Abstract
Facial trauma is often associated with severe morbidity with respect to loss of function and disfigurement. The maxilla is arguably the most anatomically intricate structure of the face and blunt trauma due to interpersonal violence, motor vehicle accidents, gunshot wounds, industrial accidents and falls contribute to etiology of maxillary fractures. Fractures of the midface are often challenging to the maxillofacial surgeon, due to wide variety of patterns of the fracture, diagnostic challenges and treatment dilemmas. The basic tenet in the management of these fractures is to reconstitute the vertical and horizontal buttresses of the midface, thus reestablishing structure and function. This chapter gives a comprehensive overview on the diagnosis, management and treatment of fractures of the Maxilla.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Complex midface trauma has challenged the diagnostic and operative skills of surgeons through the decades. Robert Marciani in his fifty year review article dated 1993, vividly described the challenges faced by early surgeons regarding the clinical and radiological diagnosis of mid face fractures and the compromised surgical results that may ensue [1].
1.1 History (Table 55.1)
In an area so anatomically complicated as the midface, the lines of fracture produced in the middle third are classified based upon the experimental studies of René Le Fort in 1901 [2]. The earliest known writings of maxillofacial fractures were recorded in the Edwin Smith papyrus in 1650 BC. Hippocrates who is often portrayed as the “Father of Medicine” described a myriad of facial injuries around 400 BC and his insight provided the basis for bandages and single jaw interdental wiring as methods of fixation and stabilization of facial fractures. Over the subsequent centuries, there appeared many techniques which in essence were variations of what Hippocrates had described. In the nineteenth century, Charles Fredrick Reiche provided the first detailed treatise on maxillary fractures [3]. It was also in the same century that Garretson and Blair advocated mandibular-maxillary fixation with the aid of splints to primarily treat maxillary fractures.
In 1901, a French surgeon René Le Fort published his classic paper on midfacial fracture patterns. He inflicted blunt facial trauma on cadavers, then subsequently removed the soft tissue and examined fracture patterns of the facial skeleton. This study has ever since been the basis for the description of maxillary fractures.
1.2 Surgical Anatomy/Osteology
The middle third of the facial skeleton is made up of the following bones (Fig. 55.1)
-
1.
Two maxillae
-
2.
Two zygomatic bones
-
3.
Two zygomatic processes of the temporal bones
-
4.
Two palatine bones
-
5.
Two nasal bones
-
6.
Two lacrimal bones
-
7.
The vomer
-
8.
The ethmoid and its attached conchae
-
9.
Two inferior conchae
-
10.
The pterygoid plates of the sphenoid
The middle third of the face is made up of a number of bones which rarely fractures in isolation. The complex nature of the midface is such that it will withstand the forces of mastication from below and provide protection in certain areas for vital structures. The middle third of the facial skeleton consists of a series of bone struts (buttresses) passing upwards from the upper teeth to the bones of the skull [4] (Fig. 55.2).
The relative fragility of the midface skeleton makes it act as a cushion for trauma directed towards the cranium from an anterior or anterolateral direction. The facial skeleton can be designated by this famous figure, where the skull is similar to a helmet, the midface is similar to a matchbox (crumble zone) and the mandible is similar to a hockey stick (Fig. 55.3). The most common causes of facial fractures in the adult population are assaults and motor vehicle accidents [5].
1.3 Applied Anatomy of the Midfacial Bones
The midface is composed of the nasal, zygoma, maxilla, ethmoid and its conchae, palatine, inferior concha and vomer which are collectively referred to as the middle third of the facial skeleton. The facial bones in isolation are comparatively fragile but gain strength and support as they articulate with each other. It is this strength that has often been described as the facial buttresses which Manson alluded to when describing the vertical and horizontal struts that support the facial skeleton [6]. The horizontal pillars are formed by the frontal bar (composed of the supraorbital rims and nasal process of the frontal bone), the zygomatic arch, the infraorbital rims and the nasal bridge and finally the alveolar process of the maxilla. The vertical pillars are the medial pillar formed by the piriform rims which continues superiorly as the frontal process of the maxilla. The zygomatic buttresses which continue superiorly with the lateral orbital rims form the lateral pillars, and the most caudal pillars are the pterygoid plates.
1.3.1 Maxilla
The maxilla consists of a central body and four processes, namely, the frontal, zygomatic, alveolar and palatine process. The body is hollowed out and contains the maxillary sinus. It is pyramidal shaped with the base being the medial surface facing the nasal cavity and the apex being elongated into the zygomatic process. It has an orbital or superior surface which forms the floor and rim of the orbit, a malar or anterolateral surface which forms part of the cheek and a posterolateral or infratemporal surface which contributes to the infratemporal fossa. The base is rimmed inferiorly by the alveolar process. The alveolar process houses the dental arch with the sockets varying in size according to the teeth. The palatine process is a horizontal process from the body to the alveolar process and medially articulates with the palatine process of the opposite maxilla, while posteriorly it articulates with the horizontal plate of the palatine bone. The zygomatic process is an extension of the anterolateral surface of the body which contributes to the zygomaticomaxillary suture. The frontal process projects upwards to articulate with the maxillary process of the frontal bone as well as the nasal bone anteriorly and the lacrimal bone posteriorly.
1.3.2 Vascular Supply and Innervation
The blood supply to the maxilla and the palatine bones is through the periosteum, the incisive artery and the greater and lesser palatine arteries. The internal maxillary artery lies posterior to the maxillae and the palatine bones and anterior to the pterygoid plates of sphenoid.
The maxillary nerve enters the caudal maxilla ventral to the orbit via the maxillary foramen and runs through the maxilla in the infraorbital canal giving off branches to supply the maxillary cheek and teeth. The nerve then exits the maxilla at the infraorbital foramen.
2 Classification
2.1 René Le Fort1901 [2]
Maxillary fractures were classified by René Le Fort based on his experiments on cadavers with low velocity unidirectional frontal trauma. Although the present-day maxillary fractures are caused due to high velocity multi directional trauma, the Le Fort classification is still widely followed due to its simplicity and the levels of anatomic differentiation it offers. Other authors have attempted classifications based on the anatomical sites and based on the involvement of the occlusion. Marciani modified the basic Le Fort classification by adding frontal bone and zygomatic fractures.
2.1.1 Le Fort I
2.1.1.1 Low Level Fracture/Guerin Fracture
The fracture line extends backwards from the lateral margin of the anterior nasal aperture below the zygomatic buttress to cross the lower third of the pterygoid laminae. The fracture also passes along the lateral wall of the nose and the lower third of the septum to join the lateral fracture behind the tuberosity (Fig. 55.4a–c).
2.1.2 Le Fort II
2.1.2.1 Pyramidal or Sub-zygomatic Fracture
This fracture runs from the thin middle area of the nasal bones down either side, crossing the frontal processes of maxillae into the medial wall of each orbit; the fracture line crosses the lacrimal bone behind the lacrimal sac before turning forwards to cross the infraorbital margins slightly medial to or through the infraorbital foramen. The fracture now extends downwards and backwards across the lateral wall of the antrum below the zygomaticomaxillary suture and divides the pterygoid laminae about half way up.
Separation of the block from the base of the skull is completed via the nasal septum and may involve the floor of the anterior cranial fossa (Fig. 55.5a–d).
2.1.3 Le Fort III
2.1.3.1 Transverse or Supra-zygomatic Fracture
The fracture runs from near the frontonasal suture transversely backwards and parallel with the base of the skull and involves the full depth of the ethmoid bone including the cribriform plate. Within the orbit the fracture passes below the optic foramen into the posterior limit of the inferior orbital fissure. From the base of the inferior orbital fissure, the fracture line extends in two directions: backwards across the pterygomaxillary fissure to fracture the roots of the pterygoid laminae and laterally across the lateral wall of the orbit separating the zygomatic bone from the frontal bone. In this way the entire middle third of the facial skeleton gets separated from the cranial base (Fig. 55.6a–c).
Le Fort classification does not take into consideration:
-
Dentoalveolar fractures
-
Palatal fractures
-
Bone loss
2.2 Killey’s Classification (1965) [2] (Table 55.2)
2.3 Rowe and Williams’s Classification (1985) [2] (Table 55.3)
Addenda
-
(i)
These fractures may occur unilaterally or be associated independently with a fracture of the zygomatic complex.
-
(ii)
There may be a midline separation of the maxillae and/or extension of the fracture pattern into the frontal or temporal bones.
2.4 Marciani (1993: Modification of Le Fort Fractures) [1]
Fractures involving the cranial base and other midface fracture configurations, including severely comminuted segments of the facial skeleton, were not classifiable by the traditional Le Fort scheme. Hence Marciani proposed a more precise system of describing fracture patterns to define the fracture configuration, establish an accurate diagnosis and to determine potential surgical approaches (Table 55.4).
2.5 Palatal Fractures Classification: Hendrickson’s Classification (1998) [7] (Figs. 55.7, 55.8, and 55.9; Table 55.5)
3 Clinical Features (Box 55.1)
3.1 Le Fort I Fractures
Gross facial swelling or facial disfigurement is generally not a feature of Le Fort I fractures, but oedema around the upper lip may occur. Soft tissue injury along the upper lip along with tearing of gingivae may occur due to the causative impact. There can be mobility of the upper dento-alveolus when digital pressure is applied. Mobility of the maxilla at the Le Fort I level must be differentiated from extended maxillary dentoalveolar fracture. Malocclusion may occur if the fracture is displaced or impacted. Dorsal and caudal pull of the medial pterygoid muscles can contribute to the posterior displacement of the maxilla and the resultant anterior open bite (Fig. 55.10a, b). Bilateral epistaxis is rare although emphysema may occur if the patient blows his nose. Ecchymosis in the upper buccal sulcus is a frequent finding. Percussion of the maxillary teeth produces a dull cracked cup sound. In case of inferiorly displaced Le Fort I fractures, the patient may have to keep the mouth open to accommodate the increased vertical dimension. Due to the extreme downward displacement of the maxilla, the nasal base is lost, leading to stretching of the soft tissues of that area, which makes it possible to see directly into the nares.
The posteriorly impacted Le Fort I fracture may result in an anterior open bite and in these cases the maxilla may be immobile. Usually the impacted maxilla can be mobilized by grasping the maxillary teeth and applying a firm anterior pull. A grate may be felt due to the movement between the fractured segments. In posteriorly impacted fractures, there may be damage to the cusps of maxillary teeth usually in the premolar region, caused by the upward impact of the mandibular teeth at the time of the trauma. The complete Le Fort I fracture may be associated with a split along the median palatal suture. Sometimes more than one fracture line may be present in the palate, so that either one or both fragments may be mobile (Fig. 55.11a–c).
3.2 Le Fort II Fractures
Marked facial disfigurement resulting from circumorbital ecchymosis and gross oedema can be a feature of Le Fort II fractures. Frequently the patient will not be able to open his eyelids to allow an ocular examination. Subconjunctival haemorrhage may be present, the posterior limit of which cannot be identified. Bilateral peri-orbital oedema and circumorbital ecchymosis (described as circumorbital as it follows the shape of the orbicularis oculi muscle) are described as racoon eyes or panda facies. There can be severe oedema of the face which is sometimes described as moon facies. Enophthalmos in case of orbital floor fractures may go undetected due to oedema. Considerable lengthening of face with posterior gagging of teeth can also occur. Bilateral epistaxis is common, and CSF leak may be present. The loss of maxillary prominence may result in a dish face appearance. If the fracture line passes through the infraorbital canal there can be associated paresthesia in the infraorbital nerve region. While clinically mobilizing the maxilla in a Le Fort II fracture, transmitted mobility may be felt at the infraorbital rim and the frontonasal suture. Figure 55.12 shows a CT image where Le Fort II and III lines are seen
3.3 Le Fort III Fractures (Also see Fig. 49.5)
This fracture is clinically similar to the Le Fort II fracture but can demonstrate a more serious condition. Bilateral ecchymosis with circumorbital oedema may close the eyes completely. As in Le Fort II, the posterior limit of the subconjunctival haemorrhage cannot be seen. The lengthening of the face occurs due to the loss of bony fixation to the base of the skull. The flattening of the face from the disrupted zygomatic bones is usually masked by the gross oedema. The fracture passes above the Whitnall’s tubercle and so the support by Lockwoods, suspensory ligament is lost. This results in hooding of upper eyelid which becomes obvious when the oedema subsides. Gagging of occlusion and shift of the maxillary midline may occur. Gross posterior displacement of the maxilla can result in the soft palate touching the posterior part of the tongue causing airway and speech impairment. As with other maxillary fractures, percussion of teeth might produce a cracked cup sound. .
The clinical differentiation between Le Fort II and Le Fort III fractures can be assessed by palpating for step deformity in the infraorbital rim in the former.
Box 55.1 Clinical features of Le Fort fractures
Clinical features | Le Fort I | Le Fort II | Le Fort III |
|---|---|---|---|
Intraoral | • Floating maxilla • Impacted or telescopic fracture • Anterior open bite • Deranged occlusion • Guerin’s sign • Palatal fracture in some cases | • Deranged occlusion • Posterior gagging of occlusion • Possible airway obstruction | • Deranged occlusion • Posterior gagging of occlusion • Possible airway obstruction |
Extraoral | • Mild swelling and oedema of midface and upper lip • Epistaxis in some cases • Increased visibility of anterior nares | • Moon face appearance • Peri-orbital oedema • Circumorbital ecchymosis • Subconjunctival haemorrhage • Infraorbital step deformity • Altered sensation of cheek • CSF rhinorrhea • Diplopia | • Separation at FZ suture • CSF rhinorrhea • Hooding of eyes • Anti-mongoloid slant • Dish face deformity |
3.4 Unusual Fracture Patterns
The Le Fort fractures may manifest without the classic fracture patterns as described above. An unilateral fracture at Le Fort I level may occur (identified through imaging) which warrants no intervention unless accompanied by a palatal fracture causing occlusal derangement and/or mobility. Such a unilateral fracture pattern can cause unilateral gagging causing open bite on the contralateral side
The clinician must be aware of the two types of Le Fort I fractures, the mobile and impacted variants; lack of mobility should not be presumed as absence of fracture.
4 Radiographic Examination
It is difficult to diagnose fractures of the middle third of the face with plain films and CT scans have now largely replaced radiographs.
The commonly used radiographs for identifying maxillary fractures are occipitomental view (OMV) 10° and 30° and paranasal sinus view 37° (PNS -Waters view).
While assessing maxillary fractures with these radiographs, Mcgregor-Campbell and Trapnell’s lines and Dolan’s lines (elephant of Rogers) may be kept in mind [8].
McGregor-Campbell’s lines:
These lines were described by McGregor and Campbell for ease of searching on an occipitomental view 10-degree frontal projection.
-
1.
First line across the zygomaticofrontal, the superior margin of the orbit and the frontal sinus
-
2.
Second line across the zygomatic arch, zygomatic body, inferior orbital margin and nasal bone
-
3.
Third line across the condyles, coronoid process and the maxillary sinus / Zygomatic buttress region
-
4.
Fourth line across the mandibular ramus, occlusal plane
-
5.
Fifth line (Trapnell’s line, added later) across the inferior border of the mandible from angle to angle (Fig. 55.13)
The four S’s described by Delbalso, Hall and Margarone [8]
In PNS view, the following four features are to be verified/compared with the unaffected side
-
1.
Symmetry
-
2.
Sharpness
-
3.
Sinus
-
4.
Soft tissues
Dolan’s Lines [8] (Fig. 55.14)
Dolan’s lines are the collective name given to three lines described by Dolan and Jacoby that aid in evaluating for maxillofacial fractures on an occipitomental skull radiograph. They are usually used as an adjunct to McGregor-Campbell lines.
-
Orbital line (line 1) traces the inner margins of the lateral, inferior and medial orbital walls and the nasal arch.
-
Zygomatic line (line 2) traces the superior margin of the zygomatic arch and body extending along the frontal process of the zygoma to the zygomaticofrontal suture.
-
Maxillary line (line 3) traces the inferior margin of the zygomatic arch, body, and buttress and the lateral wall of the maxillary sinus.Elephant of Rogers [8]Lee Rogers pointed out that the second and third lines of Dolan give the outline of the head of an elephant.
Fig. 55.14 Dolan’s lines (also see Fig. 56.22)
4.1 CT Scans
CT scans are now the gold standard for a definitive diagnosis in fractures of the maxilla. A CT scan in all three planes (axial, sagittal and coronal) along with a 3D reconstruction will aid the surgeon in accurate assessment of fracture patterns and also will aid in preoperative planning. The surgeon must never rely on the 3D CT alone but should correlate the images with those obtained in axial sagittal and coronal planes, as there could be reconstruction-related errors which appear as fracture lines or bone defects. CT scan-based fracture patterns may be classified as low, middle or high energy, defined solely by the pattern of segmentation and displacement in the CT scan [9].
5 Treatment of Maxillary fractures
The primary aim of treatment of maxillary fractures is to re-establish the dental occlusion and masticatory efficiency. The contribution of the maxilla to the projection and contour of the midface has also to be considered in the management of maxillary fractures and requires a clear understanding of the facial buttress system, subunit anatomy and inter-relationships of the various bones [10]. This aesthetic aspect is often compromised by associated injuries of the zygomatic complex, nose and orbits.
The basic principles of the treatment of maxillary fractures are:
-
1.
Direct exposure and manual reduction of the fractures
-
2.
Reconstitution of the bony buttresses of the midface so as to prevent elongation of the face and/or antero-posterior collapse of the maxilla
-
3.
Re-enforcement of the paranasal and zygomatic buttresses with mini-plates
-
4.
Replacement of missing/grossly comminuted bone at the buttresses with autogenous bone grafts [5]
Factors that influence improved treatment outcome in maxillary fractures are:
-
1.
Early definitive treatment
-
2.
Anatomic and functional repair of naso-orbito-ethmoidal injuries
-
3.
Wide exposure of fracture segments
-
4.
Anatomic repositioning and stable fixation of fracture segments in all planes of space [11]
5.1 General Considerations in Treatment of Maxillary Fractures
Proper reduction of maxillary fractures is the key to achieving good dental occlusion and needs proper clinical examination of the fracture pattern after all the accessible fracture sites are exposed. A repeat study of the CT scans (axial, coronal and 3D) and correlation with the exposed maxilla will aid the surgeon in planning adequate reduction and rigid fixation. It should be kept in mind that the fractured maxilla is usually displaced backwards and downwards and hence the reduction should in the forward and upward direction. To obtain reproducibly good results, even with the most extensive facial dislocations, the surgeon should restore the facial architecture at the Le Fort I Level [12]. In rare occasions, lateral en bloc displacement of the maxilla is seen, and this requires transverse reduction to achieve the correct dental occlusion. A depressed zygomatic fracture can physically prevent reduction of the maxilla. Hence the fractured zygomatic bone should be reduced prior to manipulating the maxilla.
The most useful instruments for reduction of the maxilla are the Rowe’s disimpaction forceps. Even in cases where the fractured maxilla appears to be minimally displaced, it is prudent to mobilize the bone with the disimpaction forceps so as to overcome any bony interferences and thus freeing the maxilla completely. When using this paired forceps, care should be taken to avoid injury to the anterior teeth and also to the palatal mucosa. Mobile, extruded and proclined anterior teeth are at particular risk, and an assistant should closely observe the anterior teeth, while the surgeon is manipulating the fractured maxilla. It would also be advisable to obtain informed consent regarding mobility or loss of these teeth. Trauma to the nasal floor is inevitable when mobilizing the maxilla using the reducing forceps, and some nasal bleeding is usually observed, but this rarely requires a nasal pack.
Adequate reduction of the fractured maxilla is confirmed by:
-
1.
Good dental occlusion
-
2.
Alignment of the paranasal, zygomatic and fronto-zygomatic bony buttresses
-
3.
Adequate reduction of all the observable fracture lines
Problems arise when the patient has few or no teeth and when there is gross comminution of maxilla. In these situations the surgeon has to make do with whatever landmarks are available, and in such cases compromised functional and cosmetic results are not uncommon.
Direct manipulation at the fracture lines is sometimes required especially when the fractured maxilla is telescoped into the superior normal bone. Care must be taken to prevent additional fractures at the bony margins during direct manipulation as this would make fixation more demanding. Using tie wires at the zygomatic buttresses, around the second maxillary premolars/first molars bilaterally and through anterior nasal spine is often useful to physically disimpact and pull the maxilla forwards and upwards thus ensuring good reduction.
When the maxilla is fractured in multiple levels (e.g. Le Fort I and III levels), reduction using the disimpaction forceps alone may not be adequate. The dental occlusion can be achieved, but the midface projection may be compromised. Here also a combination of reduction with disimpaction forceps, direct manipulation at the fracture site and the use of the above mentioned tie wires is often indicated.
Once adequate reduction of the fractured maxilla is obtained, it is mandatory that rigid maxillomandibular fixation (MMF) is applied. In almost all cases, well-adapted maxillary and mandibular arch bars are required as this ensures multiple points for the MMF. Failure to obtain rigid MMF or manually maintaining the dental occlusion during fixation can result in post-operative occlusal discrepancies. If surgical reduction and fixation of the maxilla has to be delayed, elastic traction will be helpful in obtaining a functional occlusion. The use of MMF screws definitely saves operating time but can be problematic if elastic traction is required later.
If the mandibular condylar fracture exists, this should be reduced and fixed prior to the MMF. Failure to do so may result in an open bite due to loss of posterior mandibular height.
5.2 Suspension Wiring
Internal wire suspension involves sandwiching the fractured portion of the maxilla between the mandible and the superior part of the facial skeleton/skull that is not fractured. The use of internal suspension wires is more or less obsolete unless there is severe comminution which precludes rigid internal fixation. Suspension wiring may also be the surgeon’s choice when there is presence of severe infection at the site of surgery (Fig. 55.15).
5.3 Rigid Internal Fixation
Although many wiring techniques were practised in the past, rigid internal fixation with titanium bone plates and screws of sufficient rigidity is now the standard of care. For internal fixation of the maxilla, titanium bone plates and screws of sufficient rigidity are used. For providing rigidity, screws with an outer diameter of 1.5 mm is commonly used.
5.4 Approaches to the Maxilla
When treating a very high Le Fort I fracture and in Le Fort II and III fractures, it may be necessary to use one or more of the following incisions, which are described in chapter 56 and 57 of this book:
-
1.
Skin incisions for exposure of the infraorbital rim. Extension of this incision medially ensures access to the lateral nasal area, while a lateral extension would give access to the upper portion of the zygomatic body.
-
2.
Upper eyelid or lateral eyebrow incision (blepharoplasty) to expose the fronto-zygomatic suture.
-
3.
An existing laceration with or without conservative extension for increased surgical access.
5.4.1 Maxillary Vestibular Approach
The maxilla can be approached through a variety of incisions, the most common being the maxillary vestibular approach. In addition to providing access to the lower part of the entire midfacial skeleton, this approach results in a hidden intraoral scar. This approach may result in disruption of the attachments of the facial muscles of the nasolabial region; hence careful repositioning during closure is recommended to avoid unaesthetic changes to the face. The muscles of importance are the nasalis group, the levator labii superioris alaeque nasi, the levator labii superioris, the levator anguli oris and the orbicularis oris. The vestibular incision and subsequent dissection causes stripping of origin/insertion of most muscles originating in the maxilla. These muscles tend to get reattached in a shortened manner due to the action of the zygomaticus muscle. Deepening of the alar groove and splaying of the alar bases, nostrils and nasal tip may occur following lateral displacement of the nasal modiolus. Soft tissue fullness loss in the naso-alveolar region may result in thinning and retraction of upper lip, reduced vermillion exposure and a obtuse nasolabial angle. Detachment of the levators of the upper lip may cause down turning of the corner of the mouth (Fig. 55.16).
Early intervention (7–10 days) with open reduction and fixation is the treatment of choice for maxillary Le Fort I fractures. Restoration of normal facial contour and occlusion is considered as optimal outcome of treatment. Bone reconstruction should be completed as early as possible to minimize shrinkage, stiffness and scarring of soft tissues [12].
In complex panfacial fracture management, many authors have stressed the importance of managing the Le-Fort fracture while reconstituting the facial architecture [13, 14].
Clinical Tips for approaching the Le Fort fracture via maxillary vestibular incision
-
The use of liquid paraffin will minimize trauma to the lips and corners of the mouth especially in patients with a small oral aperture.
-
It is important to place a high vestibular incision to ensure a wide gingival cuff of tissue which will aid in closure of the incision.
-
“Counter” elevation of the gingival cuff would aid in closure and also expose the root prominences, and this would be helpful during adaptation of the mini-plates and the subsequent screw fixation.
-
It is also recommended that the opening of the Stenson’s duct be identified so that injury to this structure is avoided when the buccal sulcus is stretched while making the incision.
-
Some surgeons mark the midline to ensure proper reapproximation of the tissues during closure. This is important in cases where one is forced to use an oral endotracheal tube exiting from one corner of the mouth which may distort the oral tissues.
-
Extension of the posterior end of the incision beyond the first molars may cause buccal fat herniation into the surgical site. This is of minimal concern but can be annoying to the surgeon during plate fixation.
-
Sharp elevation of the superior flap will ensure a subperiosteal plane of dissection, but this may not always be possible due to adherent tissue at the fracture sites and the presence of bony fragments in comminuted fractures. As far as possible, sizable fragments of loose bone with soft tissue attachments should be retained to avoid large gaps at the fracture site which might delay healing. Even completely denuded bone can be replaced as free autogenous grafts and fixed in place with tissue glue or fine stainless steel wires.
-
As the superior dissection proceeds, care should be taken to identify and protect the infraorbital nerve which may be involved in the fracture. It is also prudent to palpate the infraorbital margin to ensure that inadvertent entry into the orbit is avoided especially when comminution of the infraorbital rim and floor is present.
-
Once the flap has been adequately raised, long Langenbeck retractors placed superiorly and cheek retractors at the corners of the mouth will ensure good surgical exposure and adequate lighting and thus aid in reduction and fixation of the fracture (Fig. 55.17).
-
A variation which can be done is giving two separate vestibular incisions bilaterally without incising the midline frenal attachment. This variation will not disturb the mid line lip anatomy in cases where exposure of the anterior nasal spine region is not required.
5.5 Fixation of Le Fort I #
Adequate fixation of the fractured bone depends on two factors, namely, the rigidity of the plate and the friction between the bone fragments (buttressing of the bony segments). When a gap exists between the bone ends, the latter factor is missing. In these cases, non/fibrous union can result if the masticatory forces are greater than the rigidity of the plate. As a general principle, the paranasal and zygomatic buttresses must be rigidly fixed. The plates should be well adapted especially where the bone stock is poor. At least two screws must be present on either side of the fracture and more the number of screws, better the, load sharing, between the plate and the subjacent bone. Opposed to this is when there is no bone buttressing and the plate has to be ‘load bearing’. Also a minimum of two threads of the screw should engage the cortical bone. This may be a problem in thin areas as the anterior wall of the maxillary sinus and the alveolus where roots are present. In the edentulous maxilla, the bone quality is often compromised, and the lower end of the plate may need to be placed on the alveolus. This may necessitate removal of the plate prior to prosthodontic rehabilitation.
Obtaining rigid fixation becomes difficult when the buttresses are comminuted. If only one buttress is amenable for plating the reduction at this fracture interface along with reconstitution of the occlusion must be used as the template for repositioning the maxilla. When all the buttresses are comminuted, the surgeon has to “eye ball” the maxilla into the reduced position. In these situations, a long-span plate extending from the body of the zygomatic bone to the relatively thick bone in the area of the anterior nasal spine with or without a bone graft is often the only option available to maintain the vertical position of the floating maxilla. It has been stated that the lip-tooth relationship is helpful in deciding the position of the reduced maxilla, but in practice this is of limited use.Loss of bone at the buttresses may require the use of primary bone grafts [10]. Though it has been suggested that a gap of more than 5 mm at the buttresses requires a graft, rigid plate fixation followed by MMF is often enough to ensure bony healing.
In essence the decision to graft will depend on:
-
1.
The extend of the bony gap
-
2.
The quality of the bone available for plate fixation
-
3.
The rigidity of the fixation
-
4.
Use of post-operative MMF
-
5.
Loss of a large part of the anterior wall of the maxillary sinus (Fig. 55.18) (causing the overlying soft tissue to fall into the sinus causing a contour defect)
Primary bone grafting can be done using iliac bone (Fig. 55.26), split calvarium or split ribs. The calvarium is the preferred source because of the following reasons:
-
1.
Large amount of graft available
-
2.
Proximity to the operative field
-
3.
Minimal donor site morbidity
The disadvantage is that these grafts are brittle and cannot be contoured. The bone graft has to be mortised to fit the defect and must be fixed rigidly to the plate or lag screwed.
Incisions for open reduction can be placed from first molar to first molar regions through a vestibular approach for wide exposure of the fracture sites. Rowe’s disimpaction forceps and/or Hayton-Williams forceps can be used for mobilizing and reducing the fracture into position. The impacted type of Le Fort I fracture manipulation has to be done by grasping the maxilla with two pairs of Rowe’s disimpaction forceps. Osteotomizing the maxilla should be considered if there is significant interval between the time of trauma and surgery. Whenever possible a passive reduction of the maxilla with condyles firmly seated in their correct position should be ensured to avoid post-operative anterior open bite (Figs. 55.19, 55.20, and 55.21).
Use of Rowe’s disimpaction forceps | Rowe’s disimpaction forceps are available as paired (right and left) instruments |
Each instrument has two blades, one for engaging the palate (to be padded before use to avoid injury to the palatal mucosa) and one to be inserted through the nostril | |
The instrument has an outward bend at the handle which aids in the use of two forceps simultaneously | |
After engaging the forceps, the maxilla has to be moved in all planes to ensure adequate mobilisation |
Use of Hayton-Williams forceps | The Hayton-Williams forceps is used to hold the fractured maxilla together |
The instrument is inserted after vestibular incision and is engaged at the pterygoid region | |
This is the instrument of choice especially in cases with palatal bone fracture |
After reduction the maxilla should be placed into maxillomandibular fixation. The fixation of the fracture sites (four-point fixation) is done at the vertical pillars of nasomaxillary and zygomaticomaxillary (lateral piriform rim and zygomatic buttress regions) for which the preferred plates and screws used are 1.5-mm thickness with 6-mm long screws. In the zygomatic buttress regions, 2.0-mm profile plates also can be used. The mini-plates are fixed as close as possible to the lateral pyriform rim as the bone is thickest there. Usually stabilization of the fracture is achievable even if any three of the four buttresses are fixed. Apparently, gross communition at one of the buttress regions will not cause a significant risk of inadequate stabilization. The associated anterior wall of the maxillary sinuses is generally not fixed due to the relative thin nature of bone in this region. The larger free bone fragments can be repositioned and immobilized using wires or be used for reconstruction of orbital floor defects. The circumvestibular incision is closed with running resorbable sutures after ensuring that the midline of upper lip coincides with the facial midline (Fig. 55.22).
Maxillomandibular fixation of up to 6 weeks also can be considered as alternative for treatment though the results may be less satisfactory with added morbidity to the recovering patient. The readers are advised to refer chapter 50 to read about closed reduction / wiring and intermaxillary fixation techniques.
5.6 Fixation of Le Fort II Fractures
The pyramidal fracture has the apex of the fracture located at the nasofrontal suture region or at the midnasal bone level. The Le Fort II fractures are ideally fixed at the frontonasal suture region, bilateral infraorbital rims and also both zygomaticomaxillary buttresses. However in majority of the clinical situations fixation at the infra orbital rims and the zygomatic buttress regions gives reasonably good results. Most Nasal bone fractures associated with Le Fort II fractures can be adequately managed by closed reduction techniques. This may require the anaesthetist to change nasal intubation to oral intubation. A submental intubation may also be considered at the beginning of the procedure. If the nasofrontal segment is unstable, fixation of the area can be done through various approaches (existing laceration, Gull wing approach, etc.). A maxillary vestibular incision can frequently provide access to infraorbital fracture alignment and fixation in some cases. The lower eyelid approaches are not always mandatory for fixation unless simultaneous exploration and reconstruction of orbital floors are also planned.
In Le Fort II fractures that are complicated by an associated palatal fracture, surgical splints may be helpful in obtaining adequate reduction. Placement of maxilla mandibular fixation will ensure accurate alignment of midface structures (Fig. 55.23).
5.7 Fixation of Le Fort III Fractures
These are complex fractures which rarely occur in isolation and results in a dysjunction of the facial skeleton from the base of the cranium. The ideal repair time should be within 10–14 days following the injury but may get delayed due to neurosurgical issues and other comorbidities.
Incision design for Le Fort III fractures should facilitate adequate access for reduction as well as fixation of the naso-frontal, frontozygomatc and in some cases the zygomatic arches. Using existing lacerations for access avoids need of a coronal incision, as this allows for complete visualization, reduction and fixation of the frontal area and zygomatic arches. A lateral brow or upper blepharoplasty (supra-tarsal fold) incision may be used to approach the lateral orbital rims. Also in such cases, a thicker plate (2.0) placement at the lateral orbital rim may be beneficial. A coronal approach may have to be considered if bilateral fronto-zygomatic and nasofrontal fracture fixation is planned.
The occlusion is a reliable indicator of adequate reduction in cases where direct visualization of the fractured segment is not possible.
In Le Fort III fractures associated with other fractures (open facial/condyle fractures), various surgical sequences can be followed, which is discussed in chapter 60 on Panfacial fractures.
Rarely, Le Fort fractures may present without mobility, but show occlusal disturbances like crossbite, open bite or loss of intercuspation. These can be managed by using traction elastics but at times warrant mobilization and subsequent rigid fixation [15].
6 Complications of Le Fort Fractures (Table 55.6)
7 Palatal Fractures
Unlike many other areas of the midface, the palatal bone is relatively thick, and hence palatal fractures are not common. A palatal split makes reduction and fixation of maxillary fractures more difficult mainly due to the transverse instability which can cause medial collapse or outward splaying of the maxilla. The use of the Hayton-Williams forceps along with the disimpaction forceps will control outward splaying of the maxilla but at the risk of medially displacement of the dentate segment of the maxilla. Moreover, the use of all the three forceps effectively requires some amount of surgical expertise.
Moss et al. [16] have proposed a classification for palatal fractures. There is no consensus regarding the management of palatal fractures, but various options have been suggested.
-
1.
Transpalatal wires in the first molar region.
-
2.
Direct exposure of the fracture through an existing palatal laceration or an incision and rigid plate fixation.
-
3.
External fixation by fixing a screw on either side of the fracture and immobilization with a wire connecting the screws. Alternatively a palatal splint can be fabricated after sectioning a plaster model of the palate.
-
4.
Plating the labial fracture line.
-
5.
Plating the nasal floor.
Transpalatal wires are simple to apply and do not have the problems of soft tissue dehiscence and infection seen in the more invasive methods [17]. However, the reduction of the palatal fracture cannot be ensured, and the wires can be cumbersome to the patient as it affects speech and swallowing. If the palatal wires are passed through an infant feeding tube or a small gauge urinary catheter, injury to the dorsum of the tongue can be minimized. It is also noticed that palatal wires tend to become slack after a few days, and then their value in reduction and fixation of the fracture is questionable. Moreover, these wires are not an option in the edentulous maxilla.
Direct exposure and plate fixation are surgically demanding, but the fracture can be reduced and fixed under direct vision. Ceinfuegos et al. have described the technique of fixing the plate over the palatal mucosa, but this plate would have to be removed at a later date [18]. An alternative would be to use a resorbable plate and screws.
Ma et al. has documented the use of self-drilling screws on either side of the palatal fracture with wires to fix the fracture [19].
Palatal fractures of the sagittal or parasagittal variety can be stabilized by placing a mini-plate across the fracture line on the labial side. Occasionally the prominence of the anterior nasal spine has to be reduced to facilitate mini-plate placement.
The transpalatal reduction should be supplemented by fixation at the zygomaticomaxillary and nasomaxillary buttresses and the use of an arch bar [20].
Palatal fractures accompanied by soft tissue lacerations often cause a serious challenge to the surgeon regarding its management. The healing of the palatal soft tissue laceration is dependent on the exact reduction of the palatal vault and stabilization. Overzealous attempts at closure of the laceration without accurate reduction may compromise wound healing. A tension-free closure of the palatal mucosa is imperative for wound healing. In some cases, the ensuing oronasal communication will have to addressed secondarily (Fig. 55.25).
7.1 Surgical Splints
Concomitant fractures of the palate present additional challenges to the treatment of Le Fort fractures. They complicate the re-establishment of proper width and height of the maxilla. Depending on the fracture type, patient comorbidities and associated injuries, either closed reduction and wiring or rigid fixation may have to be performed. Dental impressions can be obtained and occlusion assessed prior to surgery. Fabrication of an acrylic splint may help in re-establishing the transverse width of the palate.
In cases of gross comminution with partial dentition, palatal splints are helpful. Splints are fabricated on casts on which model surgery has been performed. They are designed such that they cover the occlusal surfaces and heights of contour, and care should be taken as to not disturb the soft tissues. Holes placed in the occlusal surfaces in the splint aid in separately ligating it to the arch bar [21]. In case of edentulous patients, Gunning splints are usually used.
8 Special Considerations
8.1 Maxillary Fractures in Geriatric Patients
Advanced age and compromised medical fitness may increase the morbidity associated with surgical management of maxillary fractures. Loss of teeth leading to reduced alveolar bone, reduced vascularity of maxilla and greater pneumatisation of the maxillary sinuses, should be taken into consideration before attempting an open reduction and internal fixation. Modification of existing dentures or Gunning splints are viable options in this population.
8.2 Maxillary Fractures in Children
The long-term effects of maxillary fractures on skeletal growth are inconclusive at present. Mobile-displaced maxillary fractures in paediatric patients warrant open reduction and fixation. Removal of hardware in growing patients may be considered to overcome complications of plate translocation (shifting of the position of metal plate due to appositional bone growth), extrusion and possible growth restriction. Resorbable plating systems may offer a solution to overcome such complications.
8.3 Haemorrhage Control in Maxillary Fractures
Branches of the internal maxillary artery provide much of the vascular supply to the midface. In patients with epistaxis or bleeding, ligation of this artery may be necessary. Due to anastomoses from other branches of the internal and external carotid circulation, vascular insufficiency of the maxilla is unlikely even after ligature of maxillary artery. In certain conditions of intractable bleeding not amenable to control by normal packing methods, embolization methods have been used effectively.
9 Recent Advances
The use of pre-surgical stereolithographic models helps in plate contouring and precise positioning of fractured segments. Facilitation of the intraoperative three-dimensional bone positioning is possible due to development of sophisticated computed tomography, computer graphics hardware and image processing software capable of reproducing anatomic templates. Automated preoperative “mirroring” of the contralateral uninjured orbito-zygomaticomaxillary complex to the affected side can result in improved results. The use of intraoperative surgical navigation systems along with mobile cone beam CT improves intraoperative quality control. Endoscopic midface fracture management facilitates smaller incisions, reduced recovery time and minimal post-operative complications. These developments are discussed in the Chap. 41.
10 Conclusion
Maxillary fractures can sometimes occur with significant cosmetic and functional implications. Accurate diagnosis and early surgical intervention is essential for successful management of these fractures. The surgeon should keep in mind that the surgical management of maxillary fractures primarily aims at restoration of the vertical and horizontal support buttresses.
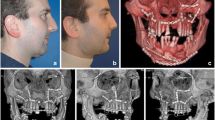
11 Case Scenario - A case of maxillary Lefort I fracture where bone grafting was done (Fig. 55.26a–g)
Case scenario (fracture maxilla fixation done with grafting in the anterior maxillary sinus wall). (a) 43-year-old man sustained bone deep laceration on face causing Le Fort I like fracture pattern. In the emergency department, oral intubation was required due to heavy bleeding. Nasal packs were placed, and the wound was primarily tacked as adjunct measures. (b) MIP view of CT scan showing the maxillary segment displaced downwards will loss of anterior maxillary wall height. (c) Intraoperative view showing the severely displaced maxillary segment. Access for the fixation was via the existing laceration. A maxillary vestibular incision was not placed. (d) The paranasal buttress was maintained, but loss of bone structure seen at the anterior wall sinus region. To attain primary healing and to avoid malunion, iliac crest bone grafts were procured and split into separate pieces. (e) (Right side maxilla) the green arrows point to the graft segments. Initially the graft segment was fixed with wire (blue arrow) and was attached to the titanium plate with screws (the plate was spanned from the zygomatic body to the displaced main fracture segment). (f) Similar technique done on left side. (g) Immediate post-operative view after closure of the laceration. Patient had arch bars fixed and underwent a period of intermaxillary fixation to help in primary union. Post-operative review showed good stability for maxilla and the occlusion was maintained
References
Marciani RD. Management of midface fractures: fifty years later. J Oral Maxillofac Surg. 1993;51(9):960–8. Review
Rowe and Williams’ maxillofacial injuries (ed 2): Williams JL (ed), with 51 contributors, New York: Churchill Livingstone; 1994, 1067 pages (2 volumes), illustrated. J Oral Maxillofac Surg. 1996;54(3):378.
Cunningham LL, Haug RH. Management of maxillary fractures. In: Miloro M, Ghali GE, Larson P, Waite P, editors. Peterson’s principles of oral and maxillofacial surgery. BC Decker; 2004. chapter 23.1, p. 434–8.
Gruss JS, Mackinnon SE. Complex maxillary fractures: role of buttress reconstruction and immediate bone grafts. Plast Reconstr Surg. 1986;78(1):9–22.
Louis M, Agrawal N, Kaufman M, Truong TA. Midface fractures I. Semin Plast Surg. 2017;31(2):85–93.
Manson PN, Hoopes JE, Su CT. Structural pillars of the facial skeleton: an approach to the management of Le Fort fractures. Plast Reconstr Surg. 1980;66:54–62.
Hendrickson M, Clark N, Manson PN, Yaremchuk M, Robertson B, Slezak S, Crawley W, Vander KC. Palatal fractures: classification, patterns, and treatment with rigid internal fixation. Plast Reconstr Surg. 1998;101(2):319–32.
Bowley NB, Brown J. Radiology for maxillofacial trauma. In Booth PW, Schendel SA, Hausamen J-E, editors. Maxillofacial surgery. Churchill Livingstone Elsevier; 2007. p. 278–9.
Manson PN, Markowitz B, Mirvis S, Dunham M, Yaremchuk M. Toward CT-based facial fracture treatment. Plast Reconstr Surg. 1990;85(2):202–12. Discussion 213–4
Gruss JS, Mackinnon SE. Complex maxillary fractures: role of buttress reconstruction and immediate bone grafts. Plast Reconstr Surg. 1986;78(1):9–22.
Nastri AL, Gurney B. Current concepts in midface fracture management. Curr Opin Otolaryngol Head Neck Surg. 2016;24(4):368–75.
Marciani RD, Gonty AA. Principles of management of complex craniofacial trauma. J Oral Maxillofac Surg. 1993;51(5):535–42.
Kelly KJ, Manson PN, Vander Kolk CA, Markowitz BL, Dunham CM, Rumley TO, Crawley WA. Sequencing Le Fort fracture treatment (Organization of treatment for a panfacial fracture). J Craniofac Surg. 1990;1(4):168–78.
Markowitz BL, Manson PN. Panfacial fractures: organization of treatment. Clin Plast Surg. 1989;16(1):105–14.
Romano JJ, Manson PN, Mirvis SE, Dunham M, Crawley W. Le Fort fractures without mobility. Plast Reconstr Surg. 1990;85(3):355–62.
Moss WJ, Kedarisetty S, Jafari A, Schaerer DE, Husseman JW. A review of hard palate fracture repair techniques. J Oral Maxillofac Surg. 2016;74(2):328–36. Review
Chen CH, Wang TY, Tsay PK, Lai JB, Chen CT, Liao HT, Lin CH, Chen YR. A 162-case review of palatal fracture: management strategy from a 10-year experience. Plast Reconstr Surg. 2008;121(6):2065–73.
Cienfuegos R, Sierra E, Ortiz B, Fernández G. Treatment of palatal fractures by osteosynthesis with 2.0-mm locking plates as external fixator. Craniomaxillofac Trauma Reconstr. 2010;3(4):223–30.
Ma D, Guo X, Yao H, Chen J. Transpalatal screw traction: a simple technique for the management of sagittal fractures of the maxilla and palate. Int J Oral Maxillofac Surg. 2014;43(12):1465–7.
Manson PN, Glassman D, Vanderkolk C, Petty P, Crawley WA. Rigid stabilization of sagittal fractures of the maxilla and palate. Plast Reconstr Surg. 1990;85(5):711–7.
Cohen SR, Leonard DK, Markowitz BL, Manson PN. Acrylic splints for dental alignment in complex facial injuries. Ann Plast Surg. 1993;31(5):406–12.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2021 The Author(s)
About this chapter
Cite this chapter
Jacob, O.A., Prathap, A. (2021). Maxillary Fractures. In: Bonanthaya, K., Panneerselvam, E., Manuel, S., Kumar, V.V., Rai, A. (eds) Oral and Maxillofacial Surgery for the Clinician. Springer, Singapore. https://doi.org/10.1007/978-981-15-1346-6_55
Download citation
DOI: https://doi.org/10.1007/978-981-15-1346-6_55
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-1345-9
Online ISBN: 978-981-15-1346-6
eBook Packages: MedicineMedicine (R0)