIST on the Posterior Gastric Wall
-
An incision is made on the anterior gastric wall overlying the tumor (Fig. 3).
-
The posterior wall tumor is lifted up through the gastrostomy and resected with a stapler (Fig. 4).
-
The anterior wall gastrostomy is closed with a stapler or with sutures.
Antral GISTs
-
Stapled wedge resection of broad antral tumors may be difficult to perform due to the thickened musculature of the antrum, making it less mobile.
-
Anterior wall tumors may be excised with an energy source, such as harmonic, and the gastrostomy closed transversely to prevent strictures. A gastrojejunostomy can be performed if there is concern of stenosis of the antrum/pylorus after excision.
-
In cases of large antral GISTs, it may not be possible to perform a wedge resection. A distal gastrectomy may be required to achieve negative resection margins.
Fundal/Lesser Curve/Cardioesophageal Junction (CEJ) GISTs
-
Resection of a fundal or lesser curve tumor should be performed over a bougie or gastroscope to ensure that the CEJ is not narrowed.
-
Intragastric resection may be performed for tumors located in the posterior wall near the CEJ, whereby laparoscopic ports are placed through the anterior gastric wall into the gastric lumen, and stapler resection is performed.
Other methods such as endoscopic submucosal dissection have been described. However, enucleation of GISTs is not considered standard treatment as GISTs do not form a true capsule, originates from the muscle layer (unlike early gastric cancer), and disruption of the pseudocapsule and perforation of the gastric wall may happen simultaneously resulting in peritoneal dissemination [7].
Postoperative Management
Margin status may not be a significant prognostic factor for GIST recurrence [8]. In cases where the resection margin has microscopic tumor cells (R1), postoperative imatinib therapy is recommended when the malignant potential is high (based on size and mitotic index). Routine surveillance can be performed for low-risk GISTs [3].
References
Soreide K, Sandvik OM, Soreide JA, Giljaca V, Jureckova A, Bulusu VR. Global epidemiology of gastrointestinal stromal tumours (GIST): a systematic review of population-based cohort studies. Cancer Epidemiol. 2016;40:39–46.
Casali PG, Abecassis N, Aro HT, et al. Gastrointestinal stromal tumours: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29(Suppl 4):iv267–iv78.
Koo DH, Ryu MH, Kim KM, et al. Asian consensus guidelines for the diagnosis and management of gastrointestinal stromal tumor. Cancer Res Treat. 2016;48(4):1155–66.
Otani Y, Furukawa T, Yoshida M, et al. Operative indications for relatively small (2-5 cm) gastrointestinal stromal tumor of the stomach based on analysis of 60 operated cases. Surgery. 2006;139(4):484–92.
Hohenberger P, Ronellenfitsch U, Oladeji O, et al. Pattern of recurrence in patients with ruptured primary gastrointestinal stromal tumour. Br J Surg. 2010;97(12):1854–9.
Gold JS, Dematteo RP. Combined surgical and molecular therapy: the gastrointestinal stromal tumor model. Ann Surg. 2006;244(2):176–84.
Kong SH, Yang HK. Surgical treatment of gastric gastrointestinal stromal tumor. J Gastric Cancer. 2013;13(1):3–18.
McCarter MD, Antonescu CR, Ballman KV, et al. Microscopically positive margins for primary gastrointestinal stromal tumors: analysis of risk factors and tumor recurrence. J Am Coll Surg. 2012;215(1):53–9. discussion 59–60
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Yeo, D., Rao, J. (2023). Gastric Gastrointestinal Stromal Tumor. In: Lomanto, D., Chen, W.TL., Fuentes, M.B. (eds) Mastering Endo-Laparoscopic and Thoracoscopic Surgery. Springer, Singapore. https://doi.org/10.1007/978-981-19-3755-2_38
Download citation
DOI: https://doi.org/10.1007/978-981-19-3755-2_38
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-3754-5
Online ISBN: 978-981-19-3755-2
eBook Packages: MedicineMedicine (R0)