Abstract
Objectives: Retrospective data from patients with severe traumatic brain injury (TBI) indicate that deviation from the continuously calculated pressure reactivity-based “optimal” cerebral perfusion pressure (CPPopt) is associated with worse patient outcome. The objective of this study was to assess the relationship between prospectively collected CPPopt data and patient outcome after TBI.
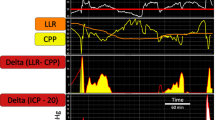
Methods: We prospectively collected intracranial pressure (ICP) monitoring data from 231 patients with severe TBI at Addenbrooke’s Hospital, UK. Uncleaned arterial blood pressure and ICP signals were recording using ICM+® software on dedicated bedside computers. CPPopt was determined using an automatic curve fitting procedure of the relationship between pressure reactivity index (PRx) and CPP using a 4-h window, as previously described. The difference between an instantaneous CPP value and its corresponding CPPopt value was denoted every minute as ΔCPPopt. A negative ΔCPPopt that was associated with impaired PRx (>+0.15) was denoted as being below the lower limit of reactivity (LLR). Glasgow Outcome Scale (GOS) score was assessed at 6 months post-ictus.
Results: When ΔCPPopt was plotted against PRx and stratified by GOS groupings, data belonging to patients with a more unfavourable outcome had a U-shaped curve that shifted upwards. More time spent with a ΔCPPopt value below the LLR was positively associated with mortality (area under the receiver operating characteristic curve = 0.76 [0.68–0.84]).
Conclusions: In a recent cohort of patients with severe TBI, the time spent with a CPP below the CPPopt-derived LLR is related to mortality. Despite aggressive CPP- and ICP-oriented therapies, TBI patients with a fatal outcome spend a significant amount of time with a CPP below their individualised CPPopt, indicating a possible therapeutic target.
Similar content being viewed by others
References
Carney N, Totten AM, O’reilly C, et al. Guidelines for the management of severe traumatic brain injury. Neurosurgery. 2017;80(1):6–15.
Le Roux P, Menon DK, Citerio G, et al. Consensus summary statement of the International Multidisciplinary Consensus Conference on Multimodality Monitoring in Neurocritical Care. Neurocrit Care. 2014;21:1189–209.
Donnelly J, Budohoski KP, Smielewski P, Czosnyka M. Regulation of the cerebral circulation: bedside assessment and clinical implications. Crit Care. 2016;20:129.
Steiner LA, Czosnyka M, Piechnik SK, Smielewski P, Chatfield D, Menon DK, Pickard JD. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med. 2002;30:733–8.
Aries MJH, Czosnyka M, Budohoski KP, et al. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40:2456–63.
Young AMH, Donnelly J, Czosnyka M, et al. Continuous multimodality monitoring in children after traumatic brain injury—preliminary experience. PLoS One. 2016;11:e0148817.
Depreitere B, Güiza F, Van den Berghe G, Schuhmann MU, Maier G, Piper I, Meyfroidt G (2014) Pressure autoregulation monitoring and cerebral perfusion pressure target recommendation in patients with severe traumatic brain injury based on minute-by-minute monitoring data. J Neurosurg 120:1451–1451457.
Guiza F, Depreitere B, Schuhmann M, Van Den Berghe G, Meyfroidt G. Development of a low-frequency autoregulation index for calculation of optimal CPP in severe traumatic brain injury. J Crit Care. 2013;28:e8.
Donnelly J, Czosnyka M, Adams H, et al. Individualizing thresholds of cerebral perfusion pressure using estimated limits of autoregulation. Crit Care Med. 2017;45(9):1464–71.
Menon DK. Cerebral protection in severe brain injury: physiological determinants of outcome and their optimisation. Br Med Bull. 1999;55:226–58.
Jennett B, Bond M. Assessment of outcome after severe brain damage: a practical scale. Lancet. 1975;1:480–1484.
Donnelly J, Aries MJH, Czosnyka M. Further understanding of cerebral autoregulation at the bedside: possible implications for future therapy. Expert Rev Neurother. 2015;15:169–85.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. http://www.r-project.org/
Wickham H, Francois R (2016) dplyr: a grammar of data manipulation. In: R Packag. version 0.5.0. http://cran.r-project.org/package=dplyr.
Wickham H. Elegant graphics for data analysis. New York: Springer; 2009. https://doi.org/10.1007/978-0-387-98141-3.
Venables WN, Ripley BD. Modern applied statistics with S. Technometrics. 2002. https://doi.org/10.1198/tech.2003.s33.
Lewis PM, Czosnyka M, Carter BG, Rosenfeld JV, Paul E, Singhal N, Butt W. Cerebrovascular pressure reactivity in children with traumatic brain injury. Pediatr Crit Care Med. 2015;16:739–49.
Dias C, Silva MJ, Pereira E, et al. Optimal cerebral perfusion pressure management at bedside: a single-center pilot study. Neurocrit Care. 2015. https://doi.org/10.1007/s12028-014-0103-8.
Brady KM, Lee JK, Kibler KK, Easley RB, Koehler RC, Shaffner DH (2008) Continuous measurement of autoregulation by spontaneous fluctuations in cerebral perfusion pressure: comparison of 3 methods. Stroke 39:2531–2532537.
Sorrentino E, Diedler J, Kasprowicz M, et al. Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocrit Care. 2012;16:258–66.
Financial Support for This Project
No specific funding for this study.
Conflicts of interest statement
Authors MC and PS declare receiving a fraction of the licensing fees of the software, ICM+ (licensed by Cambridge Enterprise, United Kingdom), used for data collection and analysis in this study.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this paper
Cite this paper
Donnelly, J. et al. (2018). Pressure Reactivity-Based Optimal Cerebral Perfusion Pressure in a Traumatic Brain Injury Cohort. In: Heldt, T. (eds) Intracranial Pressure & Neuromonitoring XVI. Acta Neurochirurgica Supplement, vol 126. Springer, Cham. https://doi.org/10.1007/978-3-319-65798-1_43
Download citation
DOI: https://doi.org/10.1007/978-3-319-65798-1_43
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-65797-4
Online ISBN: 978-3-319-65798-1
eBook Packages: MedicineMedicine (R0)