Abstract
Patients are heavily reliant on healthcare providers being knowledgeable and highly competent in a broad range of skills underpinned by sound knowledge. Some of these skills can be very specific, while others are rather general and may apply in combination or in parallel to others. The founding step to providing safe and effective patient care and working collaboratively with the wider clinical team lies in the acquisition of such skills. For learning to be imprinted in memory and then translated into performance, multiple factors come into play, such as the learners, the educators, the teaching methods, and the environment. The process is not the same for everyone, but some key educational principles prevail and some contribute to a better and faster assimilation of those skills. Simulation in particular, of which a broad range of modalities exist, and which are sometimes supported by more or less complex technology, is a particularly interesting approach as it promotes learner engagement, demonstration of competence, collaboration, and reflection. Simulation, in its various forms, has become a key element of the competency-based frameworks increasingly adopted in the educational process of healthcare learners and professionals. Its key aspects are that it is transformative for learners as it contributes to changing their mental frames and behaviors, helps them to assimilate new knowledge and skills, and promotes collaboration and reflection. The latter point is particularly important for nonprocedural clinical skills and can be promoted through structured feedback or debriefing phase following each simulation-based activity.
Similar content being viewed by others
References
Aldrich C. Simulations and the future of learning: an innovative (and perhaps revolutionary) approach to e-learning. San Francisco, CA, USA: Wiley; 2003.
Ali J, Adam R, Pierre I, Bedaysie H, Josa D, Winn J. Comparison of performance 2 years after the old and new (interactive) ATLS courses. J Surg Res. 2001;97(1):71–5.
Alinier G. Enhancing trainees’ learning experience through the opening of an advanced multiprofessional simulation training facility at the University of Hertfordshire. Br J Anaesth Recover Nurs. 2007a;8(2):22–7.
Alinier G. A typology of educationally focused medical simulation tools. Med Teach. 2007b;29(8):e243–50.
Alinier G, Granry J-C. Fundraising: a potential additional source of income for the research and educational activities of a healthcare simulation program. In: Palaganas J, Mancini B, Maxworthy J, Epps C, editors. Defining excellence in simulation programs. Philadelphia, USA: Wolters Kluwer; 2015. p. 321–8.
Alinier G, Hssain I. Creating effective learning environments: the educator’s perspective. In: Chiniara G, editor. Clinical simulation: education, operations, and engineering. 2nd ed. London: Elsevier; 2019. p. 217–27.
Alinier G, Verjee M. Learning through play. In: Chinniara G, editor. Clinical simulation: education, operations, and engineering. 2nd ed: London, Elsevier; 2019. p. 157-169.
Alinier G, Harwood C, Harwood P, Montague S, Huish E, Ruparelia K, et al. Immersive clinical simulation in undergraduate health care interprofessional education: knowledge and perceptions. Clin Simul Nurs. 2014;10(4):e205–e16.
Alinier G, Bello F, Kalbag A, Kneebone R. Space: Potential locations to conduct full-scale simulation-based education. In: Palaganas J, Mancini B, Maxworthy J, Epps C, editors. Defining excellence in simulation programs. Wolters Kluwer; 2015. p. 455–64.
Anton NE, Bean EA, Hammonds SC, Stefanidis D. Application of mental skills training in surgery: a review of its effectiveness and proposed next steps. J Laparoendosc Adv Surg Techn. 2017;27(5):459–69.
Athreya BH. Handbook of clinical skills: a practical manual. Hackensack: World Scientific; 2010.
Baldwin TT, Ford JK. Transfer of training: a review and directions for future research. Pers Psychol. 1988;41(1):63–105.
Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52(1):1–26.
Barton D, Mashlan W. An advanced nurse practitioner-led service–consequences of service redesign for managers and organizational infrastructure. J Nurs Manag. 2011;19(7):943–9.
Bedir S. Healthcare expenditure and economic growth in developing countries. Adv Econ Bus. 2016;4(2):76–86.
Benbassat J, Baumal R, Heyman SN, Brezis M. Suggestions for a shift in teaching clinical skills to medical students: the reflective clinical examination. Acad Med. 2005;80(12):1121–6.
Birnbach DJ, Rosen LF, Williams L, Fitzpatrick M, Lubarsky DA, Menna JD. A framework for patient safety: a defense nuclear industry–based high-reliability model. Jt Comm J Qual Patient Saf. 2013;39(5):233–40.
Boker A. Setup and utilization of Clinical Simulation Center, Faculty of Medicine, KING Abdulaziz University, Saudi Arabia. Life Sci J. 2013;10(1):1079–85.
Boursicot KA. Structured assessments of clinical competence. Br J Hosp Med. 2010;71(6):342–4.
Bradley P, Postlethwaite K. Setting up a clinical skills learning facility. Med Educ. 2003;37(1):6–13.
Breen KJ, Hogan AM, Mealy K. The detrimental impact of the implementation of the European working time directive (EWTD) on surgical senior house officer (SHO) operative experience. Ir J Med Sci. 2013;182(3):383–7.
Breymier T, Rutherford-Hemming T. Use of high-fidelity simulation to increase knowledge and skills in caring for patients receiving blood products. Crit Care Nurs Clin. 2017;29(3):369–75.
Brightwell A, Grant J. Competency-based training: who benefits? Postgrad Med J. 2013;89(1048):107.
Buja LM. Medical education today: all that glitters is not gold. BMC Med Educ. 2019;19(1):110.
Chiniara G, Cole G, Brisbin K, Huffman D, Cragg B, Lamacchia M, et al. Simulation in healthcare: a taxonomy and a conceptual framework for instructional design and media selection. Med Teach. 2013;35(8):e1380–95.
Collins A, Brown JS, Newman SE. Cognitive apprenticeship: teaching the craft of reading, writing and mathematics. Thinking J Philos Children. 1988;8(1):2–10.
Dale E. Audiovisual methods in teaching. New York: Dryden Press; 1969.
Davis D, O’Brien MAT, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282(9):867–74.
de Oliveira Barbosa AP, Sebastiani RL, Bez MR, Flores CD, de Castro MS. Use of a simulator to develop clinical skills for pharmacists. In: Cruz-Cunha MM, Miranda IM, Martinho R, Rijo R, editors. Encyclopedia of E-Health and telemedicine. Hershey: IGI Global; 2016. p. 412–21.
Der Sahakian G, Alinier G, Savoldelli G, Oriot D, Jaffrelot M, Lecomte F. Setting conditions for productive debriefing. Simul Gaming. 2015;46(2):197–208.
Der Sahakian G, Buléon C, Alinier G. Educational foundations of instructional design applied to simulation-based education. In: Chiniara G, editor. Clinical simulation: education, operations, and engineering. 2nd ed. London: Elsevier; 2019. p. 185–206.
Dieckmann P, Patterson M, Lahlou S, Mesman J, Nyström P, Krage R. Variation and adaptation: learning from success in patient safety-oriented simulation training. Adv Simul. 2017;2(1):21.
Dow A, Thibault G. Interprofessional education-a foundation for a new approach to health care. N Engl J Med. 2017;377(9):803.
Duvivier RJ, van Dalen J. Learning in the Skillslab. In: Al Alwan I, Magzoub ME, Elzubeir M, editors. International handbook of medical education: a guide for students. SAGE; 2012. p. 169–75.
Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(10):S70–81.
Fish D, Coles C. Medical education: developing a curriculum for practice: developing a curriculum for practice. Berkshire: McGraw-Hill Education; 2005.
Flegel KM. Does the physical examination have a future? Can Med Assoc J. 1999:1117–8.
Gross R. Psychology: the science of mind and behaviour 7th edition: Hodder Education; 2015.
Hean S. Strengthening the links between practice and education in the development of collaborative competence frameworks. In: Vyt A, Pahor M, Tervaskanto-Meantausta T, editors. Interprofessional education in Europe: policy and practice. Antwerp: Garant Publishers; 2015. p. 9–36.
Houghton CE, Casey D, Shaw D, Murphy K. Staff and students' perceptions and experiences of teaching and assessment in clinical skills laboratories: interview findings from a multiple case study. Nurse Educ Today. 2012;32(6):e29–34.
Houghton CE, Casey D, Shaw D, Murphy K. Students’ experiences of implementing clinical skills in the real world of practice. J Clin Nurs. 2013;22(13-14):1961–9.
Jones I, Alinier G. Supporting students’ learning experiences through a pocket size Cue Card designed around a reflective simulation framework. Clin Simul Nurs. 2015;11(7):325–34.
Jünger J, Schäfer S, Roth C, Schellberg D, Friedman Ben-David M, Nikendei C. Effects of basic clinical skills training on objective structured clinical examination performance. Med Educ. 2005;39(10):1015–20.
Karlsen R. Stable Program. Adaptation of the RUS model. Original work from the Center for Medical Simulation (D.R.), Cambridge, MA. 2013.
Ker J, Bradley P. Simulation in medical education. In: Swanwick T, editor. Understanding medical education: evidence, theory, and practice. Chichester: Wiley; 2013. p. 175–92.
Kessler DO, Walsh B, Whitfill T, Gangadharan S, Gawel M, Brown L, et al. Disparities in adherence to pediatric sepsis guidelines across a spectrum of emergency departments: a multicenter, cross-sectional observational in situ simulation study. J Emergency Med. 2016;50(3):403–15.e3.
Kneebone R. Simulation, safety and surgery. Qual Saf Health Care. 2010;19(Suppl 3):i47–52.
Knowles MS. The modern practice of adult education: from pedagogy to andragogy. 2nd ed. New York: Cambridge Books; 1980.
Knowles MS. Andragogy in action: applying principles of adult learning. San Farancisco: Jossey-Bass; 1984.
Kolb DA, Boyatzis RE, Mainemelis C. Experiential learning theory: previous research and new directions. Perspectives Thinking Learn Cognitive Styles. 2001;1:227–47.
Kurtz S, Silverman J, Draper J. Teaching and learning communication skills in medicine. 2nd ed. Abingdon, UK: CRC Press; 2017.
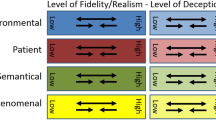
Kyaw Tun J, Alinier G, Tang J, Kneebone RL. Redefining simulation Fidelity for healthcare education. Simul Gaming. 2015;46(2):159–74.
Lai A, Haligua A, Bould MD, Everett T, Gale M, Pigford A-A, et al. Learning crisis resource management: practicing versus an observational role in simulation training–a randomized controlled trial. Anaesthesia Crit Care Pain Med. 2016;35(4):275–81.
LaRosa C, Grant-Kels JM. See one, do one, teach one: the ethical dilemma of residents performing their first procedure on patients. J Am Acad Dermatol. 2016;75(4):845–8.
Lave J, Wenger E. Situated learning: legitimate peripheral participation. Cambridge: Cambridge University Press; 1991.
Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. BMJ Qual Saf. 2004;13(suppl 1):i85–90.
Liu D, Blickensderfer EL, Macchiarella ND, Vincenzi DA. Transfer of training. In: Hancock PA, Vincenzi DA, Wise JA, Mouloua M, editors. Human factors in simulation and training. Boca Raton: CRC Press; 2009. p. 49–60.
Lord T. Revisiting the cone of learning: is it a reliable way to link instruction method with knowledge recall? J Coll Sci Teach. 2007;37(2):14–7.
Mahesh B, Sharples L, Codispoti M. Effect of the full implementation of the European working time directive on operative training in adult cardiac surgery. J Surg Educ. 2014;71(4):492–9.
Masters K. Edgar Dale’s pyramid of learning in medical education: a literature review. Med Teach. 2013;35(11):e1584–e93.
Masters K. Edgar Dale’s pyramid of learning in medical education: further expansion of the myth. Med Educ. 2019.
Masterson A. Cross-boundary working: a macro-political analysis of the impact on professional roles. J Clin Nurs. 2002;11(3):331–9.
McGaghie WC, Issenberg SB, Cohen MER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med J Assoc Am Med Coll. 2011;86(6):706–11.
McKimm J, Jollie C. Facilitating learning: teaching and learning methods. 2007. https://www.academiaedu/download/56698746/Facilitating_learning_teaching_-_learning_methods.pdf. Accessed 09 Apr 21.
Merriam SB. Andragogy and self-directed learning: pillars of adult learning theory. New Directions Adult Continuing Educ. 2001;2001(89):3–14.
Merriam SB. The role of cognitive development in Mezirow’s transformational learning theory. Adult Educ Q. 2004;55(1):60–8.
Michels MEJ, Evans DE, Blok GA. What is a clinical skill? Searching for order in chaos through a modified Delphi process. Med Teach. 2012;34(8):e573–e81.
Murphy P, Nestel D, Gormley GJ. Words matter: towards a new lexicon for ‘nontechnical skills’ training. Adv Simul. 2019;4(1):8.
O'Connell J, Gardner G, Coyer F. Beyond competencies: using a capability framework in developing practice standards for advanced practice nursing. J Adv Nurs. 2014;70(12):2728–35.
Oriot D, Alinier G. Pocket book for simulation debriefing in healthcare. Cham: Springer; 2018.
Peyton JR. Teaching & learning in medical practice. Rickmansworth, UK: Manticore Europe Limited; 1998.
Ramsden P. Learning to teach in higher education. London: Routledge; 2003.
Rethans JJ, Norcini J, Baron-Maldonado M, Blackmore D, Jolly B, LaDuca T, et al. The relationship between competence and performance: implications for assessing practice performance. Med Educ. 2002;36(10):901–9.
Riggs M, Franklin R, Saylany L. Associations between cardiopulmonary resuscitation (CPR) knowledge, self-efficacy, training history and willingness to perform CPR and CPR psychomotor skills: a systematic review. Resuscitation. 2019;138:259–72.
Riley RH, Grauze AM, Chinnery C, Horley RA, Trewhella NH. Three years of “CASMS”: the world’s busiest medical simulation Centre. Med J Aust. 2003;179(11/12):626–30.
Rodriguez-Paz J, Kennedy M, Salas E, Wu AW, Sexton J, Hunt E, et al. Beyond “see one, do one, teach one”: toward a different training paradigm. BMJ Qual Saf. 2009;18(1):63–8.
Romig T. The hijacking of Flight ET 702: the challenges of managing a major security threat, media attention and continuing daily airport operations. J Airport Manag. 2015;9(4):310–6.
Salas E, Bowers CA, Rhodenizer L. It is not how much you have but how you use it: toward a rational use of simulation to support aviation training. Int J Aviat Psychol. 1998;8(3):197–208.
Sawyer T, Brett-Fleegler M, Eppich WJ. Essentials of debriefing and feedback. In: Grant V, Cheng A, editors. Comprehensive healthcare simulation: pediatrics: Springer; 2016. p. 31-42.
Shafiq Z, Mufti TS, Qayum I. Role of clinical skill centre in undergraduate medical education: Initial experience at Rehman Medical College Peshawar encounter. J Pak Med Assoc. 2017;2:4.
Shortliffe EH, Sepúlveda MJ. Clinical decision support in the era of artificial intelligence. JAMA. 2018;320(21):2199–200.
Sinha R. The anatomy of success: management lessons from a surgeon. Noida, India: HarperCollins India; 2016.
Smith KK, Gilcreast D, Pierce K. Evaluation of staff's retention of ACLS and BLS skills. Resuscitation. 2008;78(1):59–65.
St Pierre M, Hofinger G, Buerschaper C. Crisis management in acute care settings: human factors, team psychology, and patient safety in a high stakes environment. Berlin: Springer; 2008.
Swanwick T. Understanding medical education: evidence, theory, and practice. Chichester: Wiley; 2013.
Taylor A, Dixon-Hardy DW, Wright SJ. Simulation training in UK general aviation: an undervalued aid to reducing loss of control accidents. Int J Aviat Psychol. 2014;24(2):141–52.
Yang C-W, Yen Z-S, McGowan JE, Chen HC, Chiang W-C, Mancini ME, et al. A systematic review of retention of adult advanced life support knowledge and skills in healthcare providers. Resuscitation. 2012;83(9):1055–60.
Yune SJ, Lee SY, Im SJ, Kam BS, Baek SY. Holistic rubric vs. analytic rubric for measuring clinical performance levels in medical students. BMC medical education. 2018;18(1):124.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this entry
Cite this entry
Alinier, G., Shehatta, A.L., Makker, R. (2021). Simulation for Clinical Skills in Healthcare Education. In: Nestel, D., Reedy, G., McKenna, L., Gough, S. (eds) Clinical Education for the Health Professions. Springer, Singapore. https://doi.org/10.1007/978-981-13-6106-7_93-1
Download citation
DOI: https://doi.org/10.1007/978-981-13-6106-7_93-1
Received:
Accepted:
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-6106-7
Online ISBN: 978-981-13-6106-7
eBook Packages: Springer Reference EducationReference Module Humanities and Social SciencesReference Module Education