Abstract
Transforming growth factor (TGF)-β signalling pathway recently received attention as putative therapeutic target in cancer therapy. TGF-β is dual functional in development of cancer. In early stages of tumour development, TGF-β plays tumour suppressive, and as tumour progressed, TGF-β is an oncogenic factor. Functioning as tumour suppressor, TGF-β is a potential growth inhibitor. Cancerous cells show high sensitivity to TGF-β inhibition either by depletion of TGF-β signalling components in genetic level or by perturbation of downstream signalling proteins in protein level. Intense investigations had revealed that Smad proteins constitute as core components of TGF-β intracellular cascades. Typical development of cancer often contains production of excess TGF-β which accelerates the invasion and metastasis as well as inhibiting the anti-tumoural immune responses. In order to design optimal approaches in cancer therapeutic regimes, comprehending the oncogenic function of TGF-β and function of its downstream proteins (Smads) are required. The approaches must be in the direction of inhibition of those TGF-β functions which induce metastasis phenotypes, but at the same time preserve its growth inhibitory effects. To date several anti-cancer drugs such as Genistein and several microRNAs such as microRNA-452, demonstrated the new insights in induction of tumour suppressive potential of TGF-β signalling pathways among various cancer types.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Roberts A, Sporn M. The transforming growth factor-βs. In: Peptide growth factors and their receptors I. New York, NY: Springer; 1990. p. 419–72.
Coffey R, et al. Selective inhibition of growth-related gene expression in murine keratinocytes by transforming growth factor beta. Mol Cell Biol. 1988;8(8):3088–93.
Welch DR, Fabra A, Nakajima M. Transforming growth factor beta stimulates mammary adenocarcinoma cell invasion and metastatic potential. Proc Natl Acad Sci. 1990;87(19):7678–82.
Akhurst RJ, Derynck R. TGF-β signaling in cancer a double-edged sword. Trends Cell Biol. 2001;11:S44–51.
Huminiecki L, et al. Emergence, development and diversification of the TGF-β signalling pathway within the animal kingdom. Evol Biol. 2009;9(1):28.
Kang Y, Chen C-R, Massagué J. A self-enabling TGFβ response coupled to stress signaling: smad engages stress response factor ATF3 for Id1 repression in epithelial cells. Mol Cell. 2003;11(4):915–26.
Padua D, et al. TGFβ primes breast tumors for lung metastasis seeding through angiopoietin-like 4. Cell. 2008;133(1):66–77.
Siegel PM, Massagué J. Cytostatic and apoptotic actions of TGF-β in homeostasis and cancer. Nat Rev Cancer. 2003;3(11):807–20.
Seoane J. The TGFß pathway as a therapeutic target in cancer. Clin Transl Oncol. 2008;10(1):14–9.
Annes JP, Munger JS, Rifkin DB. Making sense of latent TGFβ activation. J Cell Sci. 2003;116(2):217–24.
Ten Dijke P, Arthur HM. Extracellular control of TGFβ signalling in vascular development and disease. Nat Rev Mol Cell Biol. 2007;8(11):857–69.
Lee MK, et al. TGF‐β activates Erk MAP kinase signalling through direct phosphorylation of ShcA. EMBO J. 2007;26(17):3957–67.
Massagué J. TGFβ in cancer. Cell. 2008;134(2):215–30.
Shi Y, Massagué J. Mechanisms of TGF-β signaling from cell membrane to the nucleus. Cell. 2003;113(6):685–700.
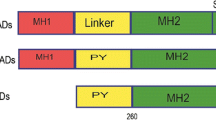
Massagué J, Seoane J, Wotton D. Smad transcription factors. Genes Dev. 2005;19(23):2783–810.
Inman GJ, Hill CS. Stoichiometry of active smad-transcription factor complexes on DNA. J Biol Chem. 2002;277(52):51008–16.
Massagué J. TGFβ signalling in context. Nat Rev Mol Cell Biol. 2012;13(10):616–30.
Huse M, et al. The TGFβ receptor activation process: an inhibitor-to substrate-binding switch. Mol Cell. 2001;8(3):671–82.
Groppe J, et al. Cooperative assembly of TGF-β superfamily signaling complexes is mediated by two disparate mechanisms and distinct modes of receptor binding. Mol Cell. 2008;29(2):157–68.
Batut J, et al. Two highly related regulatory subunits of PP2A exert opposite effects on TGF-β/Activin/Nodal signalling. Development. 2008;135(17):2927–37.
Kang JS, et al. The type I TGF-β receptor is covalently modified and regulated by sumoylation. Nat Cell Biol. 2008;10(6):654–64.
Moustakas A, Heldin C-H. The regulation of TGFβ signal transduction. Development. 2009;136(22):3699–714.
Shi W, et al. Endofin acts as a Smad anchor for receptor activation in BMP signaling. J Cell Sci. 2007;120(7):1216–24.
Chen Y-G, et al. Endofin, a FYVE domain protein, interacts with Smad4 and facilitates transforming growth factor-β signaling. J Biol Chem. 2007;282(13):9688–95.
Lin H-K, Bergmann S, Pandolfi PP. Cytoplasmic PML function in TGF-β signalling. Nature. 2004;431(7005):205–11.
Choi S-C, et al. Regulation of activin/nodal signaling by Rap2-directed receptor trafficking. Dev Cell. 2008;15(1):49–61.
Hu H, et al. Integration of transforming growth factor β and RAS signaling silences a RAB5 guanine nucleotide exchange factor and enhances growth factor-directed cell migration. Mol Cell Biol. 2008;28(5):1573–83.
Dai F, et al. Erbin inhibits transforming growth factor β signaling through a novel Smad-interacting domain. Mol Cell Biol. 2007;27(17):6183–94.
Clarke DC, et al. Transforming growth factor β depletion is the primary determinant of Smad signaling kinetics. Mol Cell Biol. 2009;29(9):2443–55.
Affolter M, Basler K. The Decapentaplegic morphogen gradient: from pattern formation to growth regulation. Nat Rev Genet. 2007;8(9):663–74.
Cheifetz S, et al. The transforming growth factor-β system, a complex pattern of cross-reactive ligands and receptors. Cell. 1987;48(3):409–15.
Zakin L, De Robertis E. Extracellular regulation of BMP signaling. Curr Biol. 2010;20(3):R89–92.
Zilberberg L, et al. Specificity of latent TGF‐β binding protein (LTBP) incorporation into matrix: role of fibrillins and fibronectin. J Cell Physiol. 2012;227(12):3828–36.
Groppe J, et al. Structural basis of BMP signalling inhibition by the cystine knot protein Noggin. Nature. 2002;420(6916):636–42.
Shi M, et al. Latent TGF-[bgr] structure and activation. Nature. 2011;474(7351):343–9.
Lindsay ME, Dietz HC. Lessons on the pathogenesis of aneurysm from heritable conditions. Nature. 2011;473(7347):308–16.
Müller P, et al. Differential diffusivity of Nodal and Lefty underlies a reaction-diffusion patterning system. Science. 2012;336(6082):721–4.
Wiater E, et al. Identification of distinct inhibin and transforming growth factor β-binding sites on betaglycan functional separation of betaglycan co-receptor actions. J Biol Chem. 2006;281(25):17011–22.
Schier AF. Nodal morphogens. Cold Spring Harb Perspect Biol. 2009;1(5):a003459.
Marchuk DA. Genetic abnormalities in hereditary hemorrhagic telangiectasia. Curr Opin Hematol. 1998;5(5):332–8.
Sekelsky JJ, et al. Genetic characterization and cloning of mothers against dpp, a gene required for decapentaplegic function in Drosophila melanogaster. Genetics. 1995;139(3):1347–58.
Derynck R, et al. Nomenclature: vertebrate mediators of TGFβ family signals. Cell. 1996;87(2):173.
Derynck R, Zhang YE. Smad-dependent and Smad-independent pathways in TGF-β family signalling. Nature. 2003;425(6958):577–84.
Zhang YE. Non-Smad pathways in TGF-β signaling. Cell Res. 2009;19(1):128–39.
Edlund S, et al. Transforming growth factor-β–induced mobilization of actin cytoskeleton requires signaling by small GTPases Cdc42 and RhoA. Mol Biol Cell. 2002;13(3):902–14.
Wu G, et al. Structural basis of Smad2 recognition by the Smad anchor for receptor activation. Science. 2000;287(5450):92–7.
Di Guglielmo GM, et al. Distinct endocytic pathways regulate TGF-β receptor signalling and turnover. Nat Cell Biol. 2003;5(5):410–21.
Le Roy C, Wrana JL. Clathrin-and non-clathrin-mediated endocytic regulation of cell signalling. Nat Rev Mol Cell Biol. 2005;6(2):112–26.
Itoh S, ten Dijke P. Negative regulation of TGF-β receptor/Smad signal transduction. Curr Opin Cell Biol. 2007;19(2):176–84.
Glasgow E, Mishra L. Transforming growth factor-β signaling and ubiquitinators in cancer. Endocr Relat Cancer. 2008;15(1):59–72.
Murakami G, et al. Cooperative inhibition of bone morphogenetic protein signaling by Smurf1 and inhibitory Smads. Mol Biol Cell. 2003;14(7):2809–17.
Kavsak P, et al. Smad7 binds to Smurf2 to form an E3 ubiquitin ligase that targets the TGFβ receptor for degradation. Mol Cell. 2000;6(6):1365–75.
Itoh S, et al. Transforming growth factor β1 induces nuclear export of inhibitory Smad7. J Biol Chem. 1998;273(44):29195–201.
Tajima Y, et al. Chromosomal region maintenance 1 (CRM1)-dependent nuclear export of Smad ubiquitin regulatory factor 1 (Smurf1) is essential for negative regulation of transforming growth factor-β signaling by Smad7. J Biol Chem. 2003;278(12):10716–21.
Wiesner S, et al. Autoinhibition of the HECT-type ubiquitin ligase Smurf2 through its C2 domain. Cell. 2007;130(4):651–62.
Suzuki C, et al. Smurf1 regulates the inhibitory activity of Smad7 by targeting Smad7 to the plasma membrane. J Biol Chem. 2002;277(42):39919–25.
Ogunjimi AA, et al. Regulation of Smurf2 ubiquitin ligase activity by anchoring the E2 to the HECT domain. Mol Cell. 2005;19(3):297–308.
Wrighton KH, Lin X, Feng X-H. Critical regulation of TGFβ signaling by Hsp90. Proc Natl Acad Sci. 2008;105(27):9244–9.
Datta PK, Moses HL. STRAP and Smad7 synergize in the inhibition of transforming growth factor β signaling. Mol Cell Biol. 2000;20(9):3157–67.
Komuro A, et al. Negative regulation of transforming growth factor-β (TGF-β) signaling by WW domain-containing protein 1 (WWP1). Oncogene. 2004;23(41):6914–23.
Lallemand F, et al. AIP4 restricts transforming growth factor-β signaling through a ubiquitination-independent mechanism. J Biol Chem. 2005;280(30):27645–53.
Kowanetz M, et al. TGFβ induces SIK to negatively regulate type I receptor kinase signaling. J Cell Biol. 2008;182(4):655–62.
Su Y, et al. The evolutionally conserved activity of Dapper2 in antagonizing TGF-β signaling. Fed Am Soc Exp Biol J. 2007;21(3):682–90.
Zhu H, et al. A SMAD ubiquitin ligase targets the BMP pathway and affects embryonic pattern formation. Nature. 1999;400(6745):687–93.
Lin X, Liang M, Feng X-H. Smurf2 is a ubiquitin E3 ligase mediating proteasome-dependent degradation of Smad2 in transforming growth factor-β signaling. J Biol Chem. 2000;275(47):36818–22.
Inoue Y, et al. Contribution of the constitutive and inducible degradation of Smad3 by the ubiquitin-proteasome pathway to transforming growth factor-β signaling. J Interferon Cytokine Res. 2004;24(1):43–54.
Li L, et al. CHIP mediates degradation of Smad proteins and potentially regulates Smad-induced transcription. Mol Cell Biol. 2004;24(2):856–64.
Guo X, et al. Axin and GSK3-β control Smad3 protein stability and modulate TGF-β signaling. Genes Dev. 2008;22(1):106–20.
Ross S, Hill CS. How the Smads regulate transcription. Int J Biochem Cell Biol. 2008;40(3):383–408.
Fuentealba LC, et al. Integrating patterning signals: Wnt/GSK3 regulates the duration of the BMP/Smad1 signal. Cell. 2007;131(5):980–93.
Lo RS, Massagué J. Ubiquitin-dependent degradation of TGF-β-activated Smad2. Nat Cell Biol. 1999;1(8):472–8.
Bonni S, et al. TGF-β induces assembly of a Smad2–Smurf2 ubiquitin ligase complex that targets SnoN for degradation. Nat Cell Biol. 2001;3(6):587–95.
Bai Y, et al. Itch E3 ligase-mediated regulation of TGF-β signaling by modulating smad2 phosphorylation. Mol Cell. 2004;15(5):825–31.
Wohlfert EA, et al. Cutting edge: deficiency in the E3 ubiquitin ligase Cbl-b results in a multifunctional defect in T cell TGF-β sensitivity in vitro and in vivo. J Immunol. 2006;176(3):1316–20.
Fukuchi M, et al. Ligand-dependent degradation of Smad3 by a ubiquitin ligase complex of ROC1 and associated proteins. Mol Biol Cell. 2001;12(5):1431–43.
Mavrakis KJ, et al. Arkadia enhances Nodal/TGF-β signaling by coupling phospho-Smad2/3 activity and turnover. PLoS Biol. 2007;5(3):e67.
Imoto S, et al. Regulation of transforming growth factor-β signaling by protein inhibitor of activated STAT, PIASy through Smad3. J Biol Chem. 2003;278(36):34253–8.
Wan M, et al. Smad4 protein stability is regulated by ubiquitin ligase SCFβ-TrCP1. J Biol Chem. 2004;279(15):14484–7.
Wan M, et al. Jab1 antagonizes TGF‐β signaling by inducing Smad4 degradation. EMBO Rep. 2002;3(2):171–6.
Liang M, et al. Ubiquitination and proteolysis of cancer-derived Smad4 mutants by SCFSkp2. Mol Cell Biol. 2004;24(17):7524–37.
Morén A, et al. Differential ubiquitination defines the functional status of the tumor suppressor Smad4. J Biol Chem. 2003;278(35):33571–82.
Lee PS, et al. Sumoylation of Smad4, the common Smad mediator of transforming growth factor-β family signaling. J Biol Chem. 2003;278(30):27853–63.
Wang B, Suzuki H, Kato M. Roles of mono-ubiquitinated Smad4 in the formation of Smad transcriptional complexes. Biochem Biophys Res Commun. 2008;376(2):288–92.
Jianyin L, et al. Repression of Smad4 transcriptional activity by SUMO modification. Biochem J. 2004;379(1):23–9.
Ebisawa T, et al. Smurf1 interacts with transforming growth factor-β type I receptor through Smad7 and induces receptor degradation. J Biol Chem. 2001;276(16):12477–80.
Koinuma D, et al. Arkadia amplifies TGF‐β superfamily signalling through degradation of Smad7. EMBO J. 2003;22(24):6458–70.
Grönroos E, et al. Control of Smad7 stability by competition between acetylation and ubiquitination. Mol Cell. 2002;10(3):483–93.
Simonsson M, et al. The balance between acetylation and deacetylation controls Smad7 stability. J Biol Chem. 2005;280(23):21797–803.
Shen R, et al. Smad6 interacts with Runx2 and mediates Smad ubiquitin regulatory factor 1-induced Runx2 degradation. J Biol Chem. 2006;281(6):3569–76.
Bai S, Cao X. A nuclear antagonistic mechanism of inhibitory Smads in transforming growth factor-β signaling. J Biol Chem. 2002;277(6):4176–82.
Inamitsu M, et al. Methylation of Smad6 by protein arginine N‐methyltransferase 1. Fed Eur Biochem Soc Lett. 2006;580(28-29):6603–11.
Heldin C-H, Moustakas A. A new twist in Smad signaling. Dev Cell. 2006;10(6):685–6.
Lönn P, et al. PARP-1 attenuates Smad-mediated transcription. Mol Cell. 2010;40(4):521–32.
Eichhorn PJ, et al. USP15 stabilizes TGF-[beta] receptor I and promotes oncogenesis through the activation of TGF-[beta] signaling in glioblastoma. Nat Med. 2012;18(3):429–35.
Inui M, et al. USP15 is a deubiquitylating enzyme for receptor-activated SMADs. Nat Cell Biol. 2011;13(11):1368–75.
Stroschein SL, et al. Negative feedback regulation of TGF-β signaling by the SnoN oncoprotein. Science. 1999;286(5440):771–4.
Lu Z, et al. Transforming growth factor β activates Smad2 in the absence of receptor endocytosis. J Biol Chem. 2002;277(33):29363–8.
Zhang L, et al. Determining TGF-β receptor levels in the cell membrane. TGF-β Signal Method Protoc. 2016;1344:35–47.
Yamashita M, et al. Ubiquitin ligase Smurf1 controls osteoblast activity and bone homeostasis by targeting MEKK2 for degradation. Cell. 2005;121(1):101–13.
Seo SR, et al. The novel E3 ubiquitin ligase Tiul1 associates with TGIF to target Smad2 for degradation. EMBO J. 2004;23(19):3780–92.
Shi W, et al. GADD34–PP1c recruited by Smad7 dephosphorylates TGFβ type I receptor. J Cell Biol. 2004;164(2):291–300.
Valdimarsdottir G, et al. Smad7 and protein phosphatase 1α are critical determinants in the duration of TGF-β/ALK1 signaling in endothelial cells. Cell Biol. 2006;7(1):16.
Xie W, et al. Alterations of smad signaling in human breast carcinoma are associated with poor outcome. Cancer Res. 2002;62(2):497–505.
Akhurst RJ. TGF-β antagonists: why suppress a tumor suppressor? J Clin Invest. 2002;109(12):1533–6.
Glick AB, et al. Transforming growth factor β1 suppresses genomic instability independent of a G1 arrest, p53, and Rb. Cancer Res. 1996;56(16):3645–50.
Agarwal MK, et al. Macrophage inhibitory cytokine 1 mediates a p53-dependent protective arrest in S phase in response to starvation for DNA precursors. Proc Natl Acad Sci. 2006;103(44):16278–83.
Maxwell CA, et al. Targeted and nontargeted effects of ionizing radiation that impact genomic instability. Cancer Res. 2008;68(20):8304–11.
Tabatabai G, et al. Irradiation and hypoxia promote homing of haematopoietic progenitor cells towards gliomas by TGF-β-dependent HIF-1α-mediated induction of CXCL12. Brain. 2006;129(9):2426–35.
Kanamoto T, et al. Functional proteomics of transforming growth factor‐β1‐stimulated Mv1Lu epithelial cells: Rad51 as a target of TGFβ1‐dependent regulation of DNA repair. EMBO J. 2002;21(5):1219–30.
Ewan KB, et al. Transforming growth factor-β1 mediates cellular response to DNA damage in situ. Cancer Res. 2002;62(20):5627–31.
Kirshner J, et al. Inhibition of transforming growth factor-β1 signaling attenuates ataxia telangiectasia mutated activity in response to genotoxic stress. Cancer Res. 2006;66(22):10861–9.
Shiloh Y, Ziv Y. The ATM protein kinase: regulating the cellular response to genotoxic stress, and more. Nat Rev Mol Cell Biol. 2013;14(4):197–210.
Savitsky K, et al. A single ataxia telangiectasia gene with a product similar to Pl-3 kinase. Science. 1995;268(5218):1749.
Whalen MK, et al. Specific ATM-mediated phosphorylation dependent on radiation quality. Radiat Res. 2008;170(3):353–64.
Wiegman EM, et al. TGFβ-1 dependent fast stimulation of ATM and p53 phosphorylation following exposure to ionizing radiation does not involve TGFβ-receptor I signalling. Radiother Oncol. 2007;83(3):289–95.
Barcellos-Hoff MH, Cucinotta FA. New tricks for an old fox: impact of TGFb on the DNA damage response and genomic stability. Sci Signal. 2014;7:re5.
Levy L, Hill CS. Smad4 dependency defines two classes of transforming growth factor β (TGF-β) target genes and distinguishes TGF-β-induced epithelial-mesenchymal transition from its antiproliferative and migratory responses. Mol Cell Biol. 2005;25(18):8108–25.
Shi X, et al. Study of interaction between Smad7 and DNA by single-molecule force spectroscopy. Biochem Biophys Res Commun. 2008;377(4):1284–7.
Cordenonsi M, et al. Links between tumor suppressors: p53 is required for TGF-β gene responses by cooperating with Smads. Cell. 2003;113(3):301–14.
Elston R, Inman GJ. Crosstalk between p53 and TGF-β Signalling. J Signal Transduct. 2012;2012:294097.
Dubrovska A, et al. TGFβ1/Smad3 counteracts BRCA1-dependent repair of DNA damage. Oncogene. 2005;24(14):2289–97.
Zhang S, et al. TGFβ1-induced activation of ATM and p53 mediates apoptosis in a Smad7-dependent manner. Cell Cycle. 2006;5(23):2787–95.
Park S, et al. Smad7 enhances ATM activity by facilitating the interaction between ATM and Mre11-Rad50-Nbs1 complex in DNA double-strand break repair. Cell Mol Life Sci. 2015;72(3):583–96.
Wang M, Saha J, Cucinotta FA. Smad7 foci are present in micronuclei induced by heavy particle radiation. Mut Res Genet Toxicol Environ Mutagen. 2013;756(1):108–14.
Kretzschmar M, Doody J, Massagu J. Opposing BMP and EGF signalling pathways converge on the TGF-β family mediator Smad1. Nature. 1997;389(6651):618–22.
Nagata H, et al. Inhibition of c‐Jun NH2‐terminal kinase switches Smad3 signaling from oncogenesis to tumor‐suppression in rat hepatocellular carcinoma. Hepatology. 2009;49(6):1944–53.
Matsuura I, et al. Cyclin-dependent kinases regulate the antiproliferative function of Smads. Nature. 2004;430(6996):226–31.
Lebrun J-J. The dual role of TGF in human cancer: from tumor suppression to cancer metastasis. Int Scholar Res Notice Mol Biol. 2012;2012:381428.
Seoane J, et al. Integration of Smad and forkhead pathways in the control of neuroepithelial and glioblastoma cell proliferation. Cell. 2004;117(2):211–23.
Asanuma H, et al. Survivin expression is regulated by coexpression of human epidermal growth factor receptor 2 and epidermal growth factor receptor via phosphatidylinositol 3-kinase/AKT signaling pathway in breast cancer cells. Cancer Res. 2005;65(23):11018–25.
Shin S, et al. An anti-apoptotic protein human survivin is a direct inhibitor of caspase-3 and-7. Biochemistry. 2001;40(4):1117–23.
Wang J, et al. Transforming growth factor β induces apoptosis through repressing the phosphoinositide 3-kinase/AKT/survivin pathway in colon cancer cells. Cancer Res. 2008;68(9):3152–60.
Shin I, et al. Transforming growth factor β enhances epithelial cell survival via Akt-dependent regulation of FKHRL1. Mol Biol Cell. 2001;12(11):3328–39.
Yi JY, Shin I, Arteaga CL. Type I transforming growth factor β receptor binds to and activates phosphatidylinositol 3-kinase. J Biol Chem. 2005;280(11):10870–6.
Grünert S, Jechlinger M, Beug H. Diverse cellular and molecular mechanisms contribute to epithelial plasticity and metastasis. Nat Rev Mol Cell Biol. 2003;4(8):657–65.
Grusch M, et al. The crosstalk of RAS with the TGF-β family during carcinoma progression and its implications for targeted cancer therapy. Curr Cancer Drug Targets. 2010;10(8):849–57.
Takai E, Tsukimoto M, Kojima S. TGF-β1 downregulates COX-2 expression leading to decrease of PGE2 production in human lung cancer A549 cells, which is involved in fibrotic response to TGF-β1. Plos One. 2013;8(10):e76346.
Minn AJ, et al. Genes that mediate breast cancer metastasis to lung. Nature. 2005;436(7050):518–24.
Mazhar D, Ang R, Waxman J. COX inhibitors and breast cancer. Br J Cancer. 2006;94(3):346–50.
Neil JR, et al. Cox-2 inactivates Smad signaling and enhances EMT stimulated by TGF-β through a PGE2-dependent mechanisms. Carcinogenesis. 2008;29(11):2227–35.
Zhao M, et al. Mediator MED15 modulates transforming growth factor beta (TGFβ)/Smad signaling and breast cancer cell metastasis. J Mol Cell Biol. 2013;5(1):57–60.
Wakefield LM, Roberts AB. TGF-β signaling: positive and negative effects on tumorigenesis. Curr Opin Genet Dev. 2002;12(1):22–9.
Xu J, Attisano L. Mutations in the tumor suppressors Smad2 and Smad4 inactivate transforming growth factor β signaling by targeting Smads to the ubiquitin–proteasome pathway. Proc Natl Acad Sci. 2000;97(9):4820–5.
Pardali K, Moustakas A. Actions of TGF-β as tumor suppressor and pro-metastatic factor in human cancer. Biochim Biophys Acta. 2007;1775(1):21–62.
Thiery JP, Chopin D. Epithelial cell plasticity in development and tumor progression. Cancer Metastasis Rev. 1999;18(1):31–42.
Levy L, Hill CS. Alterations in components of the TGF-β superfamily signaling pathways in human cancer. Cytokine Growth Factor Rev. 2006;17(1):41–58.
Izzi L, Attisano L. Ubiquitin-dependent regulation of TGβ signaling in cancer. Neoplasia. 2006;8(8):677–88.
Suzuki A, et al. Identification of SMURF1 as a possible target for 7q21. 3‐22.1 amplification detected in a pancreatic cancer cell line by in‐house array‐based comparative genomic hybridization. Cancer Sci. 2008;99(5):986–94.
Fukuchi M, et al. High-level expression of the Smad ubiquitin ligase Smurf2 correlates with poor prognosis in patients with esophageal squamous cell carcinoma. Cancer Res. 2002;62(24):7162–5.
Chen C, Matesic LE. The Nedd4-like family of E3 ubiquitin ligases and cancer. Cancer Metastasis Rev. 2007;26(3-4):587.
Halder SK, et al. Oncogenic function of a novel WD-domain protein, STRAP, in human carcinogenesis. Cancer Res. 2006;66(12):6156–66.
Dupont S, et al. Germ-layer specification and control of cell growth by Ectodermin, a Smad4 ubiquitin ligase. Cell. 2005;121(1):87–99.
Sahai E, et al. Smurf1 regulates tumor cell plasticity and motility through degradation of RhoA leading to localized inhibition of contractility. J Cell Biol. 2007;176(1):35–42.
Zhang H, Cohen SN. Smurf2 up-regulation activates telomere-dependent senescence. Genes Dev. 2004;18(24):3028–40.
Maurice D, et al. Loss of Smad4 Function in pancreatic tumors C-terminal Truncation leads to decreased stability. J Biol Chem. 2001;276(46):43175–81.
Lönn P, et al. Regulating the stability of TGFβ receptors and Smads. Cell Res. 2009;19(1):21–35.
Sun Y, et al. SnoN and Ski protooncoproteins are rapidly degraded in response to transforming growth factor β signaling. Proc Natl Acad Sci. 1999;96(22):12442–7.
Le Scolan E, et al. Transforming growth factor-β suppresses the ability of Ski to inhibit tumor metastasis by inducing its degradation. Cancer Res. 2008;68(9):3277–85.
Levy L, et al. Arkadia activates Smad3/Smad4-dependent transcription by triggering signal-induced SnoN degradation. Mol Cell Biol. 2007;27(17):6068–83.
Zhang Y, et al. Regulation of Smad degradation and activity by Smurf2, an E3 ubiquitin ligase. Proc Natl Acad Sci. 2001;98(3):974–9.
Morén A, et al. Degradation of the tumor suppressor Smad4 by WW and HECT domain ubiquitin ligases. J Biol Chem. 2005;280(23):22115–23.
Du S, Barcellos-Hoff MH. Tumors as organs: biologically augmenting radiation therapy by inhibiting transforming growth factor β activity in carcinomas. Semin Radiat Oncol. 2013;23:242.
Hardee ME, et al. Resistance of glioblastoma-initiating cells to radiation mediated by the tumor microenvironment can be abolished by inhibiting transforming growth factor-β. Cancer Res. 2012;72(16):4119–29.
Zhang M, et al. Blockade of TGF-β signaling by the TGFβR-I kinase inhibitor LY2109761 enhances radiation response and prolongs survival in glioblastoma. Cancer Res. 2011;71(23):7155–67.
Ma S, et al. MicroRNA-616 induces androgen-independent growth of prostate cancer cells by suppressing expression of tissue factor pathway inhibitor TFPI-2. Cancer Res. 2011;71(2):583–92.
Shi X-B, Tepper CG, deVere White RW. Cancerous miRNAs and their regulation. Cell Cycle. 2008;7(11):1529–38.
Guo L, et al. MicroRNAs, TGF-β signaling, and the inflammatory microenvironment in cancer. Tumor Biol. 2016;37(1):115–25.
Goto Y, et al. Regulation of E3 ubiquitin ligase-1 (WWP1) by microRNA-452 inhibits cancer cell migration and invasion in prostate cancer. Br J Cancer. 2016;114:1135.
Wang W, et al. MicroRNA-497 inhibition of ovarian cancer cell migration and invasion through targeting of SMAD specific E3 ubiquitin protein ligase 1. Biochem Biophys Res Commun. 2014;449(4):432–7.
Yu J, et al. MicroRNA-182 targets SMAD7 to potentiate TGFβ-induced epithelial-mesenchymal transition and metastasis of cancer cells. Nat Commun. 2016;7:13884.
Mishra S, et al. Androgen receptor and microRNA-21 axis downregulates transforming growth factor beta receptor II (TGFBR2) expression in prostate cancer. Oncogene. 2014;33(31):4097–106.
Xia H, Ooi LLP, Hui KM. MicroRNA‐216a/217‐induced epithelial‐mesenchymal transition targets PTEN and SMAD7 to promote drug resistance and recurrence of liver cancer. Hepatology. 2013;58(2):629–41.
Jiang F, et al. The repressive effect of miR-148a on TGF beta-SMADs signal pathway is involved in the glabridin-induced inhibition of the cancer stem cells-like properties in hepatocellular carcinoma cells. PloS One. 2014;9(5):e96698.
Bai WD, et al. MiR-200c suppresses TGF-β signaling and counteracts trastuzumab resistance and metastasis by targeting ZNF217 and ZEB1 in breast cancer. Int J Canc. 2014;135(6):1356–68.
Yang H, et al. MicroRNA-140-5p suppresses tumor growth and metastasis by targeting transforming growth factor β receptor 1 and fibroblast growth factor 9 in hepatocellular carcinoma. Hepatology. 2013;58(1):205–17.
Li Q, et al. MicroRNA-25 functions as a potential tumor suppressor in colon cancer by targeting Smad7. Cancer Lett. 2013;335(1):168–74.
Keklikoglou I, et al. MicroRNA-520/373 family functions as a tumor suppressor in estrogen receptor negative breast cancer by targeting NF-κB and TGF-β signaling pathways. Oncogene. 2012;31(37):4150–63.
Cai J, et al. miR-205 targets PTEN and PHLPP2 to augment AKT signaling and drive malignant phenotypes in non-small cell lung cancer. Cancer Res. 2013;73(17):5402–15.
Gregory PA, et al. An autocrine TGF-β/ZEB/miR-200 signaling network regulates establishment and maintenance of epithelialmesenchymal transition. Mol Biol Cell. 2011;22(10):1686–98.
Zeng Y, et al. Repression of Smad4 by miR-205 moderates TGF-β-induced epithelial-mesenchymal transition in A549 cell lines. Int J Oncol. 2016;49(2):700–8.
Ji H, et al. Inhibition of transforming growth factor beta/SMAD signal by MiR-155 is involved in arsenic trioxide-induced anti-angiogenesis in prostate cancer. Cancer Sci. 2014;105(12):1541–9.
Zhang R, et al. Upregulation of microRNA-574-3p in a human gastric cancer cell line AGS by TGF-β1. Gene. 2017;605:63.
Chiyomaru T, et al. Genistein up-regulates tumor suppressor microRNA-574-3p in prostate cancer. Plos One. 2013;8(3):e58929.
Blahna MT, Hata A. Smad-mediated regulation of microRNA biosynthesis. Fed Eur Biochem Soc Lett. 2012;586(14):1906–12.
Butz H, et al. Crosstalk between TGF-β signaling and the microRNA machinery. Trends Pharmacol Sci. 2012;33(7):382–93.
McDonald RA, et al. MicroRNA and vascular remodelling in acute vascular injury and pulmonary vascular remodelling. Cardiovasc Res. 2011;93:594.
Wang B, et al. miR-200a prevents renal fibrogenesis through repression of TGF-β2 expression. Diabetes. 2011;60(1):280–7.
Davis-Dusenbery BN, et al. Down-regulation of Krüppel-like Factor-4 (KLF4) by microRNA-143/145 is critical for modulation of vascular smooth muscle cell phenotype by transforming growth factor-β and bone morphogenetic protein 4. J Biol Chem. 2011;286(32):28097–110.
Hata A, Davis BN. Control of microRNA biogenesis by TGFβ signaling pathway—a novel role of Smads in the nucleus. Cytokine Growth Factor Rev. 2009;20(5):517–21.
Davis BN, et al. Smad proteins bind a conserved RNA sequence to promote microRNA maturation by Drosha. Mol Cell. 2010;39(3):373–84.
Hasanpourghadi M, et al. Targeting of tubulin polymerization and induction of mitotic blockage by Methyl 2-(5-fluoro-2-hydroxyphenyl)-1 Hbenzo [d] imidazole-5-carboxylate (MBIC) in human cervical cancer HeLa cell. J Exp Clin Cancer Res. 2016;35(1):1.
Hasanpourghadi M, et al. Mechanisms of the anti-tumor activity of Methyl 2-(-5-fluoro-2-hydroxyphenyl)-1 H-benzo[d]imidazole-5-carboxylate against breast cancer in vitro and in vivo. Oncotarget. 2017;8:28840.
Hasanpourghadi M, et al. Phytometabolites targeting warburg effect in cancer cells: a mechanistic review. Curr Drug Targets. 2017;18:1086.
Ganai AA, et al. Genistein modulates the expression of NF-κB and MAPK (p-38 and ERK1/2), thereby attenuating d-Galactosamine induced fulminant hepatic failure in Wistar rats. Toxicol Appl Pharmacol. 2015;283(2):139–46.
Vassilev LT, et al. In vivo activation of the p53 pathway by small-molecule antagonists of MDM2. Science. 2004;303(5659):844–8.
Wu Y, et al. Nutlin-3 inhibits epithelial–mesenchymal transition by interfering with canonical transforming growth factor-β1-Smad-Snail/Slug axis. Cancer Lett. 2014;342(1):82–91.
Da C, et al. Nobiletin inhibits epithelial-mesenchymal transition of human non-small cell lung cancer cells by antagonizing the TGF-β1/Smad3 signaling pathway. Oncol Rep. 2016;35(5):2767–74.
Mock CD, Jordan BC, Selvam C. Recent advances of curcumin and its analogues in breast cancer prevention and treatment. R Soc Chem Adv. 2015;5(92):75575–88.
Balta C, et al. Chrysin attenuates liver fibrosis and hepatic stellate cell activation through TGF-β/Smad signaling pathway. Chem Biol Interact. 2015;240:94–101.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Hasanpourghadi, M., Mustafa, M.R. (2018). TGF-β/Smad Signalling Pathway in Cancer. In: Fayyaz, S., Farooqi, A. (eds) Recent Trends in Cancer Biology: Spotlight on Signaling Cascades and microRNAs. Springer, Cham. https://doi.org/10.1007/978-3-319-71553-7_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-71553-7_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-71552-0
Online ISBN: 978-3-319-71553-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)