Abstract
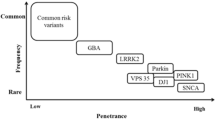
The contribution of genes to etiology is variable for different movement disorders. Some diseases are by definition genetic, such as Huntington’s disease (HD) – in all cases caused by expanded repeats in the Huntingtin (HTT) gene. Other disorders such as Parkinson’s disease may have monogenic causes but are largely the result of nongenetic factors. Dystonia and the atypical parkinsonisms have high genetic burdens in their etiologies, with reduced penetrance being a common feature. Essential tremor (ET) and restless legs syndrome (RLS) may be familial, although no monogenic causes have been elucidated; rather, risk-conferring alleles contribute to etiology. In this chapter, we review the genetic causes of these movement disorders. We focus on the monogenic causes of autosomal dominant (SNCA, LRRK2, VPS35) and recessive (PARKIN, PINK1, DJ-1) Parkinson’s disease, of isolated (TOR1A, THAP1, GNAL) and combined (GCH1, TH, ATP1A3, PRKRA, TAF1, SGCE) dystonia, and of the paroxysmal movement disorders (PRRT2, MR1, SLC2A1). We also briefly cover Huntingtin and the genes that have been linked to atypical parkinsonism, essential tremor, and restless legs syndrome. Importantly, we include new reports of genes that have been identified via next-generation sequencing, with the caveat that a number still require independent validation in more genetic and functional studies. Because the genetics of movement disorders are complex, genetic testing results determining the clinical diagnosis can only be recommended for genes that are unequivocally disease causing. However, gene panel testing is slowly transitioning into clinical utility, heralding the transition of movement disorder genetics from bench to bedside.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Williams DR, Litvan I. Parkinsonian syndromes. Continuum. 2013;19(5, Movement Disorders):1189–212.
Alcalay RN, Caccappolo E, Mejia-Santanaet H, et al. Frequency of known mutations in early-onset Parkinson disease: implication for genetic counseling. Arch Neurol. 2010;67(9):1116–22.
Marras C, Lang A, Lohmann K, et al. Fixing the broken system of genetic locus symbols: Parkinson disease and dystonia as examples. Neurology. 2012;78(13):1016–24.
Norris EH, Giasson BI, Lee VMY. α-Synuclein: normal function and role in neurodegenerative diseases. In: Schatten GP, editor. Current topics in developmental biology, vol 60, Stem cells in development and disease. Academic; 2004. p. 17–54. doi:10.1016/S0070-2153(04)60002-0.
Spillantini MG, Schmidt ML, Lee VM. [alpha]-Synuclein in Lewy bodies. Nature. 1997;388(6645):839–40.
Klein C, Schlossmacher MG. Parkinson disease, 10 years after its genetic revolution: multiple clues to a complex disorder. Neurology. 2007;69(22):2093–104.
Polymeropoulos MH, Lavedan C, Leroy E, et al. Mutation in the α-synuclein gene identified in families with Parkinson’s disease. Science. 1997;276(5321):2045–7.
Kasten M, Klein C. The many faces of alpha-synuclein mutations. Mov Disord. 2013;28(6):697–701.
Nuytemans K, Theuns S, Cruts M, et al. Genetic etiology of Parkinson disease associated with mutations in the SNCA, PARK2, PINK1, PARK7, and LRRK2 genes: a mutation update. Hum Mutat. 2010;31(7):763–80.
Singleton AB, Farrer M, Johnson J, et al. α-Synuclein locus triplication causes Parkinson’s disease. Science. 2003;302(5646):841.
Healy DG, Falchi M, O’Sullivan SS, et al. Phenotype, genotype, and worldwide genetic penetrance of LRRK2-associated Parkinson’s disease: a case-control study. Lancet Neurol. 2008;7(7):583–90.
Saunders-Pullman R, Stanley K, Wang C, et al. Olfactory dysfunction in LRRK2 G2019S mutation carriers. Neurology. 2011;77(4):319–24.
Zimprich A, Biskup S, Leitner P, et al. Mutations in LRRK2 cause autosomal-dominant parkinsonism with pleomorphic pathology. Neuron. 2004;44(4):601–7.
Kachergus J, Mata IF, Hulihan M, et al. Identification of a novel LRRK2 mutation linked to autosomal dominant parkinsonism: evidence of a common founder across European populations. Am J Hum Genet. 2005;76(4):672–80.
Ozelius L, Senthil J, Saunders-Pullman R, et al. LRRK2 G2019S as a cause of Parkinson’s disease in Ashkenazi jews. N Engl J Med. 2006;354(4):424–5.
Tan EK, Shena H, Tan LCS, et al. The G2019S LRRK2 mutation is uncommon in an Asian cohort of Parkinson’s disease patients. Neurosci Lett. 2005;384(3):327–9.
Klein C, Westenberger A. Genetics of Parkinson’s disease. Cold Spring Harb Perspect Med. 2012;2(1):a008888.
Hentati F, Trinh J, Thomson C, et al. Lrrk2 parkinsonism in Tunisia and Norway: a comparative analysis of disease penetrance. Neurology. 2014;83:568–9.
Funayama M, Li Y, Tomiyama H, et al. Leucine-rich repeat kinase 2 G2385R variant is a risk factor for Parkinson disease in Asian population. Neuroreport. 2007;18(3):273–5.
Vilariño-Güell C, Wider C, Ross OA, et al. VPS35 mutations in Parkinson disease. Am J Hum Genet. 2011;89(1):162–7.
Zimprich A, Benet-Pagès A, Struhal W. A mutation in VPS35, encoding a subunit of the retromer complex, causes late-onset Parkinson disease. Am J Hum Genet. 2011;89(1):168–75.
Sharma M, Ioannidis JPA, Aasly JO, et al. A multi-centre clinico-genetic analysis of the VPS35 gene in Parkinson disease indicates reduced penetrance for disease-associated variants. J Med Genet. 2012;49(11):721–6.
Bonifati V. Genetics of Parkinson’s disease – state of the art, 2013. Parkinsonism Relat Disord. 2014;20 Suppl 1:S23–8.
Priya A, Kalaidzidis IV, Kalaidzidis Y, Lambright D, Datta S. Molecular insights into rab7-mediated endosomal recruitment of core retromer: deciphering the role of vps26 and vps35. Traffic. 2015;16(1):68–84.
Vilariño-Güell C, Rajput A, Milnerwood AJ. DNAJC13 mutations in Parkinson disease. Hum Mol Genet. 2014;23(7):1794–801.
Funayama M, Ohe K, Amo T, et al. CHCHD2 mutations in autosomal dominant late-onset Parkinson’s disease: a genome-wide linkage and sequencing study. Lancet Neurol. 2015;14:274–82.
Lohmann E, Periquet M, Bonifati V, et al. How much phenotypic variation can be attributed to parkin genotype? Ann Neurol. 2003;54(2):176–85.
Grünewald A, Kasten M, Ziegler A, et al. Next-generation phenotyping using the Parkin example: time to catch up with genetics. JAMA Neurol. 2013;70(9):1186–91.
Doherty KM, Silveira-Moriyama L, Parkkinen L, et al. Parkin disease: a clinicopathologic entity? JAMA Neurol. 2013;70(5):571–9.
Zanon A, Rakovic A, Blankenburg H, et al. Profiling of Parkin-binding partners using tandem affinity purification. PLoS One. 2013;8(11):e78648.
Hasson SA, Kane LA, Yamano K, et al. High-content genome-wide RNAi screens identify regulators of parkin upstream of mitophagy. Nature. 2013;504(7479):291–5.
Valente EM, Abou-Sleiman PM, Caputo V, et al. Hereditary early-onset Parkinson’s disease caused by mutations in PINK1. Science. 2004;304(5674):1158–60.
Gelmetti V, Ferraris A, Brusa L, et al. Late onset sporadic Parkinson’s disease caused by PINK1 mutations: clinical and functional study. Mov Disord. 2008;23(6):881–5.
Klein C, Schlossmacher MG. The genetics of Parkinson disease: implications for neurological care. Nat Clin Prac Neurol. 2006;2(3):136–46.
Kasten M, Weichert C, Lohmann K, Klein C. Clinical and demographic characteristics of PINK1 mutation carriers – a meta-analysis. Mov Disord. 2010;25(7):952–4.
Youle RJ, Narendra DP. Mechanisms of mitophagy. Nat Rev Mol Cell Biol. 2011;12(1):9–14.
Rakovic A, Grünewald A, Kottwitz J, et al. Mutations in PINK1 and Parkin impair ubiquitination of mitofusins in human fibroblasts. PLoS One. 2011;6(3):e16746.
Grünewald A, Voges L, Rakovic A, et al. Mutant Parkin impairs mitochondrial function and morphology in human fibroblasts. PLoS One. 2010;5(9):e12962.
Bonifati V, Rizzu P, van Baren MJ, et al. Mutations in the DJ-1 gene associated with autosomal recessive early-onset parkinsonism. Science. 2003;299(5604):256–9.
Canet-Avilés RM, Wilson M, Miller D, et al. The Parkinson’s disease protein DJ-1 is neuroprotective due to cysteine-sulfinic acid-driven mitochondrial localization. Proc Natl Acad Sci U S A. 2004;101(24):9103–8.
Lill CM, Roehr JT, McQueen MB, et al. Comprehensive research synopsis and systematic meta-analyses in Parkinson’s disease genetics: the PDGene database. PLoS Genet. 2012;8(3):e1002548.
Lesage S, Anheim M, Condroyer C, et al. Large-scale screening of the Gaucher’s disease-related glucocerebrosidase gene in Europeans with Parkinson’s disease. Human Mol Genet. 2011;20(1):202–10.
Sidransky E, Nalls MA, Aasly JO, et al. Multicenter analysis of glucocerebrosidase mutations in Parkinson’s disease. N Engl J Med. 2009;361(17):1651–61.
Alcalay RN, Dinur T, Quinn T, et al. Comparison of parkinson risk in Ashkenazi jewish patients with Gaucher disease and GBA heterozygotes. JAMA Neurol. 2014;71(6):752–7.
Stamelou M, Quinn NP, Bhatia K. “Atypical” atypical parkinsonism: new genetic conditions presenting with features of progressive supranuclear palsy, corticobasal degeneration, or multiple system atrophy – diagnostic guide. Mov Disord. 2013;28(9):1184–99.
Oppenheim H. Űber eine eigenartige Krampfkrankheit des kindlichen und jugendlichen Alters (Dysbasia lordotica progressiva, Dystonia musculorum deformans). Neurol Cent. 1911;30:1090–107.
Klein C, Fahn S. Translation of Oppenheim’s 1911 paper on dystonia. Mov Disord. 2013;28:851–62.
Albanese A, Bhatia K, Bressman SB, et al. Phenomenology and classification of dystonia: a consensus update. Mov Disord. 2013;28:863–73.
Klein C. Genetics in dystonia. Park Relat Disord. 2014;20(Suppl1):S137–42.
Klein C, Marras C, Münchau A. Dystonia overview. In: Pagon RA, Adam MP, Ardinger HH, et al., editors. GeneReviews. Seattle: University of Washington; 2014.
Bressman SB, Sabatti C, Raymond D, et al. The DYT1 phenotype and guidelines for diagnostic testing. Neurology. 2000;54:1746–52.
Ozelius LJ, Hewett JW, Page CE, et al. The early-onset torsion dystonia gene (DYT1) encodes an ATP-binding protein. Nat Genet. 1997;17:40–8.
Fuchs T, Gavarini S, Saunders-Pullman R, et al. Mutations in the THAP1 gene are responsible for DYT6 primary torsion dystonia. Nat Genet. 2009;41:286–8.
Blanchard A, Ea V, Roubertie A, et al. DYT6 dystonia: review of the literature and creation of the UMD Locus-Specific Database (LSDB) for mutations in the THAP1 gene. Hum Mutat. 2011;32:1213–24.
Vemula SR, Puschmann A, Xiao J. Role of Galpha(olf) in familial and sporadic adult-onset primary dystonia. Hum Mol Genet. 2013;22:2510–9.
Kumar KR, Lohmann K, Masuho I, et al. Phenotypic spectrum of mutations in GNAL: a novel cause of cranio-cervical dystonia. JAMA Neurol. 2013;71(4):490–4.
Xiao J, Uitti RJ, Zhao Y, et al. Mutations in CIZ1 cause adult onset primary cervical dystonia. Ann Neurol. 2012;71:458–69.
Charlesworth G, Plagnol V, Holmstrom KM, et al. Mutations in Ano3 cause dominant craniocervical dystonia: ion channel implicated in pathogenesis. Am J Hum Genet. 2012;91:1041–50.
Charlesworth G, Angelova PR, Bartolomé-Robledo F, et al. Mutations in HPCA cause autosomal-recessive primary isolated dystonia. Am J Hum Genet. 2015;96(4):657–65.
Zech M, Lam DD, Francescatto L. Recessive mutations in the α3 (VI) collagen gene COL6A3 cause early-onset isolated dystonia. Am J Hum Genet. 2015;96(6):883–93.
Lohmann K, Wilcox R, Winkler S, et al. Whispering dysphonia (DYT4 dystonia) is caused by a mutation in the TUBB4 gene. Ann Neurol. 2013;73(4):537–45.
Hersheson J, Mencacci NE, Davis M, et al. Mutations in the autoregulatory domain of ß-tubulin 4a cause hereditary dystonia. Ann Neurol. 2013;73(4):546–53.
Simons C, Wolf NI, McNeil N. A de novo mutation in the β-tubulin gene TUBB4A results in the leukoencephalopathy hypomyelination with atrophy of the basal ganglia and cerebellum. Am J Hum Genet. 2013;92(5):767–73.
Segawa M, Hosaka A, Miyagawa F, et al. Hereditary progressive dystonia with marked diurnal fluctuation. Adv Neurol. 1976;14:215–33.
Mencacci NE, Isaias IU, Reich MM, et al. Parkinson’s disease in GTP cyclohydrolase 1 mutation carriers. Brain. 2014;137(Pt 9):2480–92.
Tadic V, Kasten M, Bruggemann N, et al. Dopa-responsive dystonia revisited: diagnostic delay, residual signs, and nonmotor signs. Arch Neurol. 2012;69(12):1558–62.
de Carvalho Aguiar P, Sweadner KJ, Penniston JT, et al. Mutations in the Na+/K+ -ATPase alpha3 gene ATP1A3 are associated with rapid-onset dystonia parkinsonism. Neuron. 2004;43:169–75.
Heinzen EL, Swoboda KJ, Hitomi Y, et al. De novo mutations in ATP1A3 cause alternating hemiplegia of childhood. Nat Genet. 2012;44:1030–4.
Demos MK, van Karnebeek CD, Ross CJ. A novel recurrent mutation in ATP1A3 causes CAPOS syndrome. Orphanet J Rare Dis. 2014;9:15.
Camargos S, Scholz S, Simón-Sánchez J, et al. DYT16, a novel young-onset dystonia-parkinsonism disorder: identification of a segregating mutation in the stress-response protein PRKRA. Lancet Neurol. 2008;7(3):207–15.
Zech M, Castrop F, Schormair B. DYT16 revisited: exome sequencing identifies PRKRA mutations in a European dystonia family. Mov Disord. 2014;29(12):1504–10.
Seibler P, Djarmati A, Langpap B, et al. A heterozygous frameshift mutation in PRKRA (DYT16) associated with generalised dystonia in a German patient. Lancet Neurol. 2008;7(5):380–1.
Lee LV, Rivera C, Teleg RA, et al. The unique phenomenology of sex-linked dystonia parkinsonism (XDP, DYT3, “Lubag”). Int J Neurosci. 2011;121 Suppl 1:3–11.
Domingo A, Westenberger A, Lee LV, et al. New insights on the genetics of X-linked dystonia-parkinsonism (XDP/DYT3). Eur J Hum Genet. 2015;23(10):1334–40.
Makino S, Kaji R, Ando S, et al. Reduced neuron-specific expression of the TAF1 gene is associated with X-linked dystonia-parkinsonism. Am J Hum Genet. 2007;80:393–406.
Domingo A, Amar D, Grütz K, et al. Evidence of TAF1 dysfunction in peripheral models of X-linked dystonia-parkinsonism. Cell Mol Life Sci. 2016. [Epub ahead of print].
Zimprich A, Grabowski M, Asmus F, et al. Mutations in the gene encoding epsilon-sarcoglycan cause myoclonus-dystonia syndrome. Nat Genet. 2001;29:66–9.
Müller B, Hedrich K, Kock N, et al. Evidence that paternal expression of the epsilon-sarcoglycan gene accounts for reduced penetrance in myoclonus-dystonia. Am J Hum Genet. 2002;71:1303–11.
Groen JL, Andrade A, Ritz K, et al. CACNA1B mutation is linked to unique myoclonus-dystonia syndrome. Hum Mol Genet. 2015;24(4):987–93.
Mencacci NE, Rubio-Agusti I, Zdebik A, et al. A missense mutation in KCTD17 causes autosomal dominant myoclonus-dystonia. Am J Hum Genet. 2015;96(6):938–47.
Risch NJ, Bressman SB, Senthil G, Ozelius LJ. Intragenic cis and trans modification of genetic susceptibility in DYT1 torsion dystonia. Am J Hum Genet. 2007;80(6):1188–93.
Kamm C, Fischer H, Garavaglia B, et al. Susceptibility to DYT1 dystonia in European patients is modified by the D216H polymorphism. Neurology. 2008;70(23):2261–2.
Mok KY, Schneider SA, Trabzuni D, et al. Genomewide association study in cervical dystonia demonstrates possible association with sodium leak channel. Mov Disord. 2014;29(2):245–51.
Lohmann K, Schmidt A, Schillert A, et al. Genome-wide association study in musician’s dystonia: a risk variant at the arylsulfatase G locus? Mov Disord. 2014;29(7):921–7.
Gómez-Garre P, Huertas-Fernández I, Cáceres-Redondo MT, et al. Lack of validation of variants associated with cervical dystonia risk: a GWAS replication study. Mov Disord. 2014;29(14):1825–8.
Schmidt A, Kumar KR, Redyk K, et al. Two faces of the same coin: benign familial infantile seizures and paroxysmal kinesigenic dyskinesia caused by PRRT2 mutations. Arch Neurol. 2013;69(5):668–70.
Chen WJ, Lin Y, Xiong ZQ, et al. Exome sequencing identifies truncating mutations in PRRT2 that cause paroxysmal kinesigenic dyskinesia. Nat Genet. 2011;43:1252–5.
Lee HY, Xu Y, Huang Y, et al. The gene for paroxysmal non-kinesigenic dyskinesia encodes an enzyme in a stress response pathway. Hum Mol Genet. 2004;13:3161–70.
Weber YG, Storch A, Wuttke TV, et al. GLUT1 mutations are a cause of paroxysmal exertion-induced dyskinesias and induce hemolytic anemia by a cation leak. J Clin Invest. 2008;118:2157–68.
Weber YG, Kamm C, Suls A, et al. Paroxysmal choreoathetosis/spasticity (DYT9) is caused by a GLUT1 defect. Neurology. 2011;77:959–64.
MacDonald, Bates, Buckler, et al. A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington’s disease chromosomes. Cell. 1993;72(6):971–83.
Warby S, Graham RK, Hayden MR. Huntington’s disease. In: Pagon RA, Adam MP, Ardinger HH, et al., editors. GeneReviews. Seattle: University of Washington; 2014.
Semaka A, Creighton S, Warby S, Hayden MR. Predictive testing for Huntington disease: interpretation and significance of intermediate alleles. Clin Genet. 2006;70(4):283–94.
Killoran A, Biglan KM, Jankovic J, et al. Characterization of the Huntington intermediate CAG repeat expansion phenotype in PHAROS. Neurology. 2013;80:2022.
Ha AD, Fung V. Huntington’s disease. Curr Opin Neurol. 2012;25(4):491–8.
Ross CA, Tabrizi SJ. Huntington’s disease: from molecular pathogenesis to clinical treatment. Lancet Neurol. 2011;10:83–98.
Zeuner K, Deuschl G. An update on tremors. Curr Opin Neurol. 2012;25(4):475–82.
Gulcher JR, Jónsson P, Kong A, et al. Mapping of a familial essential tremor gene, FET1, to chromosome 3q13. Nat Genet. 1997;17(1):84–7. PubMed PMID: 9288103.
Jeanneteau F, Funalot B, Jankovic J, et al. A functional variant of the dopamine D3 receptor is associated with risk and age-at-onset of essential tremor. Proc Natl Acad Sci U S A. 2006;103(28):10753–8.
Kuhlenbäumer G, Hopfner F, Deuschl G. Genetics of essential tremor: meta-analysis and review. Neurology. 2014;82(11):1000–7.
Higgins JJ, Lombardi RQ, Pucilowska J, Jankovic J, Tan EK, Rooney JP. A variant in the HS1-BP3 gene is associated with familial essential tremor. Neurology. 2005;64(3):417–21.
Merner ND, Girard SL, Catoire H, et al. Exome sequencing identifies FUS mutations as a cause of essential tremor. Am J Hum Genet. 2012;91(2):313–9.
Hopfner F, Stevanin G, Müller SH, et al. The impact of rare variants in FUS in essential tremor. Mov Disord. 2015;30(5):721–4.
Gulsuner H, Gulsuner S, Mercan FN, et al. Mitochondrial serine protease HTRA2 p.G399S in a kindred with essential tremor and Parkinson disease. Proc Natl Acad Sci U S A. 2014. pii: 201419581. [Epub ahead of print].
Strauss KM, Martins LM, Plun-Favreau H, et al. Loss of function mutations in the gene encoding Omi/HtrA2 in Parkinson’s disease. Hum Mol Genet. 2005;14(15):2099–111.
Krüger R, Sharma M, Reiss O, et al. A large-scale genetic association study to evaluate the contribution of Omi/HtrA2 (PARK13) to Parkinson’s disease. Neurobiol Aging. 2011;32(3):548.e9–548.e18.
Stefansson H, Steinberg S, Petursson H, et al. Variant in the sequence of the LINGO1 gene confers risk of essential tremor. Nat Genet. 2009;41:277–9.
Thier S, Lorenz D, Nothnagel M, et al. Polymorphisms in the glial glutamate transporter SLC1A2 are associated with essential tremor. Neurology. 2012;79(3):243–8.
Trenkwalder C, Paulus W. Restless legs syndrome: pathophysiology, clinical presentation and management. Nat Rev Neurol. 2010;6(6):337–46.
Kumar KR, Lohmann K, Klein C. Genetics of Parkinson disease and other movement disorders. Curr Opin Neurol. 2012;25(4):466–74.
Winkelmann J, Schormair B, Lichtner P, et al. Genome-wide association study of restless legs syndrome identifies common variants in three genomic regions. Nat Genet. 2007;39(8):1000–6.
Schulte E, Kousi M, Tan PL, et al. Targeted resequencing and systematic in vivo functional testing identifies rare variants in MEIS1 as significant contributors to restless legs syndrome. Am J Hum Genet. 2014;95:85–95.
Domingo A, Erro R, Lohmann K. Novel Dystonia Genes: Clues on disease mechanisms and the complexities of high-throughput sequencing. Mov Disord. 2016;31(4):471–7.
Harbo HF, Finsterer J, Baets J, et al. EFNS guidelines on the molecular diagnosis of neurogenetic disorders: general issues, Huntington’s disease, Parkinson’s disease and dystonias. Eur J Neurol. 2009;16(7):777–85.
Lohmann K, Klein C. Next generation sequencing and the future of genetic diagnosis. Neurotherapeutics. 2014;11(4):699–707.
Acknowledgments
CK is supported by a career development award from the Hermann and Lilly Schilling Foundation, and AD is the recipient of a scholarship from the German Academic Exchange Service (DAAD).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer-Verlag Wien
About this chapter
Cite this chapter
Domingo, A., Klein, C. (2017). Genetics of Movement Disorders. In: Falup-Pecurariu, C., Ferreira, J., Martinez-Martin, P., Chaudhuri, K. (eds) Movement Disorders Curricula. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1628-9_9
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1628-9_9
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1627-2
Online ISBN: 978-3-7091-1628-9
eBook Packages: MedicineMedicine (R0)