Abstract
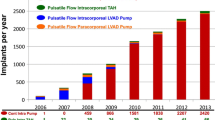
Heart failure (HF) continues to place a significant burden on the current healthcare system. In 2012, the total direct medical cost for HF was $20.9 billion, and this is expected to increase to $53.1 billion in 2030 (representing a 2.5-fold increase). The majority of these costs are related to hospitalization [1]. Left ventricular assist devices (LVAD) were developed to provide end-stage heart failure patients opportunities to wait for a heart on a bridge-to-heart transplant (BTT) strategy or improve survival for those who were not eligible for heart transplantation on a destination therapy (DT) pathway. Since the Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure (REMATCH) trial reported a 48% reduction in risk of death in patients with advanced heart failure with the HeartMate XVE LVAD versus medical management, there has been an exponential increase in the number of mechanical circulatory assist devices for NYHA class IIIB/IV, stage D heart failure [2]. The HeartMate II study reported a significant survival advantage of continuous-flow ventricular assist devices (CF-VAD) over the older pulsatile HeartMate XVE device in a BTT strategy and opened the door for continuous-flow VADs (CF-VAD) that have since become standard of care [3].
Similar content being viewed by others
References
Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–19.
Rose E, Gelijns A, Moskowitz A, et al. Long-term mechanical left ventricular assistance for end-stage heart failure. N Engl J Med. 2001;345:1435–43.
Miller LW, Pagani FD, Russell SD, et al. Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med. 2007;357:885–96.
Kirklin JK, Naftel DC, Pagani FD, Kormos RL, Stevenson LW, Blume ED, Myers SL, Miller MA, Baldwin JT, Young JB. Seventh INTERMACS annual report: 15,000 patients and counting. J Heart Lung Transplant. 2015;34(12):1495–504.
Takeda K, et al. Outcome of unplanned right ventricular assist device support for severe right heart failure after implantable left ventricular assist device insertion. J Heart Lung Transplant. 2014;33(2):141–8.
Kirklin JK, et al. Second INTERMACS annual report: more than 1,000 primary left ventricular assist device implants. J Heart Lung Transplant. 2010;29(1):1–10.
Haddad F, et al. Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117(11):1436–48.
Santamore WP, Dell’Italia LJ. Ventricular interdependence: significant left ventricular contributions to right ventricular systolic function. Prog Cardiovasc Dis. 1998;40(4):289–308.
Santamore WP, Gray L Jr. Significant left ventricular contributions to right ventricular systolic function. Mechanism and clinical implications. Chest. 1995;107(4):1134–45.
Hoffman D, Sisto D, Frater RW, Nikolic SD. Left-to- right ventricular interaction with a noncontracting right ventricle. J Thorac Cardiovasc Surg. 1994;107:1496–502.
Leo G. Kevin, Matthew Barnard; right ventricular failure. Contin Educ Anaesth Crit Care Pain. 2007;7(3):89–94.
Dell’Italia LJ, Walsh RA. Application of a time varying elastance model to right ventricular performance in man. Cardiovasc Res. 1988;22:864–74.
Feneley MP, Gavaghan TP, Baron DW, Branson JA, Roy PR, Morgan JJ. Contribution of left ventricular contraction to the generation of right ventricular systolic pressure in the human heart. Circulation. 1985;71:473–80.
Klima UP, Lee MY, Guerrero JL, et al. Determinants of maximal right ventricular function: role of septal shifts. J Thorac Cardiovasc Surg. 2002;123:72–80.
Bernheim D. De l’asystolie veineuse dans rhyper tro-phie due coer gauche par stenose concomitante du ventricule droit. Rev Med. 1910;39:785.
Henderson Y, Prince AL. The relative systolic discharges of the right and left ventricles and their bearing on pulmonary congestion and depletion. Heart. 1914;5:217–22.
Dexter L. Atrial septal defect. Br Heart J. 1956;18:209.
Lang RM, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1–39.e14.
Lang RM, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440–63.
Cameli M, et al. Evaluation of right ventricular function in the management of patients referred for left ventricular assist device therapy. Transplant Proc. 2015;47(7):2166–8.
Grant AD, et al. Independent and incremental role of quantitative right ventricular evaluation for the prediction of right ventricular failure after left ventricular assist device implantation. J Am Coll Cardiol. 2012;60(6):521–8.
Morine KJ, et al. Pulmonary artery pulsatility index is associated with right ventricular failure after left ventricular assist device surgery. J Card Fail. 2016;22(2):110–6.
Dang NC, Topkara VK, Mercando M, et al. Right heart failure after left ventricular assist device implantation in patients with chronic congestive heart failure. J Heart Lung Transplant. 2006;25:1–6.
Kukucka M, Stepanenko A, Potapov E, Krabatsch T, Redlin M, Mladenow A, et al. Right-to-left ventricular end-diastolic diameter ratio and prediction of right ventricular failure with continuous-flow left ventricular assist devices. J Heart Lung Transplant. 2011;30:64–9.
Matthews JC, Koelling TM, Pagani FD, et al. The right ventricular failure risk score a pre-operative tool for assessing the risk of right ventricular failure in left ventricular assist device candidates. J Am Coll Cardiol. 2008;51:2163–72.
Kormos RL, Teuteberg JJ, Pagani FD, et al. Right ventricular failure in patients with the HeartMate II continuous-flow left ventricular assist device: incidence, risk factors, and effect on outcomes. J Thorac Cardiovasc Surg. 2010;139:1316–24.
Ochiai Y, McCarthy PM, Smedira NG, et al. Predictors of severe right ventricular failure after implantable left ventricular assist system insertion: analysis of 245 patients. Circulation. 2002;106(12 Suppl 1):I198–202.
Atluri P, Goldstone AB, Fairman AS, et al. Predicting right ventricular failure in the modern, continuous flow left ventricular assist device era. Ann Thorac Surg. 2013;96:857–64.
Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS). Appendix A: adverse event definitions: adult and pediatric patients; 2013.
Dandel M, Krabatsch T, Falk V. Left ventricular vs. biventricular mechanical support: decision making and strategies for avoidance of right heart failure after left ventricular assist device implantation. Int J Cardiol. 2015;198:241–50.
Ondrus T, et al. Right ventricular myocardial infarction: from pathophysiology to prognosis. Exp Clin Cardiol. 2013;18(1):27–30.
Farrar DJ, Compton PG, Hershon JJ, et al. Right heart interaction with the mechanically assisted left heart. World J Surg. 1985;9:89–102.
Moon MR, Bolger AF, DeAnda A, et al. Septal function during left ventricular unloading. Circulation. 1997;95:1320–7.
Morgan JA, Paone G, Nemeh HW, et al. Impact of continuous-flow left ventricular assist device support on right ventricular function. J Heart Lung Transplant. 2013;32:398–403.
Piacentino V 3rd, Williams ML, Depp T, Garcia-Huerta K, Blue L, Lodge AJ, Mackensen GB, Swaminathan M, Rogers JG, Milano CA. Impact of tricuspid valve regurgitation in patients treated with implantable left ventricular assist devices. Ann Thorac. 2011;91:1342–7.
Brisco M, Sundareswaran K, Milano, et al. The incidence, risk, and consequences of atrial arrhythmias in patients with continuous-flow left ventricular assist devices. J Card Surg. 2014;29:572–80.
Cantillon DJ, Saliba WI, Wazni OM, Kanj M, Starling RC, Tang WH, Wilkoff BL. Low cardiac output associated with ventricular tachyarrhythmias in continuous-flow LVAD recipients with a concomitant ICD (LoCo VT study). J Heart Lung Transplant. 2014;33(3):318–20.
Kalogeropoulos AP, et al. Validation of clinical scores for right ventricular failure prediction after implantation of continuous-flow left ventricular assist devices. J Heart Lung Transplant. 2015;34(12):1595–603.
Fukamachi K, McCarthy PM, Smedira NG, Vargo RL, Starling RC, Young JB. Preoperative risk factors for right ventricular failure after implantable left ventricular assist device insertion. Ann Thorac Surg. 1999;68(6):2181–4.
Drakos SG, Janicki L, Horne BD, et al. Risk factors predictive of right ventricular failure after left ventricular assist device implantation. Am J Cardiol. 2010;105:1030–5.
Fitzpatrick JF 3rd, Frederick JR, Hsu VM, et al. Risk score derived from preoperative data analysis predicts the need for biventricular mechanical circulatory support. J Heart Lung Transplant. 2008;27:1286–92.
Puwanant S, Hamilton KK, Klodell CT, et al. Tricuspid annular motion as a predictor of severe right ventricular failure after left ventricular assist device implantation. J Heart Lung Transplant. 2008;27:1102–7.
Vivo RP, Cordero-Reyes AM, Qamar U, et al. Increased right-to-left ventricle diameter ratio is a strong predictor of right ventricular failure after left ventricular assist device. J Heart Lung Transplant. 2013;32:792–9.
Cameli M, Lisi M, Righini FM, et al. Speckle tracking echocardiography as a new technique to evaluate right ventricular function in patients with left ventricular assist device therapy. J Heart Lung Transplant. 2013;32:424–30.
Kiernan MS, French AL, DeNofrio D, Parmar YJ, Pham DT, Kapur NK, Pandian NG, Patel AR. Preoperative three-dimensional echocardiography to assess risk of right ventricular failure after left ventricular assist device surgery. J Card Fail. 2015;21(3):189–97.
Cordtz J, et al. Right ventricular failure after implantation of a continuous-flow left ventricular assist device: early haemodynamic predictors. Eur J Cardiothorac Surg. 2014;45(5):847–53.
Lampert BC, Teuteberg JJ. Right ventricular failure after left ventricular assist devices. J Heart Lung Transplant. 2015;34(9):1123–30.
Van Meter CH Jr. Right heart failure: best treated by avoidance. Ann Thorac Surg. 2001;71(3):S220–2.
Argiriou M, et al. Right heart failure post left ventricular assist device implantation. J Thorac Dis. 2014;6(Suppl 1):S52–9.
Kaplon RJ, et al. Vitamin K reduces bleeding in left ventricular assist device recipients. J Heart Lung Transplant. 1999;18(4):346–50.
Houston BA, et al. Right ventricular afterload sensitivity dramatically increases after left ventricular assist device implantation: a multi-center hemodynamic analysis. J Heart Lung Transplant. 2016;35(7):868–76.
Marzec LN, Ambardekar AV. Preoperative evaluation and perioperative management of right ventricular failure after left ventricular assist device implantation. Semin Cardiothorac Vasc Anesth. 2013;17(4):249–61.
Potapov E, Meyer D, Swaminathan M, et al. Inhaled nitric oxide after left ventricular assist device implantation: a prospective, randomized, double-blind, multicenter, placebo-controlled trial. J Heart Lung Transplant. 2011;30(8):870–8.
Tedford RJ, Hemnes AR, Russell SD, et al. PDE5A inhibitor treatment of persistent pulmonary hypertension after mechanical circulatory support. Circ Heart Fail. 2008;1(4):213–9.
Klodell CT Jr, et al. Effect of sildenafil on pulmonary artery pressure, systemic pressure, and nitric oxide utilization in patients with left ventricular assist devices. Ann Thorac Surg. 2007;83(1):68–71; discussion 71.
Baker WL, Radojevic J, Gluck JA. Systematic review of phosphodiesterase-5 inhibitor use in right ventricular failure following left ventricular assist device implantation. Artif Organs. 2016;40(2):123–8.
Fitzpatrick JR, Frederick JR, Hiesinger W, et al. Early planned institution of biventricular mechanical circulatory support results in improved outcomes compared with delayed conversion of a left ventricular assist device to a biventricular assist device. J Thorac Cardiovasc Surg. 2009;137:971–7.
Morgan JA, John R, Lee BJ, et al. Is severe right ventricular failure in left ventricular assist device recipients a risk factor for unsuccessful bridging to transplant and post-transplant mortality. Ann Thorac Surg. 2004;77:859–63.
Boeken U, et al. Intraaortic balloon pumping in patients with right ventricular insufficiency after cardiac surgery: parameters to predict failure of IABP support. Thorac Cardiovasc Surg. 2009;57(6):324–8.
Tanaka A, et al. The subclavian intraaortic balloon pump: a compelling bridge device for advanced heart failure. Ann Thorac Surg. 2015;100(6):2151–2157; discussion 2157–8.
Darrah WC, et al. Intraaortic balloon counterpulsation improves right ventricular failure resulting from pressure overload. Ann Thorac Surg. 1997;64(6):1718–23; discussion 1723–4.
Ntalianis A, et al. Prolonged intra-aortic balloon pump support in biventricular heart failure induces right ventricular reverse remodeling. Int J Cardiol. 2015;192:3–8.
Sintek MA, et al. Intra-aortic balloon Counterpulsation in patients with chronic heart failure and cardiogenic shock: clinical response and predictors of stabilization. J Card Fail. 2015;21(11):868–76.
Imamura T, et al. Prophylactic intra-aortic balloon pump before ventricular assist device implantation reduces perioperative medical expenses and improves postoperative clinical course in INTERMACS profile 2 patients. Circ J. 2015;79(9):1963–9.
Kapur NK, Paruchuri V, Korabathina R, et al. Effects of percutaneous mechanical circulatory support device for medically refractory right ventricular failure. J Heart Lung Transplant. 2011;30:1360–7.
Lima B, et al. Effectiveness and safety of the Impella 5.0 as a bridge to cardiac transplantation or durable left ventricular assist device. Am J Cardiol. 2016;117(10):1622–8.
Bansal A, et al. Using the minimally invasive Impella 5.0 via the right subclavian artery cutdown for acute on chronic decompensated heart failure as a bridge to decision. Ochsner J. 2016;16(3):210–6.
Wang Y, et al. Decision tree for adjuvant right ventricular support in patients receiving a left ventricular assist device. J Heart Lung Transplant. 2012;31(2):140–9.
Schibilsky D, et al. Impella 5.0 support in INTERMACS II cardiogenic shock patients using right and left axillary artery access. Artif Organs. 2015;39(8):660–3.
Bhama JK, Kormos RL, Toyoda Y, et al. Clinical experience using the Levitronix CentriMag system for temporary right ventricular mechanical support. J Heart Lung Transplant. 2009;28:971–6.
Copeland JG, Smith RG, Arabia FA, et al. Cardiac replacement with a total artificial heart as a bridge to transplantation. N Engl J Med. 2004;351:859.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Gohar, S., Sheth, S., Delgado, R. (2018). Optimization of Right Ventricular Function Preoperatively for LVAD Implantation. In: Morgan, J., Civitello, A., Frazier, O. (eds) Mechanical Circulatory Support for Advanced Heart Failure . Springer, Cham. https://doi.org/10.1007/978-3-319-65364-8_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-65364-8_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-65363-1
Online ISBN: 978-3-319-65364-8
eBook Packages: MedicineMedicine (R0)