Abstract
Glutathione (GSH) deficiency may play a pivotal role in a variety of apparently unrelated clinical conditions and diseases. Orally administered N-acetylcysteine (NAC), which replenishes the cysteine required for GSH synthesis, has been tested in a large number of randomized placebo-controlled trials involving these diseases and conditions. This chapter focused on developing a base of evidence suggesting that NAC administration improves disease by increasing cysteine and/or GSH in a variety of diseases, thereby implying a significant role for GSH deficiency in the clinical basis of many diseases. To develop this base of evidence, we systematically selected studies which considered the hypothesis that the therapeutic efficacy for NAC is an indication that cysteine and/or GSH deficiency is a pathophysiological part of the diseases studied. In this manner we focus this chapter on explaining the biological mechanisms of NAC therapy in a wide variety of disorders and demonstrate its ubiquitous role in improving disease that involves disrupted GSH and/or cysteine metabolism.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Randomized Placebo-controlled Trial (RPCTs)
- Cysteine Requirement
- APAP Overdose
- Cysteine Supply
- APAP Toxicity
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Life-threatening hepatotoxicity in the setting of acetaminophen (APAP) overdose is due to depletion of glutathione (GSH), a vital cysteine-containing tripeptide that protects cells and organs against oxidant injury. GSH depletion can occur when supplies of cysteine are inadequate to maintain GSH homeostasis in the face of the increased GSH consumption. Thus, rapid administration of N-acetylcysteine (NAC), which is converted to cysteine by first-pass metabolism and provides the cysteine necessary to replenish the depleted GSH, is the standard of care for preventing injury in APAP overdose.
GSH deficiency has also been recognized in a variety of apparently unrelated clinical conditions and diseases. NAC has been widely tested in randomized placebo-controlled trials (RPCTs) for efficacy in these diseases and conditions. In this chapter, we systematically review reports from early trials of NAC, which collectively suggest that GSH deficiency may be a common occurrence and that NAC may be a useful therapeutic adjunct for treating or preventing the development of this deficiency.
2 Methods
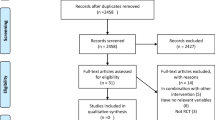
Publications included in this systematic literature review describe results from RPCT testing NAC for efficacy in a variety of disease settings. Publications were located by searching with the keywords “placebo AND N-acetylcysteine AND NOT animal” as well as “placebo AND N-acetylcysteine AND human, AND NOT animal.” We searched PubMed, the NLM database, the FDA website, Cochrane Database, Google, and subsequent material through 2006 and the references lists of all placebo- and non-placebo-controlled trials that we review here. This search identified nearly 2000 relevant publications. Within these, we identified 102 RPCTs that met the strict criteria for inclusion that we set for this review, i.e., publications reporting results from RPCT in which at least 10 subjects were used to test the efficacy of NAC administered without other drugs. Findings reported for these trials are summarized in tabular form (Online Tables 20.2 and 20.3) and discussed in the text. Trials excluded are listed in Online Table 20.1. Clinical studies relevant to the findings here but not conducted under strictly controlled conditions are found in Online Table 20.4.
3 Results
3.1 Glutathione (GSH)
Rapid administration of NAC is the standard of care for preventing hepatic injury in APAP overdose. The administered NAC is converted by first-pass metabolism to cysteine, which is needed to replenish the cysteine-containing intracellular tripeptide (l-γ-glutamyl-l-cysteinyl-glycine), commonly known as GSH. GSH is depleted during detoxification of excessive amounts of APAP. If it is not rapidly replenished, severe hepatic injury ensues.
In addition to this well-known use of NAC, at least 102 RPCTs conducted over 25 years have examined the effects of NAC treatment in respiratory, cardiovascular, endocrine, and infectious and other disease settings. Of these, 72 reported beneficial effects (Keays et al. 1991; Jackson et al. 1984; Ardissino et al. 1997; Andersen et al. 1995; Altomare et al. 1996; Aylward et al. 1980; Akerlund et al. 1996; Adair et al. 2001; Bromley et al. 1995; Badaloo et al. 2002; Boesgaard et al. 1992; Brocard et al. 1980; Bernard et al. 1997; Breitkreutz et al. 2000b; Bowles and Goral 1985; Diaz-Sandoval et al. 2002; Drager et al. 2004; De Mattia et al. 1998a, b; Dueholm et al. 1992; De Backer et al. 1996; De Flora et al. 1997; De Rosa et al. 2000; Estensen et al. 1999; Eren et al. 2003; Efrati et al. 2003; Evald et al. 1989; Fischer et al. 2004; Fulghesu et al. 2002; Ferrari 1980; Boman et al. 1983; Grassi 1980; Grassi and Morandini 1976; Horowitz et al. 1988a, b; Hansen et al. 1994; Heinig et al. 1985; Hauer et al. 2003; Herzenberg et al. 1997; Kay et al. 2003; Kasielski and Nowak 2001; McGavin 1985; MacNeill et al. 2003; Olivieri et al. 1985; Ovesen et al. 2000; Pace et al. 2003; Parr and Huitson 1987; Reinhart et al. 1995; Ratjen et al. 1985; Rasmussen and Glennow 1988; Rank et al. 2000; Shyu et al. 2002; Scholze et al. 2004; Spies et al. 1994, 1996; Spapen et al. 1998; Spada et al. 2002; Suter et al. 1994; Svendsen et al. 1989; Stafanger et al. 1988; Stafanger and Koch 1989; Tepel et al. 2000, 2003; Tepel and Zidek 2001; Tossios et al. 2003; Todisco et al. 1985; Verstraeten 1979; Van Schooten et al. 2002; Walters et al. 1986; Watt et al. 2002; Wiklund et al. 1996; Yalcin et al. 2002). Collectively, these findings suggest that cysteine/GSH deficiency contributes to the pathophysiology of a wide range of diseases and that treatment of this deficiency may be important in these diseases.
GSH is a central component of the oxidative-reductive (redox) apparatus of every cell. One of its key functions is to combine with, and thereby inactivate (detoxify), reactive oxygen species (ROS), other oxidative molecules, and certain drugs, exogenous chemicals, and toxins. Because GSH is depleted in these reactions, it must continually be replenished to maintain cell and organ viability and to support normal cellular functions. Drug intoxications resulting in severe GSH depletion, notably APAP overdose, cause extensive hepatic injury if treatment to replenish GSH is not initiated before GSH stores are depleted to below-critical protective levels.
Synthesis of GSH requires cysteine, a conditionally essential amino acid that must be obtained from dietary sources or by conversion of dietary methionine via the cystathionase pathway. If the supply of cysteine is adequate, normal GSH levels are maintained. In contrast, if supplies of cysteine are inadequate to maintain GSH homeostasis in the face of increased GSH consumption, GSH depletion occurs.
GSH depletion impacts a wide variety of cellular processes, ranging from DNA synthesis and gene expression to sugar metabolism and lactate production. The pleiotropic activity of this key intracellular molecule, which arose very early in evolution, derives from its participation in the energy economy and the synthetic and catabolic activities of virtually all cells. In higher animals, it also participates in regulating the expression or activity of extracellular molecules, including many of the cytokines and adhesion molecules implicated in inflammatory reactions and other disease processes.
Acute GSH depletion causes severe—often fatal—oxidative and/or alkylation injury. This injury can be prevented (e.g., in APAP overdose) by rapid treatment with NAC, an efficient nontoxic source of cysteine, which is able to replenish hepatocellular GSH. Chronic or slowly arising GSH deficiency due to administration of GSH-depleting drugs, or to diseases and conditions that deplete GSH, can be similarly debilitating (Taniguchi et al. 1989).
In this chapter, we first review evidence for a cysteine/GSH deficiency in a variety of disease settings and consider the biochemical mechanisms through which this deficiency, and its correction, can impact disease processes. We then consider findings from a large series of RPCT in which the effectiveness of NAC treatment has been investigated and discuss this in terms of cysteine/GSH replenishment.
3.2 GSH Deficiency and Disease
A role for GSH deficiency in the clinical manifestations of a broad spectrum of diseases and conditions is suggested either by the direct documentation of low GSH levels in these conditions or by the demonstration of significant improvement in patient condition following NAC administration. Over 70 RPCTs demonstrate beneficial effects of NAC treatment (Online Table 20.2) (Keays et al. 1991; Bromley et al. 1995; Estensen et al. 1999; Reinhart et al. 1995; Ardissino et al. 1997; Badaloo et al. 2002; Boesgaard et al. 1992; Horowitz et al. 1988a, b; Spies et al. 1996, 1994; Svendsen et al. 1989; Andersen et al. 1995; Eren et al. 2003; Fischer et al. 2004; Tossios et al. 2003; Altomare et al. 1996; Diaz-Sandoval et al. 2002; Drager et al. 2004; Efrati et al. 2003; Kay et al. 2003; MacNeill et al. 2003; Shyu et al. 2002; Tepel et al. 2000, 2003; Tepel and Zidek 2001; De Mattia et al. 1998a, b; Fulghesu et al. 2002; Pace et al. 2003; Ratjen et al. 1985; Stafanger et al. 1988; Stafanger and Koch 1989; Scholze et al. 2004; Wiklund et al. 1996; Aylward et al. 1980; Boman et al. 1983; Brocard et al. 1980; Dueholm et al. 1992; Evald et al. 1989; Ferrari 1980; Ferrari and Spinelli 1980; Grassi 1980; Grassi and Morandini 1976; Hansen et al. 1994; Heinig et al. 1985; Jackson et al. 1984; McGavin 1985; Parr and Huitson 1987; Rasmussen and Glennow 1988; Kasielski and Nowak 2001; Verstraeten 1979; Olivieri et al. 1985; Van Schooten et al. 2002; Todisco et al. 1985; Bernard et al. 1997; De Backer et al. 1996; Suter et al. 1994; Rank et al. 2000; Spapen et al. 1998; De Flora et al. 1997; Akerlund et al. 1996; Breitkreutz et al. 2000b; De Rosa et al. 2000; Herzenberg et al. 1997; Spada et al. 2002; Watt et al. 2002; Adair et al. 2001; Hauer et al. 2003; Ovesen et al. 2000; Walters et al. 1986; Yalcin et al. 2002; Bowles and Goral 1985) in diseases and conditions that include systemic inflammatory response syndrome (SIRS), acute respiratory distress syndrome (ARDS), chronic lung disease (CLD), chronic obstructive pulmonary disease (COPD), neurodegenerative disease, cardiovascular disease, alcoholism, infectious disease (e.g., HIV-1 infection and chronic hepatitis), hepatic and renal failure, diabetes, malnutrition, and certain autoimmune diseases.
The mechanisms that underlie the development of GSH deficiency in disease are reasonably well understood, at least in some instances. A wide variety of inflammatory and metabolic stimuli common during active disease increase the production of intracellular oxidants. In addition, neutrophils and other cells present at sites of inflammation release oxidants (reactive oxygen and nitrogen intermediates) that enter other cells and add to the internal oxidant burden. GSH provides the main defense against toxic oxidative intermediates by reducing and thereby inactivating them. However, in so doing, GSH is oxidized to GSH disulfide (GSSG). GSSG is then either rapidly reduced to GSH by GSSG reductase and NADPH or is excreted from the cell and only in part recovered from the circulation.
Factors that may contribute to GSH deficiency include GSH losses that occur when GSH is enzymatically conjugated to exogenous chemicals (drugs, dietary components, and toxins) and excreted from the cell as GSH or acetylcysteine mercapturates (conjugates). In addition, disease processes may decrease the cellular uptake or synthesis of cysteine or cystine, increase GSH efflux (Abrams et al. 1995), or increase the loss of cysteine/GSH sulfur due to accelerated oxidation to the final oxidized forms (sulfate and taurine) (Hortin et al. 1994; Breitkreutz et al. 2000a). Because a balance between cysteine supply and GSH utilization must be maintained, if oxidant production or levels of substrate for GSH conjugation are high and cysteine supplies for GSH replenishment become limiting, severe GSH deficiency may occur.
Importantly, there are significant potential iatrogenic contributions to GSH depletion. Inadvertent treatment with higher doses of APAP than patients can tolerate is perhaps the most common. This can be particularly dangerous for patients with conditions in which GSH depletion tends to occur as a consequence of the disease process or following treatment with drugs that are detoxified by GSH. In addition, long-term maintenance on parenteral nutrition may result in GSH depletion since parenteral nutrition formulations are not necessarily designed to provide adequate cysteine equivalents to meet the metabolic needs of diseased patients. In the absence of adequate attention to maintenance of adequate cysteine supplies, physicians and other caregivers can inadvertently contribute to GSH deficiency.
Patient behavior may also result in the development of GSH deficiency. Chronic over-consumption of alcohol is well known to deplete GSH in certain tissues, particularly the liver, and thus to render patients susceptible to APAP toxicity at doses well below those that cause toxicity in healthy individuals. Indeed, the FDA has issued a warning to this effect (www.fda.gov/ohrms/dockets/ac/02/briefing/3882b1.htm). However, chronic consumption of APAP or other GSH-depleting drugs, even well below toxic dose levels, can gradually deplete GSH to the point where these drugs elicit toxicity. Such practices become more dangerous if patients are malnourished or are GSH deficient for other reasons.
In summary, GSH deficiency occurs more frequently than previously suspected. GSH is readily replenished by de novo synthesis as long as sufficient supplies of cysteine are available, either directly from dietary sources or indirectly by conversion of dietary methionine. However, failure to obtain sufficient dietary cysteine to replace that lost when GSH is oxidized or conjugated to drugs or exogenous chemicals results in a deficiency in cysteine and/or GSH that may necessitate pharmacological intervention.
3.3 Dietary Sources of Cysteine
Cysteine utilized in the body is derived from dietary cysteine and methionine, sulfur-containing amino acids (SAAs) that are largely obtained from digested protein. Since mammals obtain cysteine both directly from the diet and by degradation of dietary methionine, the normal cysteine requirement can be satisfied from dietary sources. However, as indicated above, an additional source of cysteine may be required when cysteine loss (e.g., via GSH loss) outstrips the usual dietary supply.
Requirements for SAAs in humans are based upon nitrogen and SAA balance studies conducted with healthy individuals. The average American diet contains about 100 g of protein daily, greater than half of which is animal protein with a relatively high content of SAAs. The recommended daily allowance (RDA) for SAAs for an adult male is about 1 g (200 mg of methionine and an additional 810 mg of methionine that can be replaced by an equivalent amount of cysteine). A healthy, well-fed person will often consume greater than twice the SAA RDA. However, poor appetite and/or a tendency to select fresh food with low SAA content or bioavailability (Hitchins et al. 1989) or processed food depleted of SAAs (Volkin and Klibanov 1987; Schnackenberg et al. 2009; Briganti et al. 2008) can result in cysteine deficiency even in otherwise healthy people. Furthermore, as evidence here indicates, the need for SAAs can be substantially increased in many disease states.
The limited ability of the body to store amino acids is an additional problem. The human liver does contain a reservoir of cysteine (about 1 g) that is largely present in GSH. Since this amount approximates the daily SAA requirement, it provides only a short-term source to maintain a stable cysteine supply despite intermittent methionine and cysteine consumption. Under conditions of excessive cysteine requirements or deficient cysteine/methionine consumption, GSH is released from skeletal muscle and other tissues to supply cysteine. This results in decreased antioxidant and detoxification functions throughout the body. Consequently, even short-term inadequate intake of SAAs can pose a risk to individuals who may consume adequate amounts most of the time (Larsen and Fuller 1996; Shriner and Goetz 1992).
3.4 Mechanisms that May Mediate the Clinical Effects of Cysteine/GSH Deficiency
GSH has multiple roles in cells, ranging from neutralization of ROS to acting as a coenzyme in a variety of metabolic processes. The widespread participation of GSH in biochemical reactions of importance to cell growth, differentiation, and function offers mechanistic insights into how interfering with GSH homeostasis could influence the course of varied disease processes. A full discussion of the preclinical data bearing on these issues is beyond the scope of this review. However, to provide a mechanistic context for the clinical findings we discuss, we have summarized some of the key processes regulated by GSH in the following section.
3.4.1 Oxidative Reactions
In its best-known role, GSH participates in enzyme-mediated reactions to neutralize ROS, preventing the accumulation of ROS damage to DNA, proteins, and lipids. Glutathione peroxidases play a key role in this process by catalyzing the reaction of GSH with peroxides, including hydrogen peroxide and lipid peroxides. Thus, decreasing GSH can sharply augment oxidative damage and result in cell death or loss of function.
3.4.2 DNA Synthesis
Low GSH availability can impair DNA synthesis since GSH acts (via thioredoxin) as a coenzyme for ribonucleotide reductase, an enzyme required for the synthesis of DNA (Holmgren 1985, 1989; Zhong et al. 2000a).
3.4.3 Gene Expression and Signal Transduction
GSH has been shown to regulate or influence the expression of several genes, notably inflammatory genes under the control of transcription factor nuclear factor kappa B (NF-κB) and activator protein 1 (AP-1), even in settings where there is no marked overproduction of ROS. In addition, GSH has been shown to regulate T-cell signaling by controlling phosphorylation of phospholipase C γ 1 (PLCg1), which is required to stimulate the calcium flux that occurs early in the T-cell receptor-signaling cascade (Kanner et al. 1992a, b, c; Kanner and Ledbetter 1992; Flescher et al. 1994). Importantly, GSH has also been shown to regulate the expression of vascular cell adhesion molecule-1 (VCAM-1) on vascular endothelial cells, one of the early features in the pathogenesis of atherosclerosis and other inflammatory diseases (Ahmad et al. 2002; De Mattia et al. 1998a, b; Marui et al. 1993; Schmidt et al. 1995; Weigand et al. 2001).
3.4.4 Enzymes and Protein Functions
GSH regulates the activity of enzymes and other intracellular molecules by posttranslational modifications (glutathionylations) that control the oxidation state of protein-SH groups. When intracellular GSH is at its normal level for a particular cell type in a healthy individual, most of the free protein thiol groups are reduced, i.e., are present as protein-SH. In contrast, when GSH levels are low and/or GSSG levels are increased, GSH is reversibly coupled to many free thiols to create mixed disulfides (protein-S-S-G) (Ghezzi et al. 2002). These S-glutathionylated proteins, which may be functionally altered, then persist as such until GSH levels return to normal.
By controlling the activities of a series of enzymes and other intracellular proteins, glutathionylation can rapidly and reversibly alter the metabolic status of cells in response to changes in the redox environment. For example, glutathionylation has been shown to regulate actin polymerization (Wang et al. 2001), to inhibit the activity of several key enzymes (including glyceraldehyde-3-phosphate dehydrogenase, carbonic anhydrase, and protein tyrosine phosphatase), and to activate or stabilize other enzymes (including HIV-1 protease and the NF-ĸB transcription factor (Pineda-Molina et al. 2001)). Nitrosylation of protein thiols has similarly been shown to increase under oxidative conditions (Galli et al. 2002; Choudhary and Dudley 2002; Estevez and Jordan 2002; Yang et al. 2002) and to alter functions of key enzymes (Arnelle and Stamler 1995) and other molecules (Gow et al. 2002; Marshall et al. 2002). Thus, both glutathionylation and nitrosylation are of central importance to mechanisms through which cysteine/GSH deficiency may impact cell, and hence organ, function.
As indicated above, these types of posttranslational modifications are highly sensitive to shifts in the intracellular redox balance. They are rapidly initiated when GSH is depleted and rapidly reversed when GSH is replenished. As such, they provide the kind of flexible response to oxidative stress necessary for organisms living in an oxidative environment. However, at the extreme, they may underlie some of the pathologic changes that occur when chronic cysteine/GSH deficiency occurs in disease.
3.4.5 Glutaredoxin and Thioredoxin
Glutaredoxin (Grx) and thioredoxin (Trx) belong to the two major oxidoreductase enzyme families, which take electrons from GSH and NADPH respectively (Zhong et al. 2000a; Holmgren 1989; Cotgreave et al. 2002; Nakamura et al. 2001; Vlamis-Gardikas and Holmgren 2002). Trx and Grx interact with proteins to regulate functional activity, both directly and via glutathionylation. Intracellular GSH and GSSG levels play a major role in this regulation. The activity of Grx is directly regulated by the amount of intracellular GSH and GSSG, which controls the status of the Grx active site. The active sites in Trx (Cys-Gly-Pro-Cys) and Grx (Cys-Pro-Tyr-Cys) contain a dithiol that can be oxidized when GSH levels are low (or GSSG levels increase) to form an internal disulfide between the two cysteine residues or a mixed disulfide in which GSH is bound to one or both cysteine residues in the active site.
Formation of the Grx mixed disulfide (Casagrande et al. 2002; Cotgreave et al. 2002; Ghezzi et al. 2002) represents a special case of protein glutathionylation since it arms the Grx for glutathionylation of other proteins. Although Trx can also be glutathionylated (Casagrande et al. 2002), current data indicate that glutathionylation is mainly mediated by the Grx mixed disulfide (Daily et al. 2001; Shenton et al. 2002; Song et al. 2002). Oxidation of Grx and Trx active sites can also regulate Trx or Grx functions mediated by direct binding to key intracellular proteins. For example, under reducing conditions, Trx and Grx protect cells from apoptosis by binding to and inactivating apoptosis signaling kinase I (Song et al. 2002; Saitoh et al. 1998), whereas this binding is blocked, and apoptosis induction proceeds at low GSH levels (and/or high GSSG levels; Arner and Holmgren 2000).
3.4.6 Selenoenzymes
Decreasing GSH increases the intracellular redox potential of the GSH/GSSG redox couple and puts an additional burden on the Trx-Trx reductase system. This may be quite important in patients who have low selenium levels, since human Trx reductases are selenoenzymes with an essential selenocysteine residue in the active site (Arner and Holmgren 2000; Gladyshev et al. 1996a, b; Sandalova et al. 2001; Zhong et al. 2000a, b; Zhong and Holmgren 2000). Cysteine/GSH deficiency in these patients, in whom Trx reductase activity is compromised, may make them particularly susceptible to cell damage under oxidative stress. Thus, cysteine/GSH deficiency can impact cell and organ function through multiple pathways operating at the same or different sites, depending on the underlying mechanisms responsible for depleting GSH. The fact that multiple different pathways are affected explains why the effects of cysteine/GSH deficiency can affect many diseases and why cysteine/GSH deficiency has not been readily recognizable as a single clinical entity in the past.
3.5 N-Acetylcysteine (NAC) Treatment to Relieve Cysteine/GSH Deficiency
Clinical experience in the treatment of APAP toxicity has established that rapid administration of NAC, an essentially nontoxic cysteine source, restores normal GSH levels in solid tissues and the systemic circulation and thus prevents the potentially lethal consequences of severe cysteine/GSH deficiency induced by APAP overdose. In addition to this well-known role for NAC, NAC treatment has been shown to be clinically beneficial in a wide variety of diseases and conditions. In fact, over 70 RPCTs (Online Table 20.2) have reported beneficial effects of NAC treatment. Collectively, these studies demonstrate that cysteine/GSH deficiency is an important emerging clinical entity and that NAC administration offers an effective method for treating this deficiency.
Although various forms of cysteine and its precursors have been used as nutritional and therapeutic sources of cysteine, NAC is the most widely used and extensively studied. NAC is about ten times more stable than cysteine and much more soluble than the stable cysteine disulfide, cystine. l-2-oxothiazolidine-4-carboxylate (procysteine/OTC) has also been used effectively in some studies (Aaseth and Stoa-Birketvedt 2000) as have GSH and GSH monoethyl ester (Meister et al. 1986). In addition, dietary methionine is an effective source of cysteine, as is S-adenosylmethionine (referred to either as SAM or SAM-e) (Castagna et al. 1995). We focus on NAC in this review because NAC is the cysteine source used for correcting cysteine/GSH deficiency in most studies and because NAC is already approved for therapeutic use for treatment of APAP overdose and as a mucolytic agent in cystic fibrosis.
Surprisingly, given the diverse roles that GSH plays in cellular physiology and regulation of enzyme activity and protein function (see above), GSH deficiency has mainly been discussed from a clinical perspective in terms of the loss of intracellular protection against oxidative stress. Similarly, NAC is principally considered to be an antioxidant rather than a source of cysteine for GSH replenishment. However, while antioxidants such as vitamins E and C can spare GSH under conditions of oxidative stress, GSH loss due to oxidative or detoxifying reactions can only be offset by GSH resynthesis, which requires a cysteine source.
In addition to providing the cysteine necessary to replenish GSH, NAC administration improves the cysteine supply for protein synthesis and metabolic purposes. When administered intravenously, it also appears for a short period of time at high levels in blood and can react directly with oxidants and nitric oxide derivatives. However, when administered orally (as in most of the studies), it is rapidly converted by first-pass metabolism to cysteine, which is either incorporated into GSH in the liver or released into the blood in a regulated manner. Thus, orally administered NAC appears in the circulation only transiently and at only minimal levels. Hence, it is effective largely via its ability to increase cysteine supplies and thereby facilitate the GSH replenishment.
In the sections that follow, we discuss examples of RPCTs (Online Table 20.2) which have examined the outcomes of NAC therapy in various medical disorders. We also discuss selected findings from observational studies (Online Table 20.3) that further illuminate clinical aspects of cysteine/GSH deficiency.
3.5.1 Acetaminophen Toxicity
APAP overdose is a well-known cause of fulminant hepatic failure. In fact, APAP overdose and idiosyncratic drug reactions have now replaced viral hepatitis as the most frequent causes of acute liver failure in the United States (Ostapowicz and Lee 2000). The toxicity of APAP is due to depletion of GSH in hepatocytes (Mitchell et al. 1974, 1981; Peterson and Rumack 1978; Lauterburg et al. 1983; Smilkstein et al. 1988; Ostapowicz et al. 2002). NAC is extremely effective in preventing liver damage due to APAP toxicity. NAC administered promptly and at a sufficient dose is the standard of care for treatment of APAP poisoning (Mitchell et al. 1974; Lyons et al. 1977; Prescott et al. 1977; Peterson and Rumack 1977a, b, 1978; Marquardt 1977; Maurer and Zeisler 1978; Macy 1979; Stewart et al. 1979; Bailey 1980; Black 1980; Sellers and Freedman 1981; Rumack et al. 1981; Prescott and Critchley 1983; Miller and Rumack 1983; Rumack 1984, 1986, 2002; Davis 1986; Larrauri et al. 1987; Slattery et al. 1987, 1989; Smilkstein et al. 1988, 1991; Burgunder et al. 1989; Beckett et al. 1990, 1985; Harrison et al. 1990; Keays et al. 1991; Bray et al. 1991; Winkler and Halkin 1992; Lee 1993, 1995, 1996; Larsen and Fuller 1996; De Roos and Hoffman 1996; Perry and Shannon 1998; Salgia and Kosnik 1999; Ammenti et al. 1999; Buckley et al. 1999; Broughan and Soloway 2000; Kearns et al. 2000; Woo et al. 2000; Amirzadeh and McCotter 2002; Schmidt et al. 2002; Jones 2002; Kearns 2002; Peterson et al. 1998) and can improve survival (Harrison et al. 1990) and cardiovascular function (Harrison et al. 1991) in those already with hepatic failure.
Interestingly, although the acute dose of APAP likely to cause severe liver toxicity is well established for healthy individuals (Peterson and Rumack 1978), under conditions in which GSH levels are compromised, doses of APAP that are within the usual prescribed range can cause hepatic injury (Peterson and Rumack 1978; Larsen and Fuller 1996). Thus, usage of APAP and other GSH-depleting drugs may be quite important to overall pathology in diseases and conditions where GSH deficiency is known to occur.
This is especially important in patients with chronic alcohol consumption (Bray et al. 1991; Salgia and Kosnik 1999) because they often have lower GSH levels. In such patients, doses of APAP below those usually considered toxic could deplete GSH below the critical threshold for hepatocellular necrosis (Lauterburg and Velez 1988). Thus, it has been suggested that patients with chronic alcoholism and suspected APAP poisoning should be treated with NAC regardless of risk estimation (Johnston and Pelletier 1997; Ozaras et al. 2003; Moss et al. 2000). This has prompted the FDA to a special warning for individuals with chronic alcohol use in regard to APAP use.
3.5.2 Gastrointestinal Disease
Several studies have demonstrated GSH depletion in children with the edematous syndromes of protein-energy malnutrition (PEM), kwashiorkor, and marasmic kwashiorkor (Badaloo et al. 2002; Golden and Ramdath 1987; Jackson 1986; Reid et al. 2000). Children with edematous PEM have biomarkers of oxidant damage (Lenhartz et al. 1998; Fechner et al. 2001). The observation that biomarkers of oxidant damage normalize as soon as clinical signs and symptoms resolve (Lenhartz et al. 1998) suggests that oxidant damage plays an important role in the pathogenesis of the disease.
In a study of children with edematous PEM, Jahoor and colleagues showed that RBC GSH depletion is due to a slower rate of GSH synthesis secondary to inadequate cysteine availability (Reid et al. 2000). In another study of children with edematous PEM, Jahoor and colleagues demonstrated that GSH synthesis rate and concentration can be restored during the early phase of nutritional rehabilitation if diets are supplemented with NAC (Badaloo et al. 2002). The observation that edema is lost at a faster rate by the group whose GSH pools were restored early with NAC suggests that early restoration of GSH homeostasis accelerates recovery. This possibility is supported by another study showing that increases in GSH levels in children with kwashiorkor are associated with recovery (Fechner et al. 2001).
These findings also raise the question of whether the modest malnutrition common in elderly people, who also frequently have low GSH levels (Anderson et al. 1993, 2001), puts the elderly at risk for developing clinically significant cysteine/GSH deficiency and hence at increased risk of hepatic and other tissue injuries associated with consumption of GSH-depleting pharmaceuticals such as APAP.
3.5.3 Kidney Transplantation
Delayed graft function (DGF) after kidney transplantation is probably in large part caused by production of ROS following reperfusion of the transplant organ after a period of warm and cold ischemia. In general, these reactive molecules are detoxified by GSH-dependent mechanisms, including conjugation to GSH by a family of GSH-S-transferase (GST) enzymes, some of which are expressed in large quantity in the proximal tubule of the kidney (Davies et al. 1995). In an observational study of 229 kidney transplant recipients, donor (but not recipient) GST M1B polymorphism was associated with significantly lower rates of DGF after transplantation (Akgul et al. 2012).
3.5.4 Diabetes Mellitus
Three RPCTs demonstrate beneficial effects of NAC treatment in insulin-related disease (Online Table 20.2d). One study demonstrates that oral administration of NAC to patients with non-insulin-dependent diabetes mellitus reverses the elevation of soluble vascular cell adhesion molecule-1 (De Mattia et al. 1998b), a substance that promotes accumulation of macrophages and T lymphocytes at sites of inflammation and increases progression of vascular damage (Marui et al. 1993; Schmidt et al. 1995). A second placebo-controlled study by the same group shows that intravenous GSH infusion significantly increases both RBC GSH/GSSG redox ratio and total glucose uptake in these patients and suggests that abnormal intracellular GSH redox status plays an important role in reducing insulin sensitivity (De Mattia et al. 1998a). Consistent with these findings, in an ongoing study in type 2 diabetics, Jahoor and colleagues have demonstrated that 2 weeks of dietary supplementation with NAC elicited significant increases in both RBC GSH concentration and synthesis, suggesting that positive clinical effects of NAC are mediated through improved GSH availability (McKay et al. 2000).
3.5.5 Metabolic and Genetic Disease
Genetic defects that impair GSH synthesis or homeostasis are well known (Ristoff and Larsson 2002). The most common defect affects GSH synthetase (GS) and has a wide range of disease manifestations, including hemolytic anemia, progressive neurological symptoms, metabolic acidosis, and, in the most severe form, death during the neonatal period. Data from a small observational study suggests that early supplementation with Vitamins C and E may improve long-term outcome in these patients (Ristoff et al. 2001).
3.5.6 Systemic Inflammatory Response Syndrome
Five of seven RPCTs showed a beneficial effect of NAC as an adjunct therapy for acute lung injury and end-organ failure. These studies indicate that oxidative stress and cysteine/GSH depletion play a major role in inflammation leading to capillary leak syndromes and end-organ failure (De Flora et al. 1997; Suter et al. 1994; Rank et al. 2000). These study show that NAC: (a) decreases the cytotoxic effects of TNF-α and other inflammatory cytokines (Zimmerman et al. 1989), (b) decreases neutrophil elastase production in acute lung injury (Borregaard et al. 1987; De Backer et al. 1996; Laurent et al. 1996; Eklund et al. 1988; Moriuchi et al. 1998), and (c) increases neutrophil protection and decreases mortality in septic shock (Villa et al. 2002).
3.5.7 HIV Disease
A broad series of studies clearly demonstrates GSH levels in RBCs, lymphocytes, and other peripheral blood mononuclear cells progressively decrease as HIV disease advances (De Rosa et al. 2000; Herzenberg et al. 1997; Akerlund et al. 1996; Droge and Breitkreutz 1999; Clotet et al. 1995; Spada et al. 2002; Verhagen et al. 2001). In addition, careful pharmacokinetic studies demonstrate that the low GSH in HIV-infected individuals is due to limited availability of sufficient cysteine to maintain cellular GSH homeostasis (Droge et al. 1991; Roederer et al. 1990). In fact, a massive peripheral tissue catabolism of sulfur-containing peptides and amino acids has been observed in HIV patients (Hortin et al. 1994; Breitkreutz et al. 2000a).
Five of six RPCTs show beneficial effects of NAC treatment in HIV infection. Several trials collectively demonstrated that NAC administration to HIV-infected subjects with low GSH levels replenishes lymphocyte and erythrocyte GSH (Online Table 20.2g) (De Rosa et al. 2000; Breitkreutz et al. 2000b). Importantly, one of these studies demonstrates that NAC treatment significantly improves T-cell function (Breitkreutz et al. 2000b). This finding supports the idea that cysteine/GSH deficiency contributes to the immunodeficiency in HIV-infected individuals and plays an important and reversible role in the functional impairment of those T cells that are still present at later stages of HIV disease.
Cysteine/GSH deficiency may also contribute to the failure of the innate immune system and the development of opportunistic infections in the final stages of HIV disease. Observational studies have shown that HIV-infected individuals with low CD4 T-cell counts and low cellular and systemic GSH levels frequently have elevated blood levels of Trx, which is an effective chemokine (Bertini et al. 1999). In mice, circulating Trx (like other chemokines) blocks neutrophil migration to infection sites and hence interferes with innate defense against invading pathogens (Villa et al. 2002). Similar interference may occur in HIV infection, since the survival of infected individuals with Trx levels above the normal range is significantly decreased compared to survival of subjects with Trx levels in the normal range (Ghezzi et al. 2002). Since NAC treatment lowers Trx levels (Nakamura et al. 2001, 2002), this may contribute to the observed association between NAC ingestion and prolonged survival in HIV disease (Roederer et al. 1992; De Rosa et al. 2000; Akerlund et al. 1996; Spada et al. 2002).
The improvement in T-cell function observed in HIV-infected subjects treated with NAC (Breitkreutz et al. 2000b) suggests that NAC treatment may be a useful adjunct in HIV vaccination. In addition, this improvement provides a rationale for the strong associations observed between low GSH levels and decreased survival in HIV infection (Herzenberg et al. 1997) and between NAC administration and improved survival in an open-label NAC study (Huengsberg et al. 1998).
3.5.8 Otic Disease
Preclinical studies point to the importance of oxidative stress and GSH depletion in the genesis of noise and toxin-induced hearing loss (Kopke et al. 1999, 2001). Medications with inner ear toxicity such as aminoglycoside antibiotics and the chemotherapy agent cisplatin damage the cochlea through the generation of oxygen free radicals. Hearing loss and cochlear damage associated with administration of these compounds have been shown, in animal models, to be greatly reduced by administration of both NAC and methionine (Hoffer et al. 2001; Kopke et al. 2000; Sha and Schacht 2000). Similarly, studies with animal models show that permanent cochlear damage due to acute acoustic overexposure, which induces ischemia reperfusion, glutamate excitotoxicity, free radical generation, and GSH depletion (Kopke et al. 1999, 2000, 2001, 2002), can be almost completely prevented by systemic administration of NAC or methionine (Kopke et al. 2000, 2002).
4 Summary
The evidence reviewed here reveals cysteine/GSH deficiency as an emerging clinical entity. The manifestations of this deficiency may vary in different disease settings, as may the biochemical mechanisms that mediate its effects. However, they are united by a common positive response to NAC therapy in RPCTs (Online Table 20.2). The studies we have reviewed collectively argue for consideration of cysteine/GSH deficiency as a significant and treatable clinical entity.
Surprisingly, given the diverse roles that GSH plays in cellular physiology and regulation of enzyme activity and protein function, the consequences of low GSH levels have mainly been discussed from a clinical perspective in terms of the loss of protection against intracellular oxidative stress. However, while antioxidants such as vitamins E and C can spare GSH under conditions of oxidative stress, GSH loss can only be offset by GSH resynthesis, indicating a central role for this molecule over and above its ability to counteract the effects of intracellular oxidants.
Similarly, although NAC is a well-known source of cysteine for GSH replenishment in APAP toxicity, it is principally cast as an antioxidant in other settings. By and large, physicians and the lay public tend to equate NAC with vitamins C and E and other antioxidants. Like GSH, NAC can serve as an antioxidant. However, while other antioxidants can replace NAC and GSH in this role, only NAC or another cysteine source can provide the raw material necessary to replenish GSH and enable GSH-dependent biochemical reactions.
We have pointed out that physicians may find NAC administration useful as adjunct therapy for diseases and conditions in which cysteine/GSH deficiency is likely to play a role. The positive findings in the RPCTs we have discussed support this argument. However, the absence of large multicenter trials testing NAC in various settings leaves this as an open question. The recognition that cysteine/GSH deficiency is an important clinical entity will encourage support for such trials.
In the meantime, the findings we have discussed suggests that patients with diseases or conditions in which cysteine/GSH deficiency has been demonstrated may be well advised to avoid unnecessary exposures to medications that may exacerbate GSH depletion. In fact, when advising such patients, it seems reasonable for physicians to emphasize that alcohol usage be kept at modest levels and that APAP usage should be kept strictly within the recommended dosing.
The availability of OTC NAC, and the low toxicity of this cysteine prodrug in situations where it has been tested, opens the possibility of patient- or physician-initiated therapy. However, if such therapy is elected, we suggest that the NAC preparation(s) used be prepared under Good Manufacturing Practice conditions and packaged to prevent oxidation of the product.
References
Aaseth J, Stoa-Birketvedt G (2000) Glutathione in overweight patients with poorly controlled type 2 diabetes. J Trace Elem Exp Med 13(1):105–111
Abrams D, Cotton D, Mayer K (1995) AIDS/HIV treatment directory, vol 7 #4. American Foundation for AIDS Research (AmFAR), Rockville, MD
Adair JC, Knoefel JE, Morgan N (2001) Controlled trial of N-acetylcysteine for patients with probable Alzheimer’s disease. Neurology 57(8):1515–1517
Agusti AG, Togores B, Ibanez J, Raurich JM, Maimo A, Bergada J, Marse P, Jorda R (1997) Effects of N-acetylcysteine on tissue oxygenation in patients with multiple organ failure and evidence of tissue hypoxia. Eur Respir J 10(9):1962–1966
Ahmad M, Zhang Y, Papharalambus C, Alexander RW (2002) Role of isoprenylcysteine carboxyl methyltransferase in tumor necrosis factor-alpha stimulation of expression of vascular cell adhesion molecule-1 in endothelial cells. Arterioscler Thromb Vasc Biol 22(5):759–764
Ahola T, Lapatto R, Raivio KO, Selander B, Stigson L, Jonsson B, Jonsbo F, Esberg G, Stovring S, Kjartansson S, Stiris T, Lossius K, Virkola K, Fellman V (2003) N-acetylcysteine does not prevent bronchopulmonary dysplasia in immature infants: a randomized controlled trial. J Pediatr 143(6):713–719
Akerlund B, Jarstrand C, Lindeke B, Sonnerborg A, Akerblad A-C, Rasool O (1996) Effect of N-acetylcysteine (NAC) treatment on HIV-1 infection: a double-blind placebo-controlled trial. Eur J Clin Pharmacol 50(6):457–461
Akerlund B, Tynell E, Bratt G, Bielenstein M, Lidman C (1997) N-acetylcysteine treatment and the risk of toxic reactions to trimethoprim-sulphamethoxazole in primary Pneumocystis carinii prophylaxis in HIV-infected patients. J Infect 35(2):143–147
Akgul SU, Oguz FS, Caliskan Y, Kekik C, Gurkan H, Turkmen A, Nane I, Aydin F (2012) The effect of glutathione S-transferase polymorphisms and anti-GSTT1 antibodies on allograft functions in recipients of renal transplant. Transplant Proc 44(6):1679–1684. https://doi.org/10.1016/j.transproceed.2012.04.004
Allaqaband S, Tumuluri R, Malik AM, Gupta A, Volkert P, Shalev Y, Bajwa TK (2002) Prospective randomized study of N-acetylcysteine, fenoldopam, and saline for prevention of radiocontrast-induced nephropathy. Catheter Cardiovasc Interv 57(3):279–283. https://doi.org/10.1002/ccd.10323
Allard JP, Aghdassi E, Chau J, Tam C, Kovacs CM, Salit IE, Walmsley SL (1998) Effects of vitamin E and C supplementation on oxidative stress and viral load in HIV-infected subjects. AIDS 12(13):1653–1659
Altomare E, Colonna P, Dagostino C, Castellaneta G, Vendemiale G, Grattagliano I, Cirelli F, Bovenzi F, Colonna L (1996) High-dose antioxidant therapy during thrombolysis in patients with acute myocardial infarction. Curr Ther Res 57(2):131–141
Altomare E, Vendemiale G, Albano O (1988) Hepatic glutathione content in patients with alcoholic and non alcoholic liver disease. Life Sci 43:991–998
Amirzadeh A, McCotter C (2002) The intravenous use of oral acetylcysteine (mucomyst) for the treatment of acetaminophen overdose. Arch Intern Med 162(1):96–97
Ammenti A, Ferrante R, Spagna A (1999) Renal impairment without hepatic damage after acetaminophen overdose. Pediatr Nephrol 13(3):271–272
Andersen LW, Thiis J, Kharazmi A, Rygg I (1995) The role of N-acetylcystein administration on the oxidative response of neutrophils during cardiopulmonary bypass. Perfusion 10(1):21–26
Anderson BB, Giuberti M, Perry GM, Salsini G, Casadio I, Vullo C (1993) Low red blood cell glutathione reductase and pyridoxine phosphate oxidase activities not related to dietary riboflavin: selection by malaria? Am J Clin Nutr 57(5):666–672
Anderson RA, Roussel AM, Zouari N, Mahjoub S, Matheau JM, Kerkeni A (2001) Potential antioxidant effects of zinc and chromium supplementation in people with type 2 diabetes mellitus. J Am Coll Nutr 20(3):212–218
Andrews NP, Prasad A, Quyyumi AA (2001) N-acetylcysteine improves coronary and peripheral vascular function. J Am Coll Cardiol 37(1):117–123
Angulo P, Lindor KD (2001) Treatment of nonalcoholic fatty liver: present and emerging therapies. Semin Liver Dis 21(1):81–88
App EM, Baran D, Dab I, Malfroot A, Coffiner M, Vanderbist F, King M (2002) Dose-finding and 24-h monitoring for efficacy and safety of aerosolized Nacystelyn in cystic fibrosis. Eur Respir J 19(2):294–302
Ardissino D, Merlini PA, Savonitto S, Demicheli G, Zanini P, Bertocchi F, Falcone C, Ghio S, Marinoni G, Montemartini C, Mussini A (1997) Effect of transdermal nitroglycerin or N-acetylcysteine, or both, in the long-term treatment of unstable angina pectoris. J Am Coll Cardiol 29(5):941–947
Arnelle DR, Stamler JS (1995) NO+, NO, and NO- donation by S-nitrosothiols: implications for regulation of physiological functions by S-nitrosylation and acceleration of disulfide formation. Arch Biochem Biophys 318(2):279–285. https://doi.org/10.1006/abbi.1995.1231
Arner ES, Holmgren A (2000) Physiological functions of thioredoxin and thioredoxin reductase. Eur J Biochem 267(20):6102–6109
Aukrust P, Svardal AM, Muller F, Lunden B, Berge RK, Froland SS (1995) Decreased levels of total and reduced glutathione in CD4+ lymphocytes in common variable immunodeficiency are associated with activation of the tumor necrosis factor system: possible immunopathogenic role of oxidative stress. Blood 86(4):1383–1391
Aylward M, Maddock J, Dewland P (1980) Clinical evaluation of acetylcysteine in the treatment of patients with chronic obstructive bronchitis: a balanced double-blind trial with placebo control. Eur J Respir Dis Suppl 111:81–89
Badaloo A, Reid M, Forrester T, Heird WC, Jahoor F (2002) Cysteine supplementation improves the erythrocyte glutathione synthesis rate in children with severe edematous malnutrition. Am J Clin Nutr 76(3):646–652
Bailey BO (1980) Acetaminophen hepatotoxicity and overdose. Am Fam Physician 22(1):83–87
Bains JS, Shaw CA (1997) Neurodegenerative disorders in humans: the role of glutathione in oxidative stress-mediated neuronal death. Brain Res Rev 25(3):335–358
Banaclocha MM (2001) Therapeutic potential of N-acetylcysteine in age-related mitochondrial neurodegenerative diseases. Med Hypotheses 56(4):472–477
Banerjee BD, Seth V, Bhattacharya A, Pasha ST, Chakraborty AK (1999) Biochemical effects of some pesticides on lipid peroxidation and free-radical scavengers. Toxicol Lett 107(1–3):33–47
Barbaro G, Di Lorenzo G, Soldini M, Bellomo G, Belloni G, Grisorio B, Barbarini G (1997) Vagal system impairment in human immunodeficiency virus-positive patients with chronic hepatitis C: does hepatic glutathione deficiency have a pathogenetic role? Scand J Gastroenterol 32(12):1261–1266
Barbaro G, Di Lorenzo G, Soldini M, Parrotto S, Bellomo G, Belloni G, Grisorio B, Barbarini G (1996) Hepatic glutathione deficiency in chronic hepatitis C: quantitative evaluation in patients who are HIV positive and HIV negative and correlations with plasmatic and lymphocytic concentrations and with the activity of the liver disease. Am J Gastroenterol 91(12):2569–2573
Barditch-Crovo P, Noe D, Skowron G, Lederman M, Kalayjian RC, Borum P, Buier R, Rowe WB, Goldberg D, Lietman P (1998) A phase I/II evaluation of oral L-2-oxothiazolidine-4-carboxylic acid in asymptomatic patients infected with human immunodeficiency virus. J Clin Pharmacol 38(4):357–363
Barton AD (1974) Aerosolized detergents and mucolytic agents in the treatment of stable chronic obstructive pulmonary disease. Am Rev Respir Dis 110(6 Pt 2):104–110
Beckett GJ, Chapman BJ, Dyson EH, Hayes JD (1985) Plasma glutathione S-transferase measurements after paracetamol overdose: evidence for early hepatocellular damage. Gut 26(1):26–31
Beckett GJ, Donovan JW, Hussey AJ, Proudfoot AT, Prescott LF (1990) Intravenous N-acetylcysteine, hepatotoxicity and plasma glutathione S-transferase in patients with paracetamol overdosage. Hum Exp Toxicol 9(3):183–186
Behr J, Degenkolb B, Krombach F, Vogelmeier C (2002) Intracellular glutathione and bronchoalveolar cells in fibrosing alveolitis: effects of N-acetylcysteine. Eur Respir J 19(5):906–911
Behr J, Maier K, Degenkolb B, Krombach F, Vogelmeier C (1997) Antioxidative and clinical effects of high-dose N-acetylcysteine in fibrosing alveolitis. Adjunctive therapy to maintenance immunosuppression. Am J Respir Crit Care Med 156(6):1897–1901
Beloqui O, Prieto J, Suarez M, Gil B, Qian CH, Garcia N, Civeira MP (1993) N-acetyl cysteine enhances the response to interferon-alpha in chronic hepatitis-C: a pilot study. J Interf Res 13:279–282
Ben-Ari Z, Vaknin H, Tur-Kaspa R (2000) N-acetylcysteine in acute hepatic failure (Non-paracetamol-induced). Hepatogastroenterology 47(33):786–789
Ben-Menachem E, Kyllerman M, Marklund S (2000) Superoxide dismutase and glutathione peroxidase function in progressive myoclonus epilepsies. Epilepsy Res 40(1):33–39
Bernard GR (1990) Potential of N-acetylcysteine as treatment for the adult respiratory distress syndrome. Eur Respir J Suppl 11:496s–498s
Bernard GR, Wheeler AP, Arons MM, Morris PE, Paz HL, Russell JA, Wright PE, Bernard GR, Arons MM, Wheeler AP, Carmichael LC, Morris PE, Higgins SB, Dupont WD, Edens TR, Swindell BB, Russell JA, Paz HL, Wright PE, Steinberg KP (1997) A trial of antioxidants N-acetylcysteine and procysteine in ARDS. Chest 112(1):164–172
Bernhard MC, Junker E, Hettinger A, Lauterburg BH (1998) Time course of total cysteine, glutathione and homocysteine in plasma of patients with chronic hepatitis C treated with interferon-alpha with and without supplementation with N-acetylcysteine. J Hepatol 28(5):751–755
Bertini R, Howard OM, Dong HF, Oppenheim JJ, Bizzarri C, Sergi R, Caselli G, Pagliei S, Romines B, Wilshire JA, Mengozzi M, Nakamura H, Yodoi J, Pekkari K, Gurunath R, Holmgren A, Herzenberg LA, Ghezzi P (1999) Thioredoxin, a redox enzyme released in infection and inflammation, is a unique chemoattractant for neutrophils, monocytes, and T cells. J Exp Med 189(11):1783–1789
Bianchi G, Bugianesi E, Ronchi M, Fabbri A, Zoli M, Marchesini G (1997) Glutathione kinetics in normal man and in patients with liver cirrhosis. J Hepatol 26(3):606–613
Bibi H, Seifert B, Oullette M, Belik J (1992) Intratracheal N-acetylcysteine use in infants with chronic lung disease. Acta Paediatr 81(4):335–339
Bijlmer-Iest JC, Baart de la Faille H, van Asbeck BS, van Hattum J, van Weelden H, Marx JJ, Koningsberger JC (1992) Protoporphyrin photosensitivity cannot be attenuated by oral N-acetylcysteine. Photodermatol Photoimmunol Photomed 9(6):245–249
Black M (1980) Acetaminophen hepatotoxicity. Gastroenterology 78(2):382–392
Boccalandro F, Amhad M, Smalling RW, Sdringola S (2003) Oral acetylcysteine does not protect renal function from moderate to high doses of intravenous radiographic contrast. Catheter Cardiovasc Interv 58(3):336–341
Boesgaard S, Aldershvile J, Pedersen F, Pietersen A, Madsen JK, Grande P (1991) Continuous oral N-acetylcysteine treatment and development of nitrate tolerance in patients with stable angina pectoris. J Cardiovasc Pharmacol 17(6):889–893
Boesgaard S, Aldershvile J, Poulsen HE (1992) Preventive administration of intravenous N-acetylcysteine and development of tolerance to isosorbide dinitrate in patients with angina pectoris. Circulation 85(1):143–149
Boman G, Backer U, Larsson S, Melander B, Wahlander L (1983) Oral acetylcysteine reduces exacerbation rate in chronic bronchitis: report of a trial organized by the Swedish Society for Pulmonary Diseases. Eur J Respir Dis 64(6):405–415
Bondy SC (1992) Ethanol toxicity and oxidative stress. (Comment). Toxicol Lett 63:231–241
Boon AC, Vos AP, Graus YM, Rimmelzwaan GF, Osterhaus AD (2002) In vitro effect of bioactive compounds on influenza virus specific B- and T-cell responses. Scand J Immunol 55(1):24–32
Borregaard N, Jensen HS, Bjerrum OW (1987) Prevention of tissue damage: inhibition of myeloperoxidase mediated inactivation of alpha 1-proteinase inhibitor by N-acetyl cysteine, glutathione, and methionine. Agents Actions 22(3–4):255–260
Bostom AG, Shemin D, Yoburn D, Fisher DH, Nadeau MR, Selhub J (1996) Lack of effect of oral N-acetylcysteine on the acute dialysis-related lowering of total plasma homocysteine in hemodialysis patients. Atherosclerosis 120(1–2):241–244
Bounous G (2000) Whey protein concentrate (WPC) and glutathione modulation in cancer treatment. Anticancer Res 20(6C):4785–4792
Boushey CJ, Beresford SA, Omenn GS, Motulsky AG (1995) A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes. JAMA 274(13):1049–1057
Bowles WH, Goral V (1985) Clinical trial of the anti-plaque activity of a mucolytic agent, N-acetyl cysteine. Dent Hyg (Chic) 59(10):454–456
Bray GP, Mowat C, Muir DF, Tredger JM, Williams R (1991) The effect of chronic alcohol intake on prognosis and outcome in paracetamol overdose. Hum Exp Toxicol 10(6):435–438
Breitkreutz R, Holm S, Pittack N, Beichert M, Babylon A, Yodoi J, Droge W (2000a) Massive loss of sulfur in HIV infection. AIDS Res Hum Retrovir 16(3):203–209
Breitkreutz R, Pittack N, Nebe CT, Schuster D, Brust J, Beichert M, Hack V, Daniel V, Edler L, Droge W (2000b) Improvement of immune functions in HIV infection by sulfur supplementation: two randomized trials. J Mol Med 78(1):55–62
Briganti S, Wlaschek M, Hinrichs C, Bellei B, Flori E, Treiber N, Iben S, Picardo M, Scharffetter-Kochanek K (2008) Small molecular antioxidants effectively protect from PUVA-induced oxidative stress responses underlying fibroblast senescence and photoaging. Free Radic Biol Med 45(5):636–644. https://doi.org/10.1016/j.freeradbiomed.2008.05.006
Briguori C, Manganelli F, Scarpato P, Elia PP, Golia B, Riviezzo G, Lepore S, Librera M, Villari B, Colombo A, Ricciardelli B (2002) Acetylcysteine and contrast agent-associated nephrotoxicity. J Am Coll Cardiol 40(2):298–303
Brocard H, Charpin J, Germouty J (1980) Multicenter, double-blind study of oral acetylcysteine vs. placebo. Eur J Respir Dis Suppl 111:65–69
Brok J, Buckley N, Gluud C (2002) Interventions for paracetamol (acetaminophen) overdoses. Cochrane Database Syst Rev 3:CD003328
Bromley PN, Cottam SJ, Hilmi I, Tan KC, Heaton N, Ginsburg R, Potter DR (1995) Effects of intraoperative N-acetylcysteine in orthotopic liver transplantation. Br J Anaesth 75(3):352–354
Broughan TA, Soloway RD (2000) Acetaminophen hepatoxicity. Dig Dis Sci 45(8):1553–1558
Brown L, Rimm EB, Seddon JM, Giovannucci EL, Chasan-Taber L, Spiegelman D, Willett WC, Hankinson SE (1999) A prospective study of carotenoid intake and risk of cataract extraction in US men. Am J Clin Nutr 70(4):517–524
Buckley NA, Whyte IM, O’Connell DL, Dawson AH (1999) Oral or intravenous N-acetylcysteine: which is the treatment of choice for acetaminophen (paracetamol) poisoning? J Toxicol Clin Toxicol 37(6):759–767
Buhl R, Holroyd KJ, Mastrangeli A, Cantin AM, Jaffe HA, Wells FB, Saltini C, Crystal RG (1989) Systemic glutathione deficiency in symptom-free HIV-seropositive individuals. Lancet 334:1294–1298
Burgunder JM, Varriale A, Lauterburg BH (1989) Effect of N-acetylcysteine on plasma cysteine and glutathione following paracetamol administration. Eur J Clin Pharmacol 36(2):127–131
Bylin G, Hedenstierna G, Lagerstrand L, Wagner PD (1987) No influence of acetylcysteine on gas exchange and spirometry in chronic asthma. Eur J Respir Dis 71(2):102–107
Cantin AM, Hubbard RC, Crystal RG (1989) Glutathione deficiency in the epithelial lining fluid of the lower respiratory tract in idiopathic pulmonary fibrosis. Am Rev Respir Dis 139:370–372
Casagrande S, Bonetto V, Fratelli M, Gianazza E, Eberini I, Massignan T, Salmona M, Chang G, Holmgren A, Ghezzi P (2002) Glutathionylation of human thioredoxin: a possible crosstalk between the glutathione and thioredoxin systems. Proc Natl Acad Sci U S A 99(15):9745–9749. https://doi.org/10.1073/pnas.152168599
Castagna A, Legrazie C, Accordini A, Giulidori P, Cavalli G, Bottiglieri T, Lazzarin A (1995) Cerebrospinal fluid S-adenosylmethionine (SAMe) and glutathione concentrations in HIV infection: effect of parenteral treatment with SAMe. Neurology 45(9):1678–1683
Cayota A, Vuillier F, Gonzalez G, Dighiero G (1996) In vitro antioxidant treatment recovers proliferative responses of anergic CD4+ lymphocytes from human immunodeficiency virus-infected individuals. Blood 87(11):4746–4753
Chasan-Taber L, Willett WC, Seddon JM, Stampfer MJ, Rosner B, Colditz GA, Speizer FE, Hankinson SE (1999) A prospective study of carotenoid and vitamin A intakes and risk of cataract extraction in US women. Am J Clin Nutr 70(4):509–516
Chiao JW, Chung FL, Kancherla R, Ahmed T, Mittelman A, Conaway CC (2002) Sulforaphane and its metabolite mediate growth arrest and apoptosis in human prostate cancer cells. Int J Oncol 20(3):631–636
Chikina S, Iagmurov B, Kopylev ID, Soodaeva SK, Chuchalin AG (2002) N-Acetylcysteine: low and high doses in the treatment of chronic obstructive lung diseases in Chernobyl accident liquidators. Ter Arkh 74(3):62–65
Childs A, Jacobs C, Kaminski T, Halliwell B, Leeuwenburgh C (2001) Supplementation with vitamin C and N-acetyl-cysteine increases oxidative stress in humans after an acute muscle injury induced by eccentric exercise. Free Radic Biol Med 31(6):745–753
Choudhary G, Dudley SC Jr (2002) Heart failure, oxidative stress, and ion channel modulation. Congest Heart Fail 8(3):148–155
Christman BW, Bernard GR (1993) Antilipid mediator and antioxidant therapy in adult respiratory distress syndrome. New Horiz 1(4):623–630
Clotet B, Gomez M, Ruiz L, Sirera G, Romeu J (1995) Lack of short-term efficacy of N-acetyl-L-cysteine in human immunodeficiency virus-positive patients with CD4 cell counts <250/mm(3) {Letter}. J Acquir Immun Defic Syndr Hum Retrovirol 9(1):98–99
Cogo A, Chieffo A, Farinatti M, Ciaccia A (1996) Efficacy of topical tuaminoheptane combined with N-acetyl-cysteine in reducing nasal resistance. A double-blind rhinomanometric study versus xylometazoline and placebo. Arzneimittelforschung 46(4):385–388
Cotgreave IA, Goldschmidt L, Tonkonogi M, Svensson M (2002) Differentiation-specific alterations to glutathione synthesis in and hormonally stimulated release from human skeletal muscle cells. FASEB J 16(3):435–437
Coyle LC, Rodriguez A, Jeschke RE, Simon-Lee A, Abbott KC, Taylor AJ (2006) Acetylcysteine in diabetes (AID): a randomized study of acetylcysteine for the prevention of contrast nephropathy in diabetics. Am Heart J 151(5):1032.e9–1032.e12. https://doi.org/10.1016/j.ahj.2006.02.002
Daily D, Vlamis-Gardikas A, Offen D, Mittelman L, Melamed E, Holmgren A, Barzilai A (2001) Glutaredoxin protects cerebellar granule neurons from dopamine-induced apoptosis by activating NF-kappa B via Ref-1. J Biol Chem 276(2):1335–1344. https://doi.org/10.1074/jbc.M008121200
Davidson SD, Milanesa DM, Mallouh C, Choudhury MS, Tazaki H, Konno S (2002) A possible regulatory role of glyoxalase I in cell viability of human prostate cancer. Urol Res 30(2):116–121
Davies SJ, Reichardt-Pascal SY, Vaughan D, Russell GI (1995) Differential effect of ischaemia-reperfusion injury on anti-oxidant enzyme activity in the rat kidney. Exp Nephrol 3(6):348–354
Davis M (1986) Protective agents for acetaminophen overdose. Semin Liver Dis 6(2):138–147
De Backer WA, Amsel B, Jorens PG, Bossaert L, Hiemstra PS, van Noort P, van Overveld FJ (1996) N-acetylcysteine pretreatment of cardiac surgery patients influences plasma neutrophil elastase and neutrophil influx in bronchoalveolar lavage fluid. Intensive Care Med 22(9):900–908
De Flora S, Grassi C, Carati L (1997) Attenuation of influenza-like symptomatology and improvement of cell-mediated immunity with long-term N-acetylcysteine treatment. Eur Respir J 10(7):1535–1541
De Mattia G, Bravi MC, Laurenti O, Cassone-Faldetta M, Armiento A, Ferri C, Balsano F (1998a) Influence of reduced glutathione infusion on glucose metabolism in patients with non-insulin-dependent diabetes mellitus. Metabolism 47(8):993–997
De Mattia G, Bravi MC, Laurenti O, Cassone-Faldetta M, Proietti A, De Luca O, Armiento A, Ferri C (1998b) Reduction of oxidative stress by oral N-acetyl-L-cysteine treatment decreases plasma soluble vascular cell adhesion molecule-1 concentrations in non-obese, non-dyslipidaemic, normotensive, patients with non-insulin-dependent diabetes. Diabetologia 41(11):1392–1396
de Quay B, Malinverni R, Lauterburg BH (1992) Glutathione depletion in HIV-infected patients: role of cysteine deficiency and effect of oral N-acetylcysteine. AIDS 6(8):815–819
De Roos FJ, Hoffman RS (1996) Drug-induced hepatotoxicity. N Engl J Med 334(13):863. discussion 864
De Rosa SC, Zaretsky MD, Dubs JG, Roederer M, Anderson M, Green A, Mitra D, Watanabe N, Nakamura H, Tjioe I, Deresinski SC, Moore WA, Ela SW, Parks D, Herzenberg LA (2000) N-acetylcysteine replenishes glutathione in HIV infection. Eur J Clin Investig 30(10):915–929
De Stefano N, Matthews PM, Ford B, Genge A, Karpati G, Arnold DL (1995) Short-term dichloroacetate treatment improves indices of cerebral metabolism in patients with mitochondrial disorders. Neurology 45(6):1193–1198
Dean BS, Bricker JD, Krenzelok EP (1996) Outpatient N-acetylcysteine treatment for acetaminophen poisoning: an ethical dilemma or a new financial mandate? Vet Hum Toxicol 38(3):222–224
Demirturk L, Yazgan Y, Tarcin O, Ozel M, Diler M, Oncul O, Yildirim S (2003) Does N-acetyl cystein affect the sensitivity and specificity of Helicobacter pylori stool antigen test? Helicobacter 8(2):120–123
Di Bisceglie AM (1998) Hepatitis C. Lancet 351(9099):351–355
Diaz-Sandoval LJ, Kosowsky BD, Losordo DW (2002) Acetylcysteine to prevent angiography-related renal tissue injury (the APART trial). Am J Cardiol 89(3):356–358
Dick CA, Brown DM, Donaldson K, Stone V (2003) The role of free radicals in the toxic and inflammatory effects of four different ultrafine particle types. Inhal Toxicol 15(1):39–52
Dincer Y, Akcay T, Konukogku D, Hatemi H (1999) Erythrocyte susceptibility to lipid peroxidation in patients with coronary atherosclerosis. Acta Med Okayama 53(6):259–264
Domenighetti G, Suter PM, Schaller MD, Ritz R, Perret C (1997) Treatment with N-acetylcysteine during acute respiratory distress syndrome: a randomized, double-blind, placebo-controlled clinical study. J Crit Care 12(4):177–182
Drager LF, Andrade L, Barros de Toledo JF, Laurindo FR, Machado Cesar LA, Seguro AC (2004) Renal effects of N-acetylcysteine in patients at risk for contrast nephropathy: decrease in oxidant stress-mediated renal tubular injury. Nephrol Dial Transplant 19(7):1803–1807
Droge W, Breitkreutz R (1999) N-acetyl-cysteine in the therapy of HIV-positive patients. Curr Opin Clin Nutr Metab Care 2(6):493–498
Droge W, Breitkreutz R (2000) Glutathione and immune function. Proc Nutr Soc 59(4):595–600
Droge W, Eck H-P, Gmunder H, Mihm S (1991) Modulation of lymphocyte functions and immune responses by cysteine and cysteine derivatives. Am J Med 91(Suppl. 3C):140S–144S
Droge W, Eck H-P, Naher H, Pekar U, Daniel V (1988) Abnormal amino-acid concentrations in the blood of patients with acquired immunodeficiency syndrome (AIDS) may contribute to the immunological deficit. Biol Chem Hoppe Seyler 369:143–148
Droge W, Eck HP, Mihm S (1992) HIV-induced cysteine deficiency and T-cell dysfunction – a rationale for treatment with N-acetylcysteine. Immunol Today 13(6):211–214
Dueholm M, Nielsen C, Thorshauge H, Evald T, Hansen NC, Madsen HD, Maltbaek N (1992) N-acetylcysteine by metered dose inhaler in the treatment of chronic bronchitis: a multi-centre study. Respir Med 86(2):89–92
Durham JD, Caputo C, Dokko J, Zaharakis T, Pahlavan M, Keltz J, Dutka P, Marzo K, Maesaka JK, Fishbane S (2002) A randomized controlled trial of N-acetylcysteine to prevent contrast nephropathy in cardiac angiography. Kidney Int 62(6):2202–2207
Efrati S, Dishy V, Averbukh M, Blatt A, Krakover R, Weisgarten J, Morrow JD, Stein MC, Golik A (2003) The effect of N-acetylcysteine on renal function, nitric oxide, and oxidative stress after angiography. Kidney Int 64(6):2182–2187
Ekberg-Jansson A, Larson M, MacNee W, Tunek A, Wahlgren L, Wouters EF, Larsson S (1999) N-isobutyrylcysteine, a donor of systemic thiols, does not reduce the exacerbation rate in chronic bronchitis. Eur Respir J 13(4):829–834
Eklund A, Eriksson O, Hakansson L, Larsson K, Ohlsson K, Venge P, Bergstrand H, Bjornson A, Brattsand R, Glennow C et al (1988) Oral N-acetylcysteine reduces selected humoral markers of inflammatory cell activity in BAL fluid from healthy smokers: correlation to effects on cellular variables. Eur Respir J 1(9):832–838
Eren N, Cakir O, Oruc A, Kaya Z, Erdinc L (2003) Effects of N-acetylcysteine on pulmonary function in patients undergoing coronary artery bypass surgery with cardiopulmonary bypass. Perfusion 18(6):345–350
Estensen RD, Levy M, Klopp SJ, Galbraith AR, Mandel JS, Blomquist JA, Wattenberg LW (1999) N-acetylcysteine suppression of the proliferative index in the colon of patients with previous adenomatous colonic polyps. Cancer Lett 147(1–2):109–114
Estevez AG, Jordan J (2002) Nitric oxide and superoxide, a deadly cocktail. Ann N Y Acad Sci 962:207–211
Evald T, Hansen M, Balslov S, Brorson-Riis L, Hansen NC, Maltbaek N, Thorshauge H (1989) Steroid response after long-term treatment with oral N-acetylcysteine in patients with chronic obstructive bronchitis. Ugeskr Laeger 151(46):2076–2078
Eylar E, Rivera-Quinones C, Molina C, Baez I, Molina F, Mercado CM (1993) N-acetylcysteine enhances T cell functions and T cell growth in culture. Int Immunol 5(1):97–101
Fechner A, Bohme C, Gromer S, Funk M, Schirmer R, Becker K (2001) Antioxidant status and nitric oxide in the malnutrition syndrome kwashiorkor. Pediatr Res 49(2):237–243
Ferrari V (1980) Safety and drug interactions of oral acetylcysteine related to utilization data. Eur J Respir Dis Suppl 111:151–157
Ferrari V, Spinelli W (1980) Life table analysis of long-term randomised trials in pneumology – a worked example and a plea. Eur J Respir Dis Suppl 110:227–236
Fischer UM, Tossios P, Huebner A, Geissler HJ, Bloch W, Mehlhorn U (2004) Myocardial apoptosis prevention by radical scavenging in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg 128(1):103–108
Flescher E, Ledbetter JA, Schieven GL, Velaroch N, Fossum D, Dang H, Ogawa N, Talal N (1994) Longitudinal exposure of human T lymphocytes to weak oxidative stress suppresses transmembrane and nuclear signal transduction. J Immunol 153(11):4880–4889
Fontana RJ, McCashland TM, Benner KG, Appelman HD, Gunartanam NT, Wisecarver JL, Rabkin JM, Lee WM (1999) Acute liver failure associated with prolonged use of bromfenac leading to liver transplantation. The Acute Liver Failure Study Group. Liver Transpl Surg 5(6):480–484
Freudenthaler SM, Schreeb KH, Wiese A, Pilz J, Gleiter CH (2002) Influence of controlled hypoxia and radical scavenging agents on erythropoietin and malondialdehyde concentrations in humans. Acta Physiol Scand 174(3):231–235
Friedman AN, Bostom AG, Laliberty P, Selhub J, Shemin D (2003) The effect of N-acetylcysteine on plasma total homocysteine levels in hemodialysis: a randomized, controlled study. Am J Kidney Dis 41(2):442–446
Fulghesu AM, Ciampelli M, Muzj G, Belosi C, Selvaggi L, Ayala GF, Lanzone A (2002) N-acetyl-cysteine treatment improves insulin sensitivity in women with polycystic ovary syndrome. Fertil Steril 77(6):1128–1135
Furst DE, Clements PJ, Harris R, Ross M, Levy J, Paulus HE (1979) Measurement of clinical change in progressive systemic sclerosis: a 1 year double-blind placebo-controlled trial of N-acetylcysteine. Ann Rheum Dis 38(4):356–361
Galli F, Floridi A, Buoncristiani U (2002) Oxidant stress in hemodialysis patients. Contrib Nephrol 137:371–378
Ghezzi P, Romines B, Fratelli M, Eberini I, Gianazza E, Casagrande S, Laragione T, Mengozzi M, Herzenberg LA (2002) Protein glutathionylation: coupling and uncoupling of glutathione to protein thiol groups in lymphocytes under oxidative stress and HIV infection. Mol Immunol 38(10):773–780
Gillissen A, Nowak D (1998) Characterization of N-acetylcysteine and ambroxol in anti-oxidant therapy. Respir Med 92(4):609–623
Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Willett WC (1998) Diabetes mellitus and risk of prostate cancer (United States). Cancer Causes Control 9(1):3–9
Gisolf EH, Dreezen C, Danner SA, Weel JL, Weverling GJ (2000) Risk factors for hepatotoxicity in HIV-1-infected patients receiving ritonavir and saquinavir with or without stavudine. Prometheus Study Group. Clin Infect Dis 31(5):1234–1239
Gladyshev VN, Jeang KT, Stadtman TC (1996a) Selenocysteine, identified as the penultimate C-terminal residue in human T-cell thioredoxin reductase, corresponds to TGA in the human placental gene. Proc Natl Acad Sci U S A 93(12):6146–6151
Gladyshev VN, Khangulov SV, Stadtman TC (1996b) Properties of the selenium- and molybdenum-containing nicotinic acid hydroxylase from Clostridium barkeri. Biochemistry 35(1):212–223. https://doi.org/10.1021/bi951793i
Golden MH, Ramdath D (1987) Free radicals in the pathogenesis of kwashiorkor. Proc Nutr Soc 46(1):53–68
Goldenberg I, Shechter M, Matetzky S, Jonas M, Adam M, Pres H, Elian D, Agranat O, Schwammenthal E, Guetta V (2004) Oral acetylcysteine as an adjunct to saline hydration for the prevention of contrast-induced nephropathy following coronary angiography. A randomized controlled trial and review of the current literature. Eur Heart J 25(3):212–218
Gotoh Y, Noda T, Iwakiri R, Fujimoto K, Rhoads CA, Aw TY (2002) Lipid peroxide-induced redox imbalance differentially mediates CaCo-2 cell proliferation and growth arrest. Cell Prolif 35(4):221–235
Gotz M, Kraemer R, Kerrebijn KF, Popow C (1980) Oral acetylcysteine in cystic fibrosis. A co-operative study. Eur J Respir Dis Suppl 111:122–126
Gow AJ, Chen Q, Hess DT, Day BJ, Ischiropoulos H, Stamler JS (2002) Basal and stimulated protein S-nitrosylation in multiple cell types and tissues. J Biol Chem 277(12):9637–9640. https://doi.org/10.1074/jbc.C100746200
Graber R, Farine JC, Fumagalli I, Tatti V, Losa GA (1999) Apoptosis and oxidative status in peripheral blood mononuclear cells of diabetic patients. Apoptosis 4(4):263–270
Grandjean EM, Berthet P, Ruffmann R, Leuenberger P (2000) Cost-effectiveness analysis of oral N-acetylcysteine as a preventive treatment in chronic bronchitis. Pharmacol Res 42(1):39–50
Grant PR, Black A, Garcia N, Prieto J, Garson JA (2000) Combination therapy with interferon-alpha plus N-acetyl cysteine for chronic hepatitis C: a placebo controlled double-blind multicentre study. J Med Virol 61(4):439–442
Grassi C (1980) Long-term oral acetylcysteine in chronic bronchitis. A double-blind controlled study. Eur J Respir Dis Suppl 111:93–108
Grassi C, Morandini GC (1976) A controlled trial of intermittent oral acetylcysteine in the long-term treatment of chronic bronchitis. Eur J Clin Pharmacol 09(5–6):393–396
Grattagliano I, Vendemiale G, Sabba C, Buonamico P, Altomare E (1996) Oxidation of circulating proteins in alcoholics: role of acetaldehyde and xanthine oxidase. J Hepatol 25(1):28–36
Gringhuis SI, Leow A, Papendrecht-van der Voort EAM, Remans PHJ, Breedveld FC, Verweij CL (2000) Displacement of linker for activation of T cells from the plasma membrane due to redox balance alterations results in hyporesponsiveness of synovial fluid T lymphocytes in rheumatoid arthritis. J Immunol 164(4):2170–2179
Grundman M (2000) Vitamin E and Alzheimer disease: the basis for additional clinical trials. Am J Clin Nutr 71(2):630S–636S
Guan X, Hoffman BN, McFarland DC, Gilkerson KK, Dwivedi C, Erickson AK, Bebensee S, Pellegrini J (2002) Glutathione and mercapturic acid conjugates of sulofenur and their activity against a human colon cancer cell line. Drug Metab Dispos 30(3):331–335
Hammarqvist F, Luo JL, Cotgreave IA, Andersson K, Wernerman J (1997) Skeletal muscle glutathione is depleted in critically ill patients. Crit Care Med 25(1):78–84
Hansen NC, Skriver A, Brorsen-Riis L, Balslov S, Evald T, Maltbaek N, Gunnersen G, Garsdal P, Sander P, Pedersen JZ et al (1994) Orally administered N-acetylcysteine may improve general well-being in patients with mild chronic bronchitis. Respir Med 88(7):531–535
Hansen RM, Csuka ME, McCarty DJ, Saryan LA (1985) Gold induced aplastic anemia. Complete response to corticosteroids, plasmapheresis, and N-acetylcysteine infusion. J Rheumatol 12(4):794–797
Hansen RM, Varma RR, Hanson GA (1991) Gold induced hepatitis and pure red cell aplasia. Complete recovery after corticosteroid and N-acetylcysteine therapy. J Rheumatol 18(8):1251–1253
Harrison PM, Keays R, Bray GP, Alexander GJ, Williams R (1990) Improved outcome of paracetamol-induced fulminant hepatic failure by late administration of acetylcysteine. Lancet 335(8705):1572–1573
Harrison PM, Wendon JA, Gimson AE, Alexander GJ, Williams R (1991) Improvement by acetylcysteine of hemodynamics and oxygen transport in fulminant hepatic failure. N Engl J Med 324(26):1852–1857
Hauer K, Hildebrandt W, Sehl Y, Edler L, Oster P, Droge W (2003) Improvement in muscular performance and decrease in tumor necrosis factor level in old age after antioxidant treatment. J Mol Med 81(2):118–125
Heinig JH, Pedersen B, Andersen I, Dalgaard CE, Rasmussen O, Weeke ER, Enk B (1985) The mucolytic effects of acetylcysteine compared with bromhexine and a placebo in patients with chronic bronchitis. Ugeskr Laeger 147(46):3694–3697
Helbling B, von Overbeck J, Lauterburg BH (1996) Decreased release of glutathione into the systemic circulation of patients with HIV infection. Eur J Clin Investig 26(1):38–44
Henderson A, Hayes P (1994) Acetylcysteine as a cytoprotective antioxidant in patients with severe sepsis: potential new use for an old drug. Ann Pharmacother 28(9):1086–1088
Herzenberg LA, De Rosa SC, Dubs JG, Roederer M, Anderson MT, Ela SW, Deresinski SC (1997) Glutathione deficiency is associated with impaired survival in HIV disease. Proc Natl Acad Sci U S A 94(5):1967–1972
Hitchins AD, McDonough FE, Wells PA (1989) The use of Escherichia coli mutants to measure the bioavailability of essential amino acids in foods. Plant Foods Hum Nutr 39(1):109–120
Hoffer ME, Kopke RD, Weisskopf P, Gottshall K, Allen K, Wester D (2001) Microdose gentamicin administration via the round window microcatheter: results in patients with Meniere’s disease. Ann N Y Acad Sci 942:46–51
Hogan JC, Lewis MJ, Henderson AH (1989a) Glyceryl trinitrate and platelet aggregation: effects of N-acetyl-cysteine. Br J Clin Pharmacol 27(5):617–619
Hogan JC, Lewis MJ, Henderson AH (1989b) N-acetylcysteine fails to attenuate haemodynamic tolerance to glyceryl trinitrate in healthy volunteers. Br J Clin Pharmacol 28(4):421–426
Hogan JC, Lewis MJ, Henderson AH (1990) Chronic administration of N-acetylcysteine fails to prevent nitrate tolerance in patients with stable angina pectoris. Br J Clin Pharmacol 30(4):573–577
Holmgren A (1985) Thioredoxin. Annu Rev Biochem 54:237–271
Holmgren A (1989) Thioredoxin and glutaredoxin systems. J Biol Chem 264(24):13963–13966
Holroyd KJ, Buhl R, Borok Z, Roum JH, Bokser AD, Grimes GJ, Czerski D, Cantin AM, Crystal RG (1993) Correction of glutathione deficiency in the lower respiratory tract of HIV seropositive individuals by glutathione aerosol treatment. Thorax 48(10):985–989
Holt S, Goodler D, Marley R, Patch D, Burroughs A, Fernando B, Harry D, Moore K (1999a) Improvement in renal function in hepatorenal syndrome with N-acetylcysteine [letter]. Lancet 353(9149):294–295
Holt S, Marley R, Fernando B, Harry D, Anand R, Goodier D, Moore K (1999b) Acute cholestasis-induced renal failure: effects of antioxidants and ligands for the thromboxane A2 receptor. Kidney Int 55(1):271–277
Horowitz JD, Henry CA, Syrjanen ML, Louis WJ, Fish RD, Antman EM, Smith TW (1988a) Nitroglycerine/N-acetylcysteine in the management of unstable angina pectoris. Eur Heart J 9(Suppl A):95–100
Horowitz JD, Henry CA, Syrjanen ML, Louis WJ, Fish RD, Smith TW, Antman EM (1988b) Combined use of nitroglycerin and N-acetylcysteine in the management of unstable angina pectoris. Circulation 77(4):787–794
Hortin GL, Landt M, Powderly WG (1994) Changes in plasma amino acid concentrations in response to HIV-1 infection. Clin Chem 40:785–789
Huengsberg M, Waring R, Moffitt D, Round R, Winer J, Gompels M, Shahmanesh M (1998) Serum cysteine levels in HIV infection. {LETTER, COMMENT}. AIDS 12(10):1245
Hultberg B, Andersson A, Isaksson A (2001) Interaction of metals and thiols in cell damage and glutathione distribution: potentiation of mercury toxicity by dithiothreitol. Toxicology 156(2–3):93–100
Hurd RW, Wilder BJ, Helveston WR, Uthman BM (1996) Treatment of four siblings with progressive myoclonus epilepsy of the Unverricht-Lundborg type with N-acetylcysteine. Neurology 47(5):1264–1268
Hursting SD, Shen JC, Sun XY, Wang TT, Phang JM, Perkins SN (2002) Modulation of cyclophilin gene expression by N-4-(hydroxyphenyl)retinamide: association with reactive oxygen species generation and apoptosis. Mol Carcinog 33(1):16–24
Iantomasi T, Marraccini P, Favilli F, Vincenzini MT, Ferretti P, Tonelli F (1994) Glutathione metabolism in Crohn’s disease. Biochem Med Metab Biol 53(2):87–91
Iversen HK (1992) N-acetylcysteine enhances nitroglycerin-induced headache and cranial arterial responses. Clin Pharmacol Ther 52(2):125–133
Jackson AA (1986) Blood glutathione in severe malnutrition in childhood. Trans R Soc Trop Med Hyg 80(6):911–913
Jackson IM, Barnes J, Cooksey P (1984) Efficacy and tolerability of oral acetylcysteine (Fabrol) in chronic bronchitis: a double-blind placebo controlled study. J Int Med Res 12(3):198–206
Jahoor F, Jackson A, Gazzard B, Philips G, Sharpstone D, Frazer ME, Heird W (1999) Erythrocyte glutathione deficiency in symptom-free HIV infection is associated with decreased synthesis rate. Am J Phys 276(1 Pt 1):E205–E211
Jain SK, Krueger KS, McVie R, Jaramillo JJ, Palmer M, Smith T (1998) Relationship of blood thromboxane-B2 (TxB2) with lipid peroxides and effect of vitamin E and placebo supplementation on TxB2 and lipid peroxide levels in type 1 diabetic patients. Diabetes Care 21(9):1511–1516
Jain SK, Lim G (2000) Lipoic acid decreases lipid peroxidation and protein glycosylation and increases (Na(+) + K(+))- and Ca(++)-ATPase activities in high glucose-treated human erythrocytes. Free Radic Biol Med 29(11):1122–1128
Jain SK, McVie R (1999) Hyperketonemia can increase lipid peroxidation and lower glutathione levels in human erythrocytes in vitro and in type 1 diabetic patients. Diabetes 48(9):1850–1855
Jain SK, McVie R, Jaramillo JJ, Palmer M, Smith T (1996a) Effect of modest vitamin E supplementation on blood glycated hemoglobin and triglyceride levels and red cell indices in type I diabetic patients. J Am Coll Nutr 15(5):458–461
Jain SK, McVie R, Jaramillo JJ, Palmer M, Smith T, Meachum ZD, Little RL (1996b) The effect of modest vitamin E supplementation on lipid peroxidation products and other cardiovascular risk factors in diabetic patients. Lipids 31(Suppl):87–90
Jain SK, McVie R, Smith T (2000) Vitamin E supplementation restores glutathione and malondialdehyde to normal concentrations in erythrocytes of type 1 diabetic children. Diabetes Care 23(9):1389–1394
James JS (1997) Stanford NAC study: glutathione level predicts survival. AIDS Treat News 266:1–5
James LP, Wells E, Beard RH, Farrar HC (2002) Predictors of outcome after acetaminophen poisoning in children and adolescents. J Pediatr 140(5):522–526
Jeannin P, Delneste Y, Lecoanet-Henchoz S, Gauchat J-F, Life P, Holmes D, Bonnefoy J-Y (1995) Thiols decrease human interleukin (IL) 4 production and IL-4-induced immunoglobulin synthesis. J Exp Med 182(6):1785–1792
Jepsen S, Herlevsen P, Knudsen P, Bud MI, Klausen NO (1992) Antioxidant treatment with N-acetylcysteine during adult respiratory distress syndrome: a prospective, randomized, placebo-controlled study. Crit Care Med 20(7):918–923
Jepsen S, Klaerke A, Nielsen PH, Nielsen ST, Simonsen O (1989) Systemic administration of N-acetylcysteine has no effect on postoperative lung function following elective upper laparotomy in lung healthy patients. Acta Anaesthesiol Scand 33(3):219–222
Johnston SC, Pelletier LL Jr (1997) Enhanced hepatotoxicity of acetaminophen in the alcoholic patient. Two case reports and a review of the literature. Medicine (Baltimore) 76(3):185–191
Jones A (2002) Over-the-counter analgesics: a toxicology perspective. Am J Ther 9(3):245–257
Julius M, Lang CA, Gleiberman L, Harburg E, DiFranceisco W, Schork A (1994) Glutathione and morbidity in a community-based sample of elderly. J Clin Epidemiol 47(9):1021–1026
Kanner SB, Damle NK, Blake J, Aruffo A, Ledbetter JA (1992a) CD2/LFA-3 ligation induces phospholipase-C gamma 1 tyrosine phosphorylation and regulates CD3 signaling. J Immunol 148(7):2023–2029
Kanner SB, Deans JP, Ledbetter JA (1992b) Regulation of CD3-induced phospholipase C-gamma 1 (PLC gamma 1) tyrosine phosphorylation by CD4 and CD45 receptors. Immunology 75(3):441–447
Kanner SB, Kavanagh TJ, Grossmann A, Hu SL, Bolen JB, Rabinovitch PS, Ledbetter JA (1992c) Sulfhydryl oxidation down-regulates T-cell signaling and inhibits tyrosine phosphorylation of phospholipase C gamma 1. Proc Natl Acad Sci U S A 89(1):300–304
Kanner SB, Ledbetter JA (1992) CD45 regulates TCR-induced signalling through tyrosine phosphorylation of phospholipase C gamma 1. Biochem Soc Trans 20(1):178–184
Kasielski M, Nowak D (2001) Long-term administration of N-acetylcysteine decreases hydrogen peroxide exhalation in subjects with chronic obstructive pulmonary disease. Respir Med 95(6):448–456
Katsinelos P, Kountouras J, Paroutoglou G, Beltsis A, Mimidis K, Zavos C (2005) Intravenous N-acetylcysteine does not prevent post-ERCP pancreatitis. Gastrointest Endosc 62(1):105–111
Kay J, Chow WH, Chan TM, Lo SK, Kwok OH, Yip A, Fan K, Lee CH, Lam WF (2003) Acetylcysteine for prevention of acute deterioration of renal function following elective coronary angiography and intervention: a randomized controlled trial. JAMA 289(5):553–558
Kearns GL (2002) Acetaminophen poisoning in children: treat early and long enough. J Pediatr 140(5):495–498
Kearns GL, Leeder JS, Wasserman GS (2000) Acetaminophen intoxication during treatment: what you don’t know can hurt you. Clin Pediatr (Phila) 39(3):133–144
Keays R, Harrison PM, Wendon JA, Forbes A, Gove C, Alexander GJ, Williams R (1991) Intravenous acetylcysteine in paracetamol induced fulminant hepatic failure: a prospective controlled trial. BMJ 303(6809):1026–1029
Kefer JM, Hanet CE, Boitte S, Wilmotte L, De Kock M (2003) Acetylcysteine, coronary procedure and prevention of contrast-induced worsening of renal function: which benefit for which patient? Acta Cardiol 58(6):555–560
Kelly FJ (1999) Gluthathione: in defence of the lung. Food Chem Toxicol 37(9–10):963–966
Kerr F, Dawson A, Whyte IM, Buckley N, Murray L, Graudins A, Chan B, Trudinger B (2005) The Australasian Clinical Toxicology Investigators Collaboration randomized trial of different loading infusion rates of N-acetylcysteine. Ann Emerg Med 45(4):402–408
Kes P (2000) Hyperhomocysteinemia in end-stage renal failure. Acta Med Croatica 54(4–5):175–181
Kiefer P, Vogt J, Radermacher P (2000) From mucolytic to antioxidant and liver protection: new aspects in the intensive care unit career of N-acetylcysteine. Crit Care Med 28(12):3935–3936
Kim HJ, Liu X, Wang H, Kohyama T, Kobayashi T, Wen FQ, Romberger DJ, Abe S, MacNee W, Rahman I, Rennard SI (2002) Glutathione prevents inhibition of fibroblast-mediated collagen gel contraction by cigarette smoke. Am J Physiol Lung Cell Mol Physiol 283(2):L409–L417
Kinnunen J, Pietila J, Ahovuo J, Mankinen P, Tervahartiala P (1989) Double contrast barium meal and acetylcysteine. Eur J Radiol 9(4):258–259
Knapen MFCM, Mulder TPJ, Van Rooij IALM, Peters WHM, Steegers EAP (1998) Low whole blood glutathione levels in pregnancies complicated by preeclampsia or the hemolysis, elevated liver enzymes, low platelets syndrome. Obstet Gynecol 92(6):1012–1015
Koechlin C, Couillard A, Simar D, Cristol JP, Bellet H, Hayot M, Prefaut C (2004) Does oxidative stress alter quadriceps endurance in chronic obstructive pulmonary disease? Am J Respir Crit Care Med 169(9):1022–1027
Kokcam I, Naziroglu M (1999) Antioxidants and lipid peroxidation status in the blood of patients with psoriasis. Clin Chim Acta 289(1–2):23–31
Konrad F, Schoenberg MH, Wiedmann H, Kilian J, Georgieff M (1995) The application of n-acetylcysteine as an antioxidant and mucolytic in mechanical ventilation in intensive care patients. A prospective, randomized, placebo-controlled, double-blind study. Anaesthesist 44(9):651–658
Konukoglu D, Akcay T, Dincer Y, Hatemi H (1999) The susceptibility of red blood cells to autoxidation in type 2 diabetic patients with angiopathy. Metabolism 48(12):1481–1484
Konukoglu D, Hatemi H, Ozer EM, Gonen S, Akcay T (1997) The erythrocyte glutathione levels during oral glucose tolerance test. J Endocrinol Investig 20(8):471–475
Kopke R, Allen KA, Henderson D, Hoffer M, Frenz D, Van de Water T (1999) A radical demise. Toxins and trauma share common pathways in hair cell death. Ann N Y Acad Sci 884:171–191
Kopke RD, Coleman JK, Liu J, Campbell KC, Riffenburgh RH (2002) Candidate’s thesis: enhancing intrinsic cochlear stress defenses to reduce noise-induced hearing loss. Laryngoscope 112(9):1515–1532. https://doi.org/10.1097/00005537-200209000-00001
Kopke RD, Hoffer ME, Wester D, O’Leary MJ, Jackson RL (2001) Targeted topical steroid therapy in sudden sensorineural hearing loss. Otol Neurotol 22(4):475–479
Kopke RD, Weisskopf PA, Boone JL, Jackson RL, Wester DC, Hoffer ME, Lambert DC, Charon CC, Ding DL, McBride D (2000) Reduction of noise-induced hearing loss using L-NAC and salicylate in the chinchilla. Hear Res 149(1–2):138–146
Krenzelok EP (2002) New developments in the therapy of intoxications. Toxicol Lett 127(1–3):299–305
Kretzschmar M, Pfeiffer L, Schmidt C, Schirrmeister W (1998) Plasma levels of glutathione, alpha-tocopherol and lipid peroxides in polytraumatized patients; evidence for a stimulating effect of TNF alpha on glutathione synthesis. Exp Toxicol Pathol 50(4–6):477–483
Kupczyk M, Kuna P (2002) Mucolytics in acute and chronic respiratory tract disorders. II. Uses for treatment and antioxidant properties. Pol Merkuriusz Lek 12(69):248–252
Lamson DW, Brignall MS (2000) The use of nebulized glutathione in the treatment of emphysema: a case report [In Process Citation]. Altern Med Rev 5(5):429–431
Lands LC, Grey VL, Grenier C (2000) Total plasma antioxidant capacity in cystic fibrosis. Pediatr Pulmonol 29(2):81–87
Lang CA, Naryshkin S, Schnieder DL, Mills BJ, Lindeman RD (1992) Low blood glutathione in healthy aging adults. J Lab Clin Med 120(5):720–725
LaRowe SD, Mardikian P, Malcolm R, Myrick H, Kalivas P, McFarland K, Saladin M, McRae A, Brady K (2006) Safety and tolerability of N-acetylcysteine in cocaine-dependent individuals. Am J Addict 15(1):105–110
Larrauri A, Fabra R, Gomez-Lechon MJ, Trullenque R, Castell JV (1987) Toxicity of paracetamol in human hepatocytes. Comparison of the protective effects of sulfhydryl compounds acting as glutathione precursors. Mol Toxicol 1(4):301–311
Larsen LC, Fuller SH (1996) Management of acetaminophen toxicity. Am Fam Physician 53(1):185–190
Laurent T, Markert M, Feihl F, Schaller MD, Perret C (1996) Oxidant-antioxidant balance in granulocytes during ARDS. Effect of N-acetylcysteine. Chest 109(1):163–166
Lauterburg BH, Corcoran GB, Mitchell JR (1983) Mechanism of action of N-acetylcysteine in the protection against the hepatotoxicity of acetaminophen in rats in vivo. J Clin Invest 71(4):980–991
Lauterburg BH, Velez ME (1988) Glutathione deficiency in alcoholics: risk factor for paracetamol hepatotoxicity. Gut 29:1153–1157
Lee WM (1993) Drug-induced hepatotoxicity. Aliment Pharmacol Ther 7(5):477–485
Lee WM (1995) Drug-induced hepatotoxicity. N Engl J Med 333(17):1118–1127
Lee WM (1996) Management of acute liver failure. Semin Liver Dis 16(4):369–378
Lenhartz H, Ndasi R, Anninos A, Botticher D, Mayatepek E, Tetanye E, Leichsenring M (1998) The clinical manifestation of the kwashiorkor syndrome is related to increased lipid peroxidation. J Pediatr 132(5):879–881
Listed NA (1980) Acetylcysteine (Parvolex) for paracetamol poisoning. Drug Ther Bull 18(21):81–82
Listed NA (2000) N-acetylcysteine. Altern Med Rev 5(5):467–471
Loguercio C, Nardi G, Argenzio F, Aurilio C, Petrone E, Grella A, Del Vecchio Blanco C, Coltorti M (1994) Effect of S-adenosyl-L-methionine administration on red blood cell cysteine and glutathione levels in alcoholic patients with and without liver disease. Alcohol Alcohol 29(5):597–604
Lou MF, Dickerson JE Jr, Tung WH, Wolfe JK, Chylack LT Jr (1999) Correlation of nuclear color and opalescence with protein S-thiolation in human lenses. Exp Eye Res 68(5):547–552
Louwerse ES, Weverling GJ, Bossuyt PM, Meyjes FE, de Jong JM (1995) Randomized, double-blind, controlled trial of acetylcysteine in amyotrophic lateral sclerosis. Arch Neurol 52(6):559–564
Lyons L, Studdiford JS, Sommaripa AM (1977) Treatment of acetaminophen overdosage with N-acetylcysteine. N Engl J Med 296(3):174–175
MacNeill BDHS, Bazari H, Patton KK, Colon-Hernadez P, DeJoseph D, Jang IK (2003) Prophylaxis of contrast-induced nephropathy in patients undergoing coronary angiography. Catheter Cardiovas Interv 60(4):458–461
Macy AM (1979) Preventing hepatotoxicity in acetaminophen overdose. Am J Nurs 79(2):301–303
Mangione S, Patel DD, Levin BR, Fiel SB (1994) Erythrocytic glutathione in cystic fibrosis. A possible marker of pulmonary dysfunction. Chest 105(5):1470–1473
Marenzi G, Assanelli E, Marana I, Lauri G, Campodonico J, Grazi M, De Metrio M, Galli S, Fabbiocchi F, Montorsi P, Veglia F, Bartorelli AL (2006) N-acetylcysteine and contrast-induced nephropathy in primary angioplasty. N Engl J Med 354(26):2773–2782
Marini U, Visconti G, Spotti D, Geniram A (1980) Controlled endoscopic study on gastroduodenal safety of acetylcysteine after oral administration. Eur J Respir Dis Suppl 111:147–150
Marquardt ED (1977) Treatment of acetaminophen toxicity. Am J Hosp Pharm 34(8):805–806
Marshall RJ, Scott KC, Hill RC, Lewis DD, Sundstrom D, Jones GL, Harper J (2002) Supplemental vitamin C appears to slow racing greyhounds. J Nutr 132(6 Suppl 2):1616S–1621S
Martin DS, Willis SE, Cline DM (1990) N-acetylcysteine in the treatment of human arsenic poisoning. J Am Board Fam Pract 3(4):293–296
Marui N, Offermann MK, Swerlick R, Kunsch C, Rosen CA, Ahmad M, Alexander RW, Medford RM (1993) Vascular cell adhesion molecule-1 (VCAM-1) gene transcription and expression are regulated through an antioxidant-sensitive mechanism in human vascular endothelial cells. J Clin Invest 92(4):1866–1874. https://doi.org/10.1172/JCI116778
Maurer WG, Zeisler J (1978) Intravenous acetylcysteine as treatment for acetaminophen overdose. Am J Hosp Pharm 35(9):1025, 1030
Maurice MM, Nakamura H, van der Voort EAM, van Vliet AI, Staal FJT, Tak P-P, Breedveld FC, Verweij CL (1997) Evidence for the role of an altered redox state in hyporesponsiveness of synovial T cells in rheumatoid arthritis. J Immunol 158(3):1458–1465
Mayaud C, Lentschner C, Bouchoucha S, Marsac J (1980) Thiamphenicol glycinate acetylcysteinate in the treatment of acute respiratory infections with mucostasis. Eur J Respir Dis Suppl 111:70–73
McGavin C (1985) Oral N-acetylcysteine and exacerbation rates in patients with chronic bronchitis and severe airways obstruction. British Thoracic Society Research Committee. Thorax 40(11):832–835
McKay DL, Perrone G, Rasmussen H, Dallal G, Hartman W, Cao G, Prior RL, Roubenoff R, Blumberg JB (2000) The effects of a multivitamin/mineral supplement on micronutrient status, antioxidant capacity and cytokine production in healthy older adults consuming a fortified diet. J Am Coll Nutr 19(5):613–621
Medved I, Brown MJ, Bjorksten AR, Leppik JA, Sostaric S, McKenna MJ (2003) N-acetylcysteine infusion alters blood redox status but not time to fatigue during intense exercise in humans. J Appl Physiol 94(4):1572–1582
Medved I, Brown MJ, Bjorksten AR, McKenna MJ (2004a) Effects of intravenous N-acetylcysteine infusion on time to fatigue and potassium regulation during prolonged cycling exercise. J Appl Physiol 96(1):211–217
Medved I, Brown MJ, Bjorksten AR, Murphy KT, Petersen AC, Sostaric S, Gong X, McKenna MJ (2004b) N-acetylcysteine enhances muscle cysteine and glutathione availability and attenuates fatigue during prolonged exercise in endurance-trained individuals. J Appl Physiol 97:1477
Meister A, Anderson ME, Hwang O (1986) Intracellular cysteine and glutathione delivery systems. J Am Coll Nutr 5(2):137–151
Melillo G, Chiummariello A, Scala G (1966) On the use of a new molecular combination of acetylcysteine with thiamphenicol glycinate in bronchopulmonary suppurations. G Ital Chemioter 13(1):156–160
Meyer A, Buhl R, Kampf S, Magnussen H (1995) Intravenous N-acetylcysteine and lung glutathione of patients with pulmonary fibrosis and normals. Am J Respir Crit Care Med 152(3):1055–1060
Meyer A, Buhl R, Magnussen H (1994) The effect of oral N-Acetylcysteine on lung glutathione levels in idiopathic pulmonary fibrosis. Eur Respir J 7(3):431–436
Michelet F, Gueguen R, Leroy P, Wellman M, Nicolas A, Siest G (1995) Blood and plasma glutathione measured in healthy subjects by HPLC: relation to sex, aging, biological variables, and life habits. Clin Chem 41(10):1509–1517
Milewski J, Rydzewska G, Degowska M, Kierzkiewicz M, Rydzewski A (2006) N-acetylcysteine does not prevent post-endoscopic retrograde cholangiopancreatography hyperamylasemia and acute pancreatitis. World J Gastroenterol 12(23):3751–3755
Millar AB, Pavia D, Agnew JE, Lopez-Vidriero MT, Lauque D, Clarke SW (1985) Effect of oral N-acetylcysteine on mucus clearance. Br J Dis Chest 79(3):262–266
Miller LF, Rumack BH (1983) Clinical safety of high oral doses of acetylcysteine. Semin Oncol 10(1 Suppl 1):76–85
Miller M (1975) Clinical experimentation using a combination with antibiotic and mucolytic activity in the treatment of respiratory and oto-rhino-laryngologic infections with allergic components. Brux Med 55(6):349–351
Miralles-Barrachina O, Savoye G, Belmonte-Zalar L, Hochain P, Ducrotte P, Hecketsweiler B, Lerebours E, Dechelotte P (1999) Low levels of glutathione in endoscopic biopsies of patients with Crohn’s colitis: the role of malnutrition. Clin Nutr 18(5):313–317
Mitchell JR, Corcoran GB, Smith CV, Hughes H, Lauterburg BH (1981) Alkylation and peroxidation injury from chemically reactive metabolites. Adv Exp Med Biol 136(Pt A):199–223
Mitchell JR, Thorgeirsson SS, Potter WZ, Jollow DJ, Keiser H (1974) Acetaminophen-induced hepatic injury: protective role of glutathione in man and rationale for therapy. Clin Pharmacol Ther 16(4):676–684
Moberly JB, Logan J, Borum PR, Story KO, Webb LE, Jassal SV, Mupas L, Rodela H, Alghamdi GA, Moran JE, Wolfson M, Martis L, Oreopoulos DG (1998) Elevation of whole-blood glutathione in peritoneal dialysis patients by L-2-oxothiazolidine-4-carboxylate, a cysteine prodrug (Procysteine(R)). J Am Soc Nephrol 9(6):1093–1099
Molnar Z, MacKinnon KL, Shearer E, Lowe D, Watson ID (1998) The effect of N-acetylcysteine on total serum anti-oxidant potential and urinary albumin excretion in critically ill patients. Intensive Care Med 24(3):230–235
Molnar Z, Shearer E, Lowe D (1999) N-Acetylcysteine treatment to prevent the progression of multisystem organ failure: a prospective, randomized, placebo-controlled study. Crit Care Med 27(6):1100–1104
Molnar Z, Szakmany T, Koszegi T (2003) Prophylactic N-acetylcysteine decreases serum CRP but not PCT levels and microalbuminuria following major abdominal surgery. A prospective, randomised, double-blinded, placebo-controlled clinical trial. Intensive Care Med 29(5):749–755
Montanini S, Sinardi D, Pratico C, Sinardi AU, Trimarchi G (1999) Use of acetylcysteine as the life-saving antidote in Amanita phalloides (Death cap) poisoning – case report on 11 patients. Arzneim Forsch Drug Res 49(12):1044–1047
Moriuchi H, Zaha M, Fukumoto T, Yuizono T (1998) Activation of polymorphonuclear leukocytes in oleic acid-induced lung injury. Intensive Care Med 24(7):709–715
Morrison JA, Jacobsen DW, Sprecher DL, Robinson K, Khoury P, Daniels SR (1999) Serum glutathione in adolescent males predicts parental coronary heart disease. Circulation 100(22):2244–2247
Moss M, Guidot DM, Wong-Lambertina M, Ten Hoor T, Perez RL, Brown LAS (2000) The effects of chronic alcohol abuse on pulmonary glutathione homeostasis. Am J Respir Crit Care Med 161(2):414–419
Murakami K, Kondo T, Ohtsuka Y, Fujiwara Y, Shimada M, Kawakami Y (1989) Impairment of glutathione metabolism in erthrocytes from patients with diabetes mellitus. Metab Clin Exp 38:753–758
Mutimer D, Neuberger J (1993) Acute liver failure: improving outcome despite a paucity of treatment options. Q J Med 86(7):409–411
Mutlu-Turkoglu U, Ademoglu E, Ibrahimoglu L, Aykac-Toker G, Uysal M (1998) Imbalance between lipid peroxidation and antioxidant status in preeclampsia. Gynecol Obstet Investig 46(1):37–40
N’Dow J, Robson CN, Matthews JN, Neal DE, Pearson JP (2001) Reducing mucus production after urinary reconstruction: a prospective randomized trial. J Urol 165(5):1433–1440
Nakagawa Y, Akao Y, Morikawa H, Hirata I, Katsu K, Naoe T, Ohishi N, Yagi K (2002) Arsenic trioxide-induced apoptosis through oxidative stress in cells of colon cancer cell lines. Life Sci 70(19):2253–2269
Nakamura H, De Rosa SC, Yodoi J, Holmgren A, Ghezzi P, Herzenberg LA (2001) Chronic elevation of plasma thioredoxin: Inhibition of chemotaxis and curtailment of life expectancy in AIDS. Proc Natl Acad Sci U S A 98(5):2688–2693
Nakamura H, Masutani H, Yodoi J (2002) Redox imbalance and its control in HIV infection. Antioxid Redox Signal 4(3):455–464
Nallamothu BK, Shojania KG, Saint S, Hofer TP, Humes HD, Moscucci M, Bates ER (2004) Is acetylcysteine effective in preventing contrast-related nephropathy? A meta-analysis. Am J Med 117(12):938–947
Naziroglu M, Cay M (2001) Protective role of intraperitoneally administered vitamin E and selenium on the antioxidative defense mechanisms in rats with diabetes induced by streptozotocin. Biol Trace Elem Res 79(2):149–159
Nielsen HB (1999) N-acetylcysteine. Ugeskr Laeger 161(31):4424
Nielsen HB, Kharazmi A, Bolbjerg ML, Poulsen HE, Pedersen BK, Secher NH (2001) N-acetylcysteine attenuates oxidative burst by neutrophils in response to ergometer rowing with no effect on pulmonary gas exchange. Int J Sports Med 22(4):256–260
Nuttall SL, Dunne F, Kendall MJ, Martin U (1999) Age-independent oxidative stress in elderly patients with non-insulin-dependent diabetes mellitus. QJM 92(1):33–38
Oldemeyer JB, Biddle WP, Wurdeman RL, Mooss AN, Cichowski E, Hilleman DE (2003) Acetylcysteine in the prevention of contrast-induced nephropathy after coronary angiography. Am Heart J 146(6):E23
Olivieri D, Marsico SA, Del Donno M (1985) Improvement of mucociliary transport in smokers by mucolytics. Eur J Respir Dis Suppl 139:142–145
Ortolani O, Conti A, De Gaudio AR, Moraldi E, Novelli GP (2002) Glutathione and N-acetylcysteine in the prevention of free-radical damage in the initial phase of septic shock. Recenti Prog Med 93(2):125–129
Ostapowicz G, Fontana RJ, Schiodt FV, Larson A, Davern TJ, Han SH, McCashland TM, Shakil AO, Hay JE, Hynan L, Crippin JS, Blei AT, Samuel G, Reisch J, Lee WM (2002) Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med 137(12):947–954
Ostapowicz G, Lee WM (2000) Acute hepatic failure: a western perspective. J Gastroenterol Hepatol 15(5):480–488
Ovesen T, Felding JU, Tommerup B, Schousboe LP, Petersen CG (2000) Effect of N-acetylcysteine on the incidence of recurrence of otitis media with effusion and re-insertion of ventilation tubes. Acta Otolaryngol 120:79–81
Ozaras R, Tahan V, Aydin S, Uzun H, Kaya S, Senturk H (2003) N-acetylcysteine attenuates alcohol-induced oxidative stress in the rat. World J Gastroenterol 9(1):125–128
Pace BS, Shartava A, Pack-Mabien A, Mulekar M, Ardia A, Goodman SR (2003) Effects of N-acetylcysteine on dense cell formation in sickle cell disease. Am J Hematol 73(1):26–32
Pacht ER, Diaz P, Clanton T, Hart J, Gadek JE (1997) Alveolar fluid glutathione decreases in asymptomatic HIV-seropositive subjects over time. Chest 112(3):785–788
Pacht ER, Timerman AP, Lykens MG, Merola AJ (1991) Deficiency of alveolar fluid glutathione in patients with sepsis and the adult respiratory distress syndrome. Chest 100(5):1397–1403
Pannu N, Manns B, Lee H, Tonelli M (2004) Systematic review of the impact of N-acetylcysteine on contrast nephropathy. Kidney Int 65(4):1366–1374
Parr GD, Huitson A (1987) Oral Fabrol (oral N-acetyl-cysteine) in chronic bronchitis. Br J Dis Chest 81(4):341–348
Paterson RL, Galley HF, Webster NR (2003) The effect of N-acetylcysteine on nuclear factor-kappa B activation, interleukin-6, interleukin-8, and intercellular adhesion molecule-1 expression in patients with sepsis. Crit Care Med 31(11):2574–2578. https://doi.org/10.1097/01.ccm.0000089945.69588.18
Peake SL, Moran JL, Leppard PI (1996) N-acetyl-L-cysteine depresses cardiac performance in patients with septic shock. Crit Care Med 24(8):1302–1310
Pena LR, Hill DB, McClain CJ (1999) Treatment with glutathione precursor decreases cytokine activity. J Parenter Enter Nutr 23(1):1–6
Pendyala L, Schwartz G, Bolanowska-Higdon W, Hitt S, Zdanowicz J, Murphy M, Lawrence D, Creaven PJ (2001) Phase I/pharmacodynamic study of N-acetylcysteine/oltipraz in smokers: early termination due to excessive toxicity. Cancer Epidemiol Biomark Prev 10(3):269–272
Perez RS, Zuurmond WW, Bezemer PD, Kuik DJ, van Loenen AC, de Lange JJ, Zuidhof AJ (2003) The treatment of complex regional pain syndrome type I with free radical scavengers: a randomized controlled study. Pain 102(3):297–307
Perry HE, Shannon MW (1998) Efficacy of oral versus intravenous N-acetylcysteine in acetaminophen overdose: results of an open-label, clinical trial [see comments]. J Pediatr 132(1):149–152
Peters WH, Roelofs HM, Hectors MP, Nagengast FM, Jansen JB (1993) Glutathione and glutathione S-transferases in Barrett’s epithelium. Br J Cancer 67(6):1413–1417
Peterson JD, Herzenberg LA, Vasquez K, Waltenbaugh C (1998) Glutathione levels in antigen-presenting cells modulate Th1 versus Th2 response patterns. Proc Natl Acad Sci U S A 95(6):3071–3076
Peterson RG, Rumack BH (1977a) N-acetylcysteine for acetaminophen overdosage (cont.) N Engl J Med 296(9):515
Peterson RG, Rumack BH (1977b) Treating acute acetaminophen poisoning with acetylcysteine. JAMA 237(22):2406–2407
Peterson RG, Rumack BH (1978) Toxicity of acetaminophen overdose. J Am Coll Emerg Physicians 7(5):202–205
Pineda-Molina E, Klatt P, Vazquez J, Marina A, Garcia de Lacoba M, Perez-Sala D, Lamas S (2001) Glutathionylation of the p50 subunit of NF-kappaB: a mechanism for redox-induced inhibition of DNA binding. Biochemistry 40(47):14134–14142
Ponnappan U (2002) Ubiquitin-proteasome pathway is compromised in CD45RO+ and CD45RA+ T lymphocyte subsets during aging. Exp Gerontol 37(2–3):359–367
Porsio A, Borgia M (1970) Intravenous administration of acetylcysteine: clinical experience with its tolerance and action. Clin Ter 55(2):123–132
Prasad A, Andrews NP, Padder FA, Husain M, Quyyumi AA (1999) Glutathione reverses endothelial dysfunction and improves nitric oxide bioavailability. J Am Coll Cardiol 34(2):507–514
Prescott LF (1983) New approaches in managing drug overdosage and poisoning. Br Med J (Clin Res Ed) 287(6387):274–276
Prescott LF, Critchley JA (1983) The treatment of acetaminophen poisoning. Annu Rev Pharmacol Toxicol 23:87–101
Prescott LF, Park J, Ballantyne A, Adriaenssens P, Proudfoot AT (1977) Treatment of paracetamol (acetaminophen) poisoning with N- acetylcysteine. Lancet 2(8035):432–434
Pulle DF, Glass P, Dulfano MJ (1970) A controlled study of the safety and efficacy of acetylcysteine-isoproterenol combination. Curr Ther Res Clin Exp 12(8):485–492
Rahman I, Skwarska E, Henry M, Davis M, O’Connor CM, FitzGerald MX, Greening A, MacNee W (1999) Systemic and pulmonary oxidative stress in idiopathic pulmonary fibrosis. Free Radic Biol Med 27(1–2):60–68
Rank N, Michel C, Haertel C, Lenhart A, Welte M, Meier-Hellmann A, Spies C (2000) N-acetylcysteine increases liver blood flow and improves liver function in septic shock patients: results of a prospective, randomized, double-blind study. Crit Care Med 28(12):3799–3807
Rashid ST, Salman M, Myint F, Baker DM, Agarwal S, Sweny P, Hamilton G (2004) Prevention of contrast-induced nephropathy in vascular patients undergoing angiography: a randomized controlled trial of intravenous N-acetylcysteine. J Vasc Surg 40(6):1136–1141
Rasmussen JB, Glennow C (1988) Reduction in days of illness after long-term treatment with N-acetylcysteine controlled-release tablets in patients with chronic bronchitis. Eur Respir J 1(4):351–355
Ratjen F, Wonne R, Posselt HG, Stover B, Hofmann D, Bender SW (1985) A double-blind placebo controlled trial with oral ambroxol and N-acetylcysteine for mucolytic treatment in cystic fibrosis. Eur J Pediatr 144(4):374–378
Reid M, Badaloo A, Forrester T, Morlese JF, Frazer M, Heird WC, Jahoor F (2000) In vivo rates of erythrocyte glutathione synthesis in children with severe protein-energy malnutrition. Am J Physiol Endocrinol Metab 278(3):E405–E412
Reid M, Jahoor F (2001) Glutathione in disease. Curr Opin Clin Nutr Metab Care 4(1):65–71
Reinhart K, Spies CD, Meier-Hellmann A, Bredle DL, Hannemann L, Specht M, Schaffartzik W (1995) N-acetylcysteine preserves oxygen consumption and gastric mucosal pH during hyperoxic ventilation. Am J Respir Crit Care Med 151(3 Pt 1):773–779
Repetto M, Reides C, Carretero MLG, Costa M, Griemberg G, Llesuy S (1996) Oxidative stress in blood of HIV infected patients. Clin Chim Acta 255(2):107–117
Riise GC, Larsson S, Larsson P, Jeansson S, Andersson BA (1994) The intrabronchial microbial flora in chronic bronchitis patients: a target for N-acetylcysteine therapy? Eur Respir J 7(1):94–101
Ristoff E, Larsson A (2002) Oxidative stress in inborn errors of metabolism: lessons from glutathione deficiency. J Inherit Metab Dis 25(3):223–226
Ristoff E, Mayatepek E, Larsson A (2001) Long-term clinical outcome in patients with glutathione synthetase deficiency. J Pediatr 139(1):79–84. https://doi.org/10.1067/mpd.2001.114480
Rizvi SI, Zaid MA (2001) Intracellular reduced glutathione content in normal and type 2 diabetic erythrocytes: effect of insulin and (-)epicatechin. J Physiol Pharmacol 52(3):483–488
Roederer M, Ela SW, Staal FJT, Herzenberg LA, Herzenberg LA (1992) N-Acetylcysteine: a new approach to anti-HIV therapy. AIDS Res Hum Retroviruses 8(2):209–217
Roederer M, Staal FJ, Raju PA, Ela SW, Herzenberg LA (1990) Cytokine-stimulated human immunodeficiency virus replication is inhibited by N-acetyl-L-cysteine. Proc Natl Acad Sci U S A 87(12):4884–4888
Roederer M, Staal FJT, Osada H, Herzenberg LA, Herzenberg LA (1991) CD4 and CD8 T cells with high intracellular glutathione levels are selectively lost as the HIV infection progresses. Int Immunol 3(9):933–937
Roum JH, Borok Z, McElvaney NG, Grimes GJ, Bokser AD, Buhl R, Crystal RG (1999) Glutathione aerosol suppresses lung epithelial surface inflammatory cell-derived oxidants in cystic fibrosis. J Appl Physiol 87(1):438–443
Roum JH, Buhl R, Mcelvaney NG, Borok Z, Crystal RG (1993) Systemic deficiency of glutathione in cystic fibrosis. J Appl Physiol 75(6):2419–2424
Ruan EA, Rao S, Burdick JS, Stryker SJ, Telford GL, Otterson MF, Opara EC, Koch TR (1997) Glutathione levels in chronic inflammatory disorders of the human colon. Nutr Res 17(3):463–473
Ruffmann R, Wendel A (1991) GSH rescue by N-acetylcysteine. Klin Wochenschr 69(18):857–862
Rumack BH (1984) Acetaminophen overdose in young children. Treatment and effects of alcohol and other additional ingestants in 417 cases. Am J Dis Child 138(5):428–433
Rumack BH (1986) Acetaminophen overdose in children and adolescents. Pediatr Clin N Am 33(3):691–701
Rumack BH (2002) Acetaminophen hepatotoxicity: the first 35 years. J Toxicol Clin Toxicol 40(1):3–20
Rumack BH, Peterson RC, Koch GG, Amara IA (1981) Acetaminophen overdose. 662 cases with evaluation of oral acetylcysteine treatment. Arch Intern Med 141(3 Spec No):380–385
Saitoh M, Nishitoh H, Fujii M, Takeda K, Tobiume K, Sawada Y, Kawabata M, Miyazono K, Ichijo H (1998) Mammalian thioredoxin is a direct inhibitor of apoptosis signal-regulating kinase (ASK) 1. EMBO J 17(9):2596–2606. https://doi.org/10.1093/emboj/17.9.2596
Salgia AD, Kosnik SD (1999) When acetaminophen use becomes toxic. Treating acute accidental and intentional overdose. Postgrad Med 105(4):81–84, 87, 90
Samiec PS, Drews-Botsch C, Flagg EW, Kurtz JC, Sternberg P, Reed RL, Jones DP (1998) Glutathione in human plasma: decline in association with aging, age-related macular degeneration, and diabetes. Free Radic Biol Med 24(5):699–704
Sandalova T, Zhong L, Lindqvist Y, Holmgren A, Schneider G (2001) Three-dimensional structure of a mammalian thioredoxin reductase: implications for mechanism and evolution of a selenocysteine-dependent enzyme. Proc Natl Acad Sci U S A 98(17):9533–9538. https://doi.org/10.1073/pnas.171178698
Sandberg K, Fellman V, Stigson L, Thiringer K, Hjalmarson O (2004) N-acetylcysteine administration during the first week of life does not improve lung function in extremely low birth weight infants. Biol Neonate 86(4):275–279
Sandhu C, Belli AM, Oliveira DB (2006) The role of N-acetylcysteine in the prevention of contrast-induced nephrotoxicity. Cardiovasc Intervent Radiol 29(3):344–347
Sano M, Ernesto C, Thomas RG, Klauber MR, Schafer K, Grundman M, Woodbury P, Growdon J, Cotman CW, Pfeiffer E, Schneider LS, Thal LJ (1997) A controlled trial of selegiline, alpha-tocopherol, or both as treatment for Alzheimer’s disease. The Alzheimer’s Disease Cooperative Study. N Engl J Med 336(17):1216–1222
Sasazuki S, Kodama H, Yoshimasu K, Liu Y, Washio M, Tanaka K, Tokunaga S, Kono S, Arai H, Doi Y, Kawano T, Nakagaki O, Takada K, Koyanagi S, Hiyamuta K, Nii T, Shirai K, Ideishi M, Arakawa K, Mohri M, Takeshita A (2000) Relation between green tea consumption and the severity of coronary atherosclerosis among Japanese men and women. Ann Epidemiol 10(6):401–408
Sastre J, Pallardo FV, Garcia de la Asuncion J, Vina J (2000) Mitochondria, oxidative stress and aging. Free Radic Res 32(3):189–198
Sastre J, Pallardo FV, Vina J (1996) Glutathione, oxidative stress and aging. Age 19(4):129–139
Saugstad OD (1997) Bronchopulmonary dysplasia and oxidative stress: are we closer to an understanding of the pathogenesis of BPD? Acta Paediatr 86(12):1277–1282
Saxena S, Kumar D, Srivastava P, Khanna VK, Seth PK (1999) Low levels of platelet glutathione in Eales’ disease. Med Sci Res 27(9):625–626
Schmidinger M, Budinsky AC, Wenzel C, Piribauer M, Brix R, Kautzky M, Oder W, Locker GJ, Zielinski CC, Steger GG (2000) Glutathione in the prevention of cisplatin induced toxicities. A prospectively randomized pilot trial in patients with head and neck cancer and non small cell lung cancer. Wien Klin Wochenschr 112(14):617–623
Schmidt AM, Hori O, Chen JX, Li JF, Crandall J, Zhang J, Cao R, Yan SD, Brett J, Stern D (1995) Advanced glycation endproducts interacting with their endothelial receptor induce expression of vascular cell adhesion molecule-1 (VCAM-1) in cultured human endothelial cells and in mice. A potential mechanism for the accelerated vasculopathy of diabetes. J Clin Invest 96(3):1395–1403
Schmidt LE, Knudsen TT, Dalhoff K, Bendtsen F (2002) Effect of acetylcysteine on prothrombin index in paracetamol poisoning without hepatocellular injury. Lancet 360(9340):1151–1152
Schnackenberg LK, Chen M, Sun J, Holland RD, Dragan Y, Tong W, Welsh W, Beger RD (2009) Evaluations of the trans-sulfuration pathway in multiple liver toxicity studies. Toxicol Appl Pharmacol 235(1):25–32. https://doi.org/10.1016/j.taap.2008.11.015
Scholze A, Rinder C, Beige J, Riezler R, Zidek W, Tepel M (2004) Acetylcysteine reduces plasma homocysteine concentration and improves pulse pressure and endothelial function in patients with end-stage renal failure. Circulation 109(3):369–374
Schulz JB, Lindenau J, Seyfried J, Dichgans J (2000) Glutathione, oxidative stress and neurodegeneration. Eur J Biochem 267(16):4904–4911
Seema KR, Mandal RN, Tandon A, Randhawa VS, Mehta G, Batra S, Ray GN, Kapoor AK (1999) Serum TNF-alpha and free radical scavengers in neonatal septicemia. Indian J Pediatr 66(4):511–516
Sellers EM, Freedman F (1981) Treatment of acetaminophen poisoning. Can Med Assoc J 125(8):827–829
Selwa LM (1999) N-acetylcysteine therapy for Unverricht-Lundborg disease. Neurology 52(2):426–427
Sha SH, Schacht J (2000) Antioxidants attenuate gentamicin-induced free radical formation in vitro and ototoxicity in vivo: D-methionine is a potential protectant. Hear Res 142(1–2):34–40
Shan X, Aw TY, Jones DP (1990) Glutathione-dependent protection against oxidative injury. Pharmacol Ther 47:61–71
Shapiro BL, Smith QT, Warick WJ (1975) Serum glutathione reductase and cystic fibrosis. Pediatr Res 9(12):885–888
Shapiro BL, Smith QT, Warwick WJ (1973) Red cell glutathione and glutathione reductase in cystic fibrosis. Proc Soc Exp Biol Med 144(1):181–183
Shenton D, Perrone G, Quinn KA, Dawes IW, Grant CM (2002) Regulation of protein S-thiolation by glutaredoxin 5 in the yeast Saccharomyces cerevisiae. J Biol Chem 277(19):16853–16859. https://doi.org/10.1074/jbc.M200559200
Shriner K, Goetz MB (1992) Severe hepatotoxicity in a patient receiving both acetaminophen and zidovudine. Am J Med 93(1):94–96
Shyu KG, Cheng JJ, Kuan P (2002) Acetylcysteine protects against acute renal damage in patients with abnormal renal function undergoing a coronary procedure. J Am Coll Cardiol 40(8):1383–1388
Sido B, Hack V, Hochlehnert A, Lipps H, Herfarth C, Droge W (1998) Impairment of intestinal glutathione synthesis in patients with inflammatory bowel disease. Gut 42(4):485–492
Skurnick JH, Bogden JD, Baker H, Kemp FW, Sheffet A, Quattrone G, Louria DB (1996) Micronutrient profiles in HIV-1-infected heterosexual adults. J Acquir Immune Defic Syndr 12(1):75–83
Slattery JT, McRorie TI, Reynolds R, Kalhorn TF, Kharasch ED, Eddy AC (1989) Lack of effect of cimetidine on acetaminophen disposition in humans. Clin Pharmacol Ther 46(5):591–597
Slattery JT, Wilson JM, Kalhorn TF, Nelson SD (1987) Dose-dependent pharmacokinetics of acetaminophen: evidence of glutathione depletion in humans. Clin Pharmacol Ther 41:413–418
Smilkstein MJ, Bronstein AC, Linden C, Augenstein WL, Kulig KW, Rumack BH (1991) Acetaminophen overdose: a 48-hour intravenous N-acetylcysteine treatment protocol. Ann Emerg Med 20(10):1058–1063
Smilkstein MJ, Knapp GL, Kulig KW, Rumack BH (1988) Efficacy of oral N-acetylcysteine in the treatment of acetaminophen overdose. Analysis of the national multicenter study (1976 to 1985). N Engl J Med 319(24):1557–1562
Smith CV, Hansen TN, Martin NE, McMicken HW, Elliott SJ (1993) Oxidant stress responses in premature infants during exposure to hyperoxia. Pediatr Res 34(3):360–365
Smith CV, Rogers LK, Rabin RL, Maldonado YA, Herzenberg LA, Herzenberg LA, Petru A (1994) Effects of human immunodeficiency virus (HIV) infection on plasma glutathione status in children. Pediatr Res 35:196A. (Abstract #1163)
Sochman J (2002) N-acetylcysteine in acute cardiology: 10 years later: what do we know and what would we like to know? J Am Coll Cardiol 39(9):1422–1428
Song JJ, Rhee JG, Suntharalingam M, Walsh SA, Spitz DR, Lee YJ (2002) Role of glutaredoxin in metabolic oxidative stress. Glutaredoxin as a sensor of oxidative stress mediated by H2O2. J Biol Chem 277(48):46566–46575. https://doi.org/10.1074/jbc.M206826200
Spada C, Treitinger A, Reis M, Masokawa IY, Verdi JC, Luiz MC, Silveira MV, Michelon CM, Avila-Junior S, Gil DO, Ostrowskyl S (2002) The effect of N-acetylcysteine supplementation upon viral load, CD4, CD8, total lymphocyte count and hematocrit in individuals undergoing antiretroviral treatment. Clin Chem Lab Med 40(5):452–455
Spapen H, Zhang H, Demanet C, Vleminckx W, Vincent JL, Huyghens L (1998) Does N-acetyl-L-cysteine influence cytokine response during early human septic shock? Chest 113(6):1616–1624
Spies C, Giese C, Meier-Hellmann A, Specht M, Hannemann L, Schaffartzik W, Reinhart K (1996) The effect of prophylactically administered n-acetylcysteine on clinical indicators for tissue oxygenation during hyperoxic ventilation in cardiac risk patients. Anaesthesist 45(4):343–350
Spies CD, Reinhart K, Witt I, Meier-Hellmann A, Hannemann L, Bredle DL, Schaffartzik W (1994) Influence of N-acetylcysteine on indirect indicators of tissue oxygenation in septic shock patients: results from a prospective, randomized, double-blind study. Crit Care Med 22(11):1738–1746
Sprietsma JE (1999) Modern diets and diseases: NO-zinc balance. Under Th1, zinc and nitrogen monoxide (NO) collectively protect against viruses, AIDS, autoimmunity, diabetes, allergies, asthma, infectious diseases, atherosclerosis and cancer. Med Hypotheses 53(1):6–16
Sprince H (1985) Protective action of sulfur compounds against aldehyde toxicants of cigarette smoke. Eur J Respir Dis Suppl 139:102–112
Sprince H, Parker CM, Smith GG, Gonzales LJ (1975) Protective action of ascorbic acid and sulfur compounds against acetaldehyde toxicity: implications in alcoholism and smoking. Agents Actions 5(2):164–173
Staal FJ, Ela SW, Roederer M, Anderson MT, Herzenberg LA (1992a) Glutathione deficiency and human immunodeficiency virus infection. Lancet 339(8798):909–912
Staal FJ, Roederer M, Herzenberg LA (1990) Intracellular thiols regulate activation of nuclear factor kappa B and transcription of human immunodeficiency virus. Proc Natl Acad Sci U S A 87(24):9943–9947
Staal FJ, Roederer M, Israelski DM, Bubp J, Mole LA, McShane D, Deresinski SC, Ross W, Sussman H, Raju PA et al (1992b) Intracellular glutathione levels in T cell subsets decrease in HIV-infected individuals. AIDS Res Hum Retrovir 8(2):305–311
Stafanger G, Garne S, Howitz P, Morkassel E, Koch C (1988) The clinical effect and the effect on the ciliary motility of oral N-acetylcysteine in patients with cystic fibrosis and primary ciliary dyskinesia. Eur Respir J 1(2):161–167
Stafanger G, Koch C (1989) N-acetylcysteine in cystic fibrosis and Pseudomonas aeruginosa infection: clinical score, spirometry and ciliary motility. Eur Respir J 2(3):234–237
Stewart DM, Dillman RO, Kim HS, Stewart K (1979) Acetaminophen overdose: a growing health care hazard. Clin Toxicol 14(5):507–513
Stey C, Steurer J, Bachmann S, Medici TC, Tramer MR (2000) The effect of oral N-acetylcysteine in chronic bronchitis: a quantitative systematic review [In Process Citation]. Eur Respir J 16(2):253–262
Stiksa G, Nemcek K, Melin S (1984) Effects of inhaled N-acetylcysteine in combination with terbutaline. Eur J Respir Dis 65(4):278–282
Straface E, Rivabene R, Masella R, Santulli M, Paganelli R, Malorni W (2002) Structural changes of the erythrocyte as a marker of non-insulin-dependent diabetes: protective effects of N-acetylcysteine. Biochem Biophys Res Commun 290(5):1393–1398
Suarez M, Beloqui O, Ferrer JV, Gil B, Qian C, Garcia N, Civeira P, Prieto J (1993) Glutathione depletion in chronic hepatitis C. Int Hepatol Commun 1:215–221
Sulkowski MS, Thomas DL, Chaisson RE, Moore RD (2000) Hepatotoxicity associated with antiretroviral therapy in adults infected with human immunodeficiency virus and the role of hepatitis C or B virus infection. JAMA 283(1):74–80
Sung L, Simons JA, Dayneka NL (1997) Dilution of intravenous N-acetylcysteine as a cause of hyponatremia. Pediatrics 100(3 Pt 1):389–391
Suter PM, Domenighetti G, Schaller M-D, Laverriere M-C, Ritz R, Perret C (1994) N-acetylcysteine enhances recovery from acute lung injury in man. A randomized, double-blind, placebo-controlled clinical study. Chest 105:190–194
Svendsen JH, Klarlund K, Aldershvile J, Waldorff S (1989) N-acetylcysteine modifies the acute effects of isosorbide-5-mononitrate in angina pectoris patients evaluated by exercise testing. J Cardiovasc Pharmacol 13(2):320–323
Szakmany T, Marton S, Molnar Z (2003) Lack of effect of prophylactic N-acetylcysteine on postoperative organ dysfunction following major abdominal tumour surgery: a randomized, placebo-controlled, double-blinded clinical trial. Anaesth Intensive Care 31(3):267–271
Taniguchi N, Higashi T, Sakamoto Y, Meister A (eds) (1989) Glutathione centennial: molecular perspectives and clinical applications. Academic Press, New York
Tatebe S, Sinicrope FA, Kuo MT (2002) Induction of multidrug resistance proteins MRP1 and MRP3 and gamma-glutamylcysteine synthetase gene expression by nonsteroidal anti-inflammatory drugs in human colon cancer cells. Biochem Biophys Res Commun 290(5):1427–1433
Tenenbein M (1984) Hypersensitivity-like reactions to N-acetylcysteine. Vet Hum Toxicol 26(Suppl 2):3–5
Tepel M, van der Giet M, Schwarzfeld C, Laufer U, Liermann D, Zidek W (2000) Prevention of radiographic-contrast-agent-induced reductions in renal function by acetylcysteine. N Engl J Med 343:180–184
Tepel M, van der Giet M, Statz M, Jankowski J, Zidek W (2003) The antioxidant acetylcysteine reduces cardiovascular events in patients with end-stage renal failure. A randomized, controlled trial. Circulation 107:992
Tepel M, Zidek W (2001) Acetylcysteine for radiocontrast nephropathy. Curr Opin Crit Care 7(6):390–392
Tessier D, Khalil A, Fulop T (1999) Effects of an oral glucose challenge on free radicals/antioxidants balance in an older population with type II diabetes. J Gerontol A Biol Sci Med Sci 54(11):M541–M545
Tice JA, Ross E, Coxson PG, Rosenberg I, Weinstein MC, Hunink MG, Goldman PA, Williams L, Goldman L (2001) Cost-effectiveness of vitamin therapy to lower plasma homocysteine levels for the prevention of coronary heart disease: effect of grain fortification and beyond. JAMA 286(8):936–943
Todisco T, Polidori R, Rossi F, Iannacci L, Bruni B, Fedeli L, Palumbo R (1985) Effect of N-acetylcysteine in subjects with slow pulmonary mucociliary clearance. Eur J Respir Dis Suppl 139:136–141
Tossios P, Bloch W, Huebner A, Raji MR, Dodos F, Klass O, Suedkamp M, Kasper SM, Hellmich M, Mehlhorn U (2003) N-acetylcysteine prevents reactive oxygen species-mediated myocardial stress in patients undergoing cardiac surgery: results of a randomized, double-blind, placebo-controlled clinical trial. J Thorac Cardiovasc Surg 126(5):1513–1520
Travaline JM, Sudarshan S, Roy BG, Cordova F, Leyenson V, Criner GJ (1997) Effect of N-acetylcysteine on human diaphragm strength and fatigability. Am J Respir Crit Care Med 156(5):1567–1571
Treeprasertsuk S, Krudsood S, Tosukhowong T, Maek ANW, Vannaphan S, Saengnetswang T, Looareesuwan S, Kuhn WF, Brittenham G, Carroll J (2003) N-acetylcysteine in severe falciparum malaria in Thailand. Southeast Asian J Trop Med Public Health 34(1):37–42
Tripi S, Di Gaetano G, Soresi M, Carroccio A, Bonfissuto G, Savi A, Vuturo O, Montalto G (1998) Acetylcysteine therapy for chronic hepatitis C: are its effects synergistic with interferon alpha? A pilot study. Clin Drug Invest 16(4):297–302
Uden S, Bilton D, Guyan PM, Kay PM, Braganza JM (1990) Rationale for antioxidant therapy in pancreatitis and cystic fibrosis. Adv Exp Med Biol 264:555–572
Unverferth DV, Jagadeesh JM, Unverferth BJ, Magorien RD, Leier CV, Balcerzak SP (1983) Attempt to prevent doxorubicin-induced acute human myocardial morphologic damage with acetylcysteine. J Natl Cancer Inst 71(5):917–920
Upritchard JE, Sutherland WH, Mann JI (2000) Effect of supplementation with tomato juice, vitamin E, and vitamin C on LDL oxidation and products of inflammatory activity in type 2 diabetes. Diabetes Care 23(6):733–738
Usal A, Acarturk E, Yuregir GT, Unlukurt I, Demirci C, Kurt HI, Birand A (1996) Decreased glutathione levels in acute myocardial infarction. Jpn Heart J 37(2):177–182
van Bakel MM, Printzen G, Wermuth B, Wiesmann UN (2000) Antioxidant and thyroid hormone status in selenium-deficient phenylketonuric and hyperphenylalaninemic patients. Am J Clin Nutr 72(4):976–981
van Dalen EC, Caron HN, Dickinson HO, Kremer LC (2005) Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev 1:CD003917
Van Schooten FJ, Nia AB, De Flora S, D’Agostini F, Izzotti A, Camoirano A, Balm AJ, Dallinga JW, Bast A, Haenen GR, Van’t Veer L, Baas P, Sakai H, Van Zandwijk N (2002) Effects of oral administration of N-acetyl-L-cysteine: a multi-biomarker study in smokers. Cancer Epidemiol Biomark Prev 11(2):167–175
Vecchiarelli A, Dottorini M, Pietrella D, Cociani C, Eslami A, Todisco T, Bistoni F (1994) Macrophage activation by N-acetyl-cysteine in COPD patients. Chest 105(3):806–811
Verhagen H, Hageman GJ, Rauma AL, Versluis-de Haan G, van Herwijnen MH, de Groot J, Torronen R, Mykkanen H (2001) Biomonitoring the intake of garlic via urinary excretion of allyl mercapturic acid. Br J Nutr 86(Suppl 1):S111–S114
Verhulst M-L, Van Oijen AHAM, Roelofs HMJ, Peters WHM, Jansen JBMJ (2000) Antral glutathione concentration and glutathione S-transferase activity in patients with and without Helicobacter pylori. Dig Dis Sci 45(3):629–632
Verjee ZH, Behal R (1976) Protein-calorie malnutrition: a study of red blood cell and serum enzymes during and after crisis. Clin Chim Acta 70(1):139–147
Verstraeten JM (1979) Mucolytic treatment in chronic obstructive pulmonary disease. Double-blind comparative clinical trial with N-acetylcysteine, bromhexine and placebo. Acta Tuberc Pneumol Belg 70(1):71–80
Villa P, Saccani A, Sica A, Ghezzi P (2002) Glutathione protects mice from lethal sepsis by limiting inflammation and potentiating host defense. J Infect Dis 185(8):1115–1120
Vita JA, Frei B, Holbrook M, Gokce N, Leaf C, Keaney Jr JF (1998) L-2-oxothiazolidine-4-carboxylic acid reverses endothelial dysfunction in patients with coronary artery disease. J Clin Invest 101(6):1408–1414
Vlamis-Gardikas A, Holmgren A (2002) Thioredoxin and glutaredoxin isoforms. Methods Enzymol 347:286–296
Volkin DB, Klibanov AM (1987) Thermal destruction processes in proteins involving cystine residues. J Biol Chem 262(7):2945–2950
Wagdi P, Fluri M, Aeschbacher B, Fikrle A, Meier B (1996) Cardioprotection in patients undergoing chemo- and/or radiotherapy for neoplastic disease. A pilot study. Jpn Heart J 37(3):353–359
Wagdi P, Rouvinez G, Fluri M, Aeschbacher B, Thoni A, Schefer H, Meier B (1995) Cardioprotection in chemo- and radiotherapy for malignant diseases – an echocardiographic pilot study. Schweiz Rundsch Med Prax 84(43):1220–1223
Walmsley SL, Winn LM, Harrison ML, Uetrecht JP, Wells PG (1997) Oxidative stress and thiol depletion in plasma and peripheral blood lymphocytes from HIV-infected patients: toxicological and pathological implications. AIDS 11(14):1689–1697
Walters MT, Rubin CE, Keightley SJ, Ward CD, Cawley MI (1986) A double-blind, cross-over, study of oral N-acetylcysteine in Sjogren’s syndrome. Scand J Rheumatol Suppl 61:253–258
Wang J, Boja ES, Tan W, Tekle E, Fales HM, English S, Mieyal JJ, Chock PB (2001) Reversible Glutathionylation Regulates Actin Polymerization in A431 Cells. J Biol Chem 276(51):47763–47766
Ward KP, Arthur JR, Russell G, Aggett PJ (1984) Blood selenium content and glutathione peroxidase activity in children with cystic fibrosis, coeliac disease, asthma, and epilepsy. Eur J Pediatr 142(1):21–24
Watt G, Jongsakul K, Ruangvirayuth R (2002) A pilot study of N-acetylcysteine as adjunctive therapy for severe malaria. QJM 95(5):285–290
Weber S, Auclert L, Touiza K, Pellois A, Guerin C, Blin P, Guerin F (1992) Evaluation of tolerance during intravenous administration of low dose of isosorbide dinitrate in the treatment of unstable angina. Arch Mal Coeur Vaiss 85(1):59–65
Weigand MA, Plachky J, Thies JC, Spies-Martin D, Otto G, Martin E, Bardenheuer HJ (2001) N-acetylcysteine attenuates the increase in alpha-glutathione S-transferase and circulating ICAM-1 and VCAM-1 after reperfusion in humans undergoing liver transplantation. Transplantation 72(4):694–698
Weikert LF, Bernard GR (1996) Pharmacotherapy of sepsis. Clin Chest Med 17(2):289–305
White AC, Thannickal VJ, Fanburg BL (1994) Glutathione deficiency in human disease. J Nutr Biochem 5:218–226
Whitekus MJ, Li N, Zhang M, Wang M, Horwitz MA, Nelson SK, Horwitz LD, Brechun N, Diaz-Sanchez D, Nel AE (2002) Thiol antioxidants inhibit the adjuvant effects of aerosolized diesel exhaust particles in a murine model for ovalbumin sensitization. J Immunol 168(5):2560–2567
Wiklund O, Fager G, Andersson A, Lundstam U, Masson P, Hultberg B (1996) N-acetylcysteine treatment lowers plasma homocysteine but not serum lipoprotein(a) levels. Atherosclerosis 119(1):99–106
Winkler E, Halkin H (1992) Paracetamol overdose in Israel–1992. Isr J Med Sci 28(11):811–812
Winklhofer-Roob BM (2000) Cystic fibrosis: nutritional status and micronutrients [In Process Citation]. Curr Opin Clin Nutr Metab Care 3(4):293–297
Winterbourn CC, Peskin AV, Parsons-Mair HN (2002) Thiol oxidase activity of copper, zinc superoxide dismutase. J Biol Chem 277(3):1906–1911
Woo OF, Mueller PD, Olson KR, Anderson IB, Kim SY (2000) Shorter duration of oral N-acetylcysteine therapy for acute acetaminophen overdose. Ann Emerg Med 35(4):363–368
Xu D, Finkel T (2002) A role for mitochondria as potential regulators of cellular life span. Biochem Biophys Res Commun 294(2):245–248
Yalcin E, Altin F, Cinhuseyinoglue F, Arslan MO (2002) N-acetylcysteine in chronic blepharitis. Cornea 21(2):164–168
Yang ES, Richter C, Chun JS, Huh TL, Kang SS, Park JW (2002) Inactivation of NADP(+)-dependent isocitrate dehydrogenase by nitric oxide. Free Radic Biol Med 33(7):927–937
Yiengpruksawan A, Lightdale CJ, Gerdes H, Botet JF (1991) Mucolytic-antifoam solution for reduction of artifacts during endoscopic ultrasonography: a randomized controlled trial. Gastrointest Endosc 37(5):543–546
Yoshida K, Hirokawa J, Tagami S, Kawakami Y, Urata Y, Kondo T (1995) Weakened cellular scavenging activity against oxidative stress in diabetes mellitus: regulation of glutathione synthesis and efflux. Diabetologia 38(2):201–210
Yucel D, Aydogdu S, Cehreli S, Saydam G, Canatan H, Senes M, Topkaya BC, Nebioglu S (1998) Increased oxidative stress in dilated cardiomyopathic heart failure. Clin Chem 44(1):148–154
Zhong L, Arner ES, Holmgren A (2000a) Structure and mechanism of mammalian thioredoxin reductase: the active site is a redox-active selenolthiol/selenenylsulfide formed from the conserved cysteine-selenocysteine sequence. Proc Natl Acad Sci U S A 97(11):5854–5859
Zhong L, Holmgren A (2000) Essential role of selenium in the catalytic activities of mammalian thioredoxin reductase revealed by characterization of recombinant enzymes with selenocysteine mutations. J Biol Chem 275(24):18121–18128
Zhong L, Persson K, Sandalova T, Schneider G, Holmgren A (2000b) Purification, crystallization and preliminary crystallographic data for rat cytosolic selenocysteine 498 to cysteine mutant thioredoxin reductase. Acta Crystallogr D Biol Crystallogr 56(Pt 9):1191–1193
Zimmerman RJ, Marafino BJ Jr, Chan A, Landre P, Winkelhake JL (1989) The role of oxidant injury in tumor cell sensitivity to recombinant human tumor necrosis factor in vivo. Implications for mechanism of action. J Immunol 142:1405–1409
Acknowledgments
This presentation would not have been completed without the help from Mr. David Aiello (BioAdvantex Pharma, Mississauga, Ontario, Canada) and Dr. Thilo Messerschmidt (Diamalt B.F. Goodrich, Raubling, Germany). Mr. Aiello helped ferret out and interpret citations of importance for this manuscript and provided key editorial and technical support when we needed it most. Dr. Messerschmidt provided highly valuable technical and biochemical insights in addition to editorial advice concerning NAC synthesis and the mechanisms involved in maintaining the redox balance in cells and organisms. Mr. Onny Chattergee and Mr. Kevin McCaffrey provided unstinting technical help in the organization and handling of the many publications reviewed here, and Ms. Claudia Weber provided the solid administrative support that allowed us to focus on the mammoth job of collecting and reviewing all of these publications. Studies presented here were supported in part by a grant (CA-42509) from the National Cancer Institute of the US National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
Online Table 20.1
Studies excluded from this review (DOCX 31 kb)
Online Table 20.2
NAC treatment in randomized placebo-controlled studies (DOCX 60 kb)
Online Table 20.3
Intravenous (IV) NAC (DOCX 44 kb)
Online Table 20.4
Observational NAC treatment studies (DOCX 40 kb)
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Ghezzi, P. et al. (2019). Cysteine/Glutathione Deficiency: A Significant and Treatable Corollary of Disease. In: Frye, R., Berk, M. (eds) The Therapeutic Use of N-Acetylcysteine (NAC) in Medicine. Adis, Singapore. https://doi.org/10.1007/978-981-10-5311-5_20
Download citation
DOI: https://doi.org/10.1007/978-981-10-5311-5_20
Published:
Publisher Name: Adis, Singapore
Print ISBN: 978-981-10-5310-8
Online ISBN: 978-981-10-5311-5
eBook Packages: MedicineMedicine (R0)