Abstract
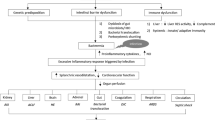
Patients with cirrhosis are susceptible to a wide variety of infections. Sepsis is an established precipitant of acute on chronic liver failure (ACLF). The occurrence of sepsis in cirrhosis is associated with high morbidity and mortality and warrants early recognition and prompt treatment. Antibiotics are widely used in patients with cirrhosis both prophylactically and as a part of treatment to control sepsis. However, since a majority of the antibiotics used are metabolized through the liver, it is important to take note of the altered pharmacodynamics and pharmacokinetics in cirrhosis while prescribing antibiotics. Drugs and medications can cause hepatic injury and exacerbate pre-existing liver disease, leading to decompensations and ACLF. Besides, patients with cirrhosis often have underlying renal dysfunction. This can be further potentiated by the use of nephrotoxic antibiotics. Antibiotics can also cause cytopenias, neurotoxicity, and skin injury. The emergence of drug-resistant bacteria is also a challenge in the setting of cirrhosis. Judicious and rational use of antibiotics, early de-escalation, and implementation of antibiotic stewardship programmes are essential to tackle the problem of drug resistance. Careful selection of antibiotics, knowledge of pharmacological profiles of antibiotics used, awareness of antibiotic-associated toxicities, and strategies to tackle drug resistance are important while prescribing antibiotics in patients with cirrhosis.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Moreau R, Jalan R, Gines P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144:1426–37, 1437.e1–9.
Fernández J, Acevedo J, Castro M, et al. Prevalence and risk factors of infections by multiresistant bacteria in cirrhosis: a prospective study. Hepatology. 2012;55:1551–61.
Gustot T, Durand F, Lebrec D, Vincent J-L, Moreau R. Severe sepsis in cirrhosis. Hepatology. 2009;50:2022–33.
Piano S, Tonon M, Vettore E, et al. Incidence, predictors and outcomes of acute-on-chronic liver failure in outpatients with cirrhosis. J Hepatol. 2017;67:1177–84.
Fernández J, Acevedo J, Wiest R, et al. Bacterial and fungal infections in acute-on-chronic liver failure: prevalence, characteristics and impact on prognosis. Gut. 2018;67:1870–80.
Arvaniti V, D’Amico G, Fede G, et al. Infections in patients with cirrhosis increase mortality four-fold and should be used in determining prognosis. Gastroenterology. 2010;139:1246–56, 1256.e1–5.
Foreman MG, Mannino DM, Moss M. Cirrhosis as a risk factor for sepsis and death: analysis of the National Hospital Discharge Survey. Chest. 2003;124:1016–20.
Jalan R, Fernandez J, Wiest R, et al. Bacterial infections in cirrhosis: a position statement based on the EASL special conference 2013. J Hepatol. 2014;60:1310–24.
Appenrodt B, Grünhage F, Gentemann MG, Thyssen L, Sauerbruch T, Lammert F. Nucleotide-binding oligomerization domain containing 2 (NOD2) variants are genetic risk factors for death and spontaneous bacterial peritonitis in liver cirrhosis. Hepatology. 2010;51:1327–33.
Nischalke HD, Berger C, Aldenhoff K, et al. Toll-like receptor (TLR) 2 promoter and intron 2 polymorphisms are associated with increased risk for spontaneous bacterial peritonitis in liver cirrhosis. J Hepatol. 2011;55:1010–6.
Soriano G, Sánchez E, Nieto JC, et al. Cytokine production in patients with cirrhosis and D299g and/or T399i toll-like receptor 4 polymorphisms. J Hepatol. 2013;58:S247–8.
Bauer TM, Steinbrückner B, Brinkmann FE, et al. Small intestinal bacterial overgrowth in patients with cirrhosis: prevalence and relation with spontaneous bacterial peritonitis. Am J Gastroenterol. 2001;96:2962–7.
Morencos FC, de las Heras Castaño G, Martín Ramos L, López Arias MJ, Ledesma F, Pons Romero F. Small bowel bacterial overgrowth in patients with alcoholic cirrhosis. Dig Dis Sci. 1995;40:1252–6.
Pande C, Kumar A, Sarin SK. Small-intestinal bacterial overgrowth in cirrhosis is related to the severity of liver disease. Aliment Pharmacol Ther. 2009;29:1273–81.
Chang CS, Chen GH, Lien HC, Yeh HZ. Small intestine dysmotility and bacterial overgrowth in cirrhotic patients with spontaneous bacterial peritonitis. Hepatology. 1998;28:1187–90.
Saitoh O, Sugi K, Lojima K, et al. Increased prevalence of intestinal inflammation in patients with liver cirrhosis. World J Gastroenterol. 1999;5:391–6.
Lorenzo-Zúñiga V, Bartolí R, Planas R, et al. Oral bile acids reduce bacterial overgrowth, bacterial translocation, and endotoxemia in cirrhotic rats. Hepatology. 2003;37:551–7.
Teltschik Z, Wiest R, Beisner J, et al. Intestinal bacterial translocation in rats with cirrhosis is related to compromised Paneth cell antimicrobial host defense. Hepatology. 2012;55:1154–63.
Assimakopoulos SF, Tsamandas AC, Tsiaoussis GI, et al. Altered intestinal tight junctions’ expression in patients with liver cirrhosis: a pathogenetic mechanism of intestinal hyperpermeability. Eur J Clin Investig. 2012;42:439–46.
Assimakopoulos SF, Charonis AS. Uncovering the molecular events associated with increased intestinal permeability in liver cirrhosis: the pivotal role of enterocyte tight junctions and future perspectives. J Hepatol. 2013;59:1144–6.
Tritto G, Bechlis Z, Stadlbauer V, et al. Evidence of neutrophil functional defect despite inflammation in stable cirrhosis. J Hepatol. 2011;55:574–81.
Wasmuth HE, Kunz D, Yagmur E, et al. Patients with acute on chronic liver failure display “sepsis-like” immune paralysis. J Hepatol. 2005;42:195–201.
Malik R, Mookerjee RP, Jalan R. Infection and inflammation in liver failure: two sides of the same coin. J Hepatol. 2009;51:426–9.
Fasolato S, Angeli P, Dallagnese L, et al. Renal failure and bacterial infections in patients with cirrhosis: epidemiology and clinical features. Hepatology. 2007;45:223–9.
Fernández J, Gustot T. Management of bacterial infections in cirrhosis. J Hepatol. 2012;56:S1–12.
O’Leary JG, Reddy KR, Wong F, et al. Long-term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis. Clin Gastroenterol Hepatol. 2015;13:753–9.e1-2.
Bajaj JS, O’Leary JG, Reddy KR, et al. Second infections independently increase mortality in hospitalized patients with cirrhosis: the north American consortium for the study of end-stage liver disease (NACSELD) experience. Hepatology. 2012;56:2328–35.
Merli M, Lucidi C, Giannelli V, et al. Cirrhotic patients are at risk for health care-associated bacterial infections. Clin Gastroenterol Hepatol. 2010;8:979–85.
Jalan R, Gines P, Olson JC, et al. Acute-on chronic liver failure. J Hepatol. 2012;57:1336–48.
Rodighiero V. Effects of liver disease on pharmacokinetics. An update. Clin Pharmacokinet. 1999;37:399–431.
Delcò F, Tchambaz L, Schlienger R, Drewe J, Krähenbühl S. Dose adjustment in patients with liver disease. Drug Saf. 2005;28:529–45.
Lewis JH. The rational use of potentially hepatotoxic medications in patients with underlying liver disease. Expert Opin Drug Saf. 2002;1:159–72.
Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. Lippincott Williams & Wilkins; 1999.
Amarapurkar DN. Prescribing medications in patients with decompensated liver cirrhosis. Int J Hepatol. 2011;2011:519526.
Bajaj JS, Liu EJ, Kheradman R, et al. Fungal dysbiosis in cirrhosis Gut. 2018;67:1146–54.
Brown GD, Denning DW, Gow NAR, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012;4:165rv13.
Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the Management of Candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1–50.
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis. 2004;39:309–17.
Kuti EL, Kuti JL. Pharmacokinetics, antifungal activity and clinical efficacy of anidulafungin in the treatment of fungal infections. Expert Opin Drug Metab Toxicol. 2010;6:1287–300.
Vekeman F, Weiss L, Aram J, et al. Retrospective cohort study comparing the risk of severe hepatotoxicity in hospitalized patients treated with echinocandins for invasive candidiasis in the presence of confounding by indication. BMC Infect Dis. 2018;18:438.
Glöckner A. Treatment and prophylaxis of invasive candidiasis with anidulafungin, caspofungin and micafungin: review of the literature. Eur J Med Res. 2011;16:167–79.
Bajaj JS, Heuman DM, Sanyal AJ, et al. Modulation of the metabiome by rifaximin in patients with cirrhosis and minimal hepatic encephalopathy. PLoS One. 2013;8:e60042.
Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362:1071–81.
Hanouneh MA, Hanouneh IA, Hashash JG, et al. The role of rifaximin in the primary prophylaxis of spontaneous bacterial peritonitis in patients with liver cirrhosis. J Clin Gastroenterol. 2012;46:709–15.
Vlachogiannakos J, Viazis N, Vasianopoulou P, Vafiadis I, Karamanolis DG, Ladas SD. Long-term administration of rifaximin improves the prognosis of patients with decompensated alcoholic cirrhosis. J Gastroenterol Hepatol. 2013;28:450–5.
Fernández J, Tandon P, Mensa J, Garcia-Tsao G. Antibiotic prophylaxis in cirrhosis: good and bad. Hepatology. 2016;63:2019–31.
Udy AA, Roberts JA, Lipman J. Clinical implications of antibiotic pharmacokinetic principles in the critically ill. Intensive Care Med. 2013;39:2070–82.
Ali N, Gupta N, Saravu K. Malnutrition as an important risk factor for drug-induced liver injury in patients on anti-tubercular therapy: an experience from a tertiary care center in South India. Drug Discov Ther. 2020;14:135–8.
Whitcomb DC, Block GD. Association of acetaminophen hepatotoxicity with fasting and ethanol use. JAMA. 1994;272:1845–50.
Li X, Gao P, Niu J. Metabolic comorbidities and risk of development and severity of drug-induced liver injury. Biomed Res Int. 2019;2019:8764093.
Cross FS, Long MW, Banner AS, Snider DE. Rifampin-isoniazid therapy of alcoholic and nonalcoholic tuberculous patients in a U.S. Public Health Service cooperative therapy trial. Am Rev Respir Dis. 1980;122:349–53.
Russo MW, Watkins PB. Are patients with elevated liver tests at increased risk of drug-induced liver injury? Gastroenterology. 2004;126:1477–80.
Wong WM, Wu PC, Yuen MF, et al. Antituberculosis drug-related liver dysfunction in chronic hepatitis B infection. Hepatology. 2000;31:201–6.
Patel PA, Voigt MD. Prevalence and interaction of hepatitis B and latent tuberculosis in Vietnamese immigrants to the United States. Am J Gastroenterol. 2002;97:1198–203.
Reuben A, Koch DG, Lee WM. Acute liver failure study group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76.
Devarbhavi H, Andrade RJ. Drug-induced liver injury due to antimicrobials, central nervous system agents, and nonsteroidal anti-inflammatory drugs. Semin Liver Dis. 2014;34:145–61.
Orlando R, Mussap M, Plebani M, et al. Diagnostic value of plasma cystatin C as a glomerular filtration marker in decompensated liver cirrhosis. Clin Chem. 2002;48:850–8.
Lodise TP, Lomaestro B, Graves J, Drusano GL. Larger vancomycin doses (at least four grams per day) are associated with an increased incidence of nephrotoxicity. Antimicrob Agents Chemother. 2008;52:1330–6.
Habib S, Patel N, Yarlagadda S, et al. Safety and efficacy of antibiotics among acutely decompensated cirrhosis patients. J Gastroenterol Hepatol. 2018;33:1882–8.
Dixit RK, Satapathy SK, Kumar R, et al. Pharmacokinetics of ciprofloxacin in patients with liver cirrhosis. Indian J Gastroenterol. 2002;21:62–3.
Montay G, Gaillot J. Pharmacokinetics of fluoroquinolones in hepatic failure. J Antimicrob Chemother. 1990;26:61–7.
Vuppalanchi R, Juluri R, Ghabril M, et al. Drug-induced QT prolongation in cirrhotic patients with transjugular intrahepatic portosystemic shunt. J Clin Gastroenterol. 2011;45:638–42.
Mattappalil A, Mergenhagen KA. Neurotoxicity with antimicrobials in the elderly: a review. Clin Ther. 2014;36:1489–511.e4.
Bhattacharyya S, Darby RR, Raibagkar P, Castro LNG, Berkowitz AL. Antibiotic-associated encephalopathy. Neurology. 2016;86:963–71.
Veirup N, Kyriakopoulos C. Neomycin [Internet]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021 [cited 2021 Oct 1]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK560603/
Loft S, Sonne J, Døssing M, Andreasen PB. Metronidazole pharmacokinetics in patients with hepatic encephalopathy. Scand J Gastroenterol. 1987;22:117–23.
Ianiro G, Tilg H, Gasbarrini A. Antibiotics as deep modulators of gut microbiota: between good and evil. Gut. 2016;65:1906–15.
Singh N, Yu VL, Mieles LA, Wagener MM. Beta-lactam antibiotic-induced leukopenia in severe hepatic dysfunction: risk factors and implications for dosing in patients with liver disease. Am J Med. 1993;94:251–6.
He Z-F, Wu X-A, Wang Y-P. Severe bone marrow suppression and hepatic dysfunction caused by piperacillin/tazobactam. Scand J Infect Dis. 2013;45:885–7.
Patil A, Khillan V, Thakur M, Kale P, Bihari C. Antimicrobial-induced Cytopenia and bone marrow Hypocellularity in patients with cirrhosis. Bone Marrow Res. 2018;2018:e4029648.
Devarbhavi H, Raj S. Drug-induced liver injury with skin reactions: drugs and host risk factors, clinical phenotypes and prognosis. Liver Int. 2019;39:802–11.
Lin Y-T, Wu P-H, Lin C-Y, et al. Cirrhosis as a risk factor for tuberculosis infection–a Nationwide longitudinal study in Taiwan. Am J Epidemiol. 2014;180:103–10.
Rifampin [Internet]. In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012 [cited 2021 Oct 1]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK548314/
Gupta NK, Lewis JH. Review article: the use of potentially hepatotoxic drugs in patients with liver disease. Aliment Pharmacol Ther. 2008;28:1021–41.
Saito A, Nagayama N, Yagi O, et al. Tuberculosis complicated with liver cirrhosis. Kekkaku. 2006;81:457–65.
Hawkins MT, Lewis JH. Latest advances in predicting DILI in human subjects: focus on biomarkers. Expert Opin Drug Metab Toxicol. 2012;8:1521–30.
Isoniazid [Internet]. In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012 [cited 2021 Oct 1]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK548754/
Kaneko Y, Nagayama N, Kawabe Y, et al. Drug-induced hepatotoxicity caused by anti-tuberculosis drugs in tuberculosis patients complicated with chronic hepatitis. Kekkaku. 2008;83:13–9.
Jahng AW, Tran T, Bui L, Joyner JL. Safety of treatment of latent tuberculosis infection in compensated cirrhotic patients during transplant candidacy period. Transplantation. 2007;83:1557–62.
Holty J-EC, Gould MK, Meinke L, Keeffe EB, Ruoss SJ. Tuberculosis in liver transplant recipients: a systematic review and meta-analysis of individual patient data. Liver Transplant. 2009;15:894–906.
Jafri S-M, Singal AG, Kaul D, Fontana RJ. Detection and management of latent tuberculosis in liver transplant patients. Liver Transplant. 2011;17:306–14.
Lacroix C, Tranvouez JL, Phan Hoang T, Duwoos H, Lafont O. Pharmacokinetics of pyrazinamide and its metabolites in patients with hepatic cirrhotic insufficiency. Arzneimittelforschung. 1990;40:76–9.
Kumar N, Kedarisetty CK, Kumar S, Khillan V, Sarin SK. Antitubercular therapy in patients with cirrhosis: challenges and options. World J Gastroenterol. 2014;20:5760–72.
Saigal S, Agarwal SR, Nandeesh HP, Sarin SK. Safety of an ofloxacin-based antitubercular regimen for the treatment of tuberculosis in patients with underlying chronic liver disease: a preliminary report. J Gastroenterol Hepatol. 2001;16:1028–32.
Fernández J, Prado V, Trebicka J, et al. Multidrug-resistant bacterial infections in patients with decompensated cirrhosis and with acute-on-chronic liver failure in Europe. J Hepatol. 2019;70:398–411.
Merli M, Lucidi C, Di Gregorio V, et al. The spread of multi drug resistant infections is leading to an increase in the empirical antibiotic treatment failure in cirrhosis: a prospective survey. PLoS One. 2015;10:e0127448.
Ariza X, Castellote J, Lora-Tamayo J, et al. Risk factors for resistance to ceftriaxone and its impact on mortality in community, healthcare and nosocomial spontaneous bacterial peritonitis. J Hepatol. 2012;56:825–32.
Tandon P, Delisle A, Topal JE, Garcia-Tsao G. High prevalence of antibiotic-resistant bacterial infections among patients with cirrhosis at a US liver center. Clin Gastroenterol Hepatol. 2012;10:1291–8.
Chan C, Levitsky J. Infection and alcoholic liver disease. Clin Liver Dis. 2016;20:595–606.
Bunchorntavakul C, Chavalitdhamrong D. Bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. World J Hepatol. 2012;4:158–68.
Fernandez J, Arroyo V. Bacterial infections in cirrhosis: a growing problem with significant implications. Clin Liver Dis. 2013;2:102–5.
Arabi YM, Dara SI, Memish Z, et al. Antimicrobial therapeutic determinants of outcomes from septic shock among patients with cirrhosis. Hepatology. 2012;56:2305–15.
European Association for the Study of the Liver. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69:406–60.
Viale P, Giannella M, Bartoletti M, Tedeschi S, Lewis R. Considerations about antimicrobial stewardship in settings with epidemic extended-Spectrum β-lactamase-producing or Carbapenem-resistant Enterobacteriaceae. Infect Dis Ther. 2015;4:65–83.
Fernández J, Bert F, Nicolas-Chanoine M-H. The challenges of multi-drug-resistance in hepatology. J Hepatol. 2016;65:1043–54.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Chouhan, S., Anirvan, P., Singh, S.P. (2022). Antibiotics in Liver Cirrhosis. In: Qi, X., Yang, Y. (eds) Pharmacotherapy for Liver Cirrhosis and Its Complications. Springer, Singapore. https://doi.org/10.1007/978-981-19-2615-0_4
Download citation
DOI: https://doi.org/10.1007/978-981-19-2615-0_4
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-2614-3
Online ISBN: 978-981-19-2615-0
eBook Packages: MedicineMedicine (R0)