Abstract
Cellular grafting for vitiligo has evolved since its inception. Non-cultured cellular grafting has superseded cultured techniques as the preferred modus operandi in clinical practice. The reasons are straightforward: it can be completed in a few hours, does not require the use of xenobiotics (except trypsin) or culture media and is of significantly lower costs. Although it does not offer the possibility of cell expansion and cryopreservation for future transplant, this can be supplanted by harvesting a new piece ultrathin split skin graft. Under proper training, harvesting an ultrathin split skin graft (not beyond the papillary dermis) is fast and results in no or minimal scarring. Innovative methods to simplify non-cultured cellular grafting have also been successfully achieved.
Melanocytes can now be extracted not only from the epidermis for transplantation but from outer root sheath of hair follicles.
Non-cultured cellular grafting has proven to be a safe and effective surgical treatment for stable vitiligo, substantiated by various long-term studies over the last two decades. The imposition of strict legislative regulation on this technique is unwarranted and will only drive up cost and deprive patients’ access to this innovative procedure.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
Change history
18 March 2020
Permission for using the table 11.1 had been acquired from Pigm Mel Research. Hence, caption for Table 11.1 has been corrected to “van Geel N, Speeckaert R, Taieb A et al. Koebner’s phenomenon in vitiligo: European position paper. Pigment Cell
References
Hartmann A, Broecker EB, Hamm H. Repigmentation of skin and hairs in stable vitiligo by transplantation of autologous melanocytes in fibrin suspension. J Eur Acad Dermatol Venereol. 2008;22:624–6.
Gan EY, van Geel N, Goh BK. Repigmentation of leucotrichia in vitiligo with noncultured cellular grafting. Br J Dermatol. 2012;166:196–9.
Eisinger M, Marko O. Selective proliferation of normal human melanocytes in vitro in the presence of phorbol ester and cholera toxin. Proc Natl Acad Sci U S A. 1982;79:2018–22.
Halaban R, Ghosh S, Duray P, Kirkwood JM, Lerner AB. Human melanocytes cultured from naevi and melanomas. J Invest Dermatol. 1986;87:95–101.
Lerner A, Halaban R, Klaus SN, Moellman GE. Transplantation of human melanocytes. J Invest Dermatol. 1987;89:219–24.
Halaban R, Langdon R, Birchall N, et al. Basic fibroblast growth factor from human keratinocytes is a natural mitogen for melanocytes. J Cell Biol. 1988;107:1611–9.
Olsson MJ, Juhlin L. Repigmentation of vitiligo by transplantation of cultured autologous melanocytes. Acta Derm Venereol. 1993;73:49–51.
Löntz W, Olsson MJ, Moellmann G, Lerner AB. Pigment cell transplantation for the treatment of vitiligo: a progress report. J Am Acad Dermatol. 1994;30:591–7.
Olsson MJ, Moellman G, Lerner AB, Juhlin L. Vitiligo: repigmentation with cultured melanocytes after cryostorage. Acta Derm Venereol. 1994;74:226–8.
Kaufmann R, Greiner D, Kippenberger S, Bernd A. Grafting of in vitro cultured melanocytes onto laser-ablated lesions of vitiligo. Acta Derm Venereol. 1998;78:136–8.
Dover JS, Hruza G. Lasers in skin resurfacing. Australas J Dermatol. 2000;41:72–85.
Olsson MJ, Juhlin L. Transplantation of melanocytes in vitiligo. Br J Dermatol. 1995;132:587–91.
Chen YF, Yang PY, Hu DH, Kuo FS, Hung CS, Hung CM. Treatment of vitiligo by transplantation of cultured pure melanocyte suspension: analysis of 120 cases. J Am Acad Dermatol. 2004;51:68–74.
O’Connor NE, Mulliken JB, Banks-Schlegel S, Kehinde O, Green H. Grafting of burns with cultured epithelium prepared from autologous epidermal cells. Lancet. 1981;1:75–8.
Compton CC, Gill JM, Bradford DA, Regauer S, Gallico GG, O’Connor NE. Skin regenerated from cultured epithelial autografts on full-thickness burn wounds from 6 days to 5 years after grafting. Lab Investig. 1989;60:600–12.
Brysk MM, Newton RC, Rajaraman S, et al. Repigmentation of vitiliginous skin by cultured cells. Pigment Cell Res. 1989;2:202–7.
Plott RT, Brysk MM, Newton RC, Raimer SS, Rajaraman S. A surgical treatment for vitiligo: autologous cultured-epithelial grafts. J Dermatol Surg Oncol. 1989;15:1161–6.
Falabella R, Escobar C, Borrero I. Transplantation of in vitro-cultured epidermis bearing melanocytes for repigmenting vitiligo. J Am Acad Dermatol. 1989;21:257–64.
Falabella R, Escobar C, Borrero I. Treatment of refractory and stable vitiligo by transplantation of in vitro cultured epidermal autografts bearing melanocytes. J Am Acad Dermatol. 1992;26:230–6.
Andreassi L, Pianigiani E, Andreassi A, Taddeucci P, Biagioli M. A new model of epidermal culture for the surgical treatment of vitiligo. Int J Dermatol. 1998;37:595–8.
Eves PC, Beck AJ, Shard AG, MacNeil S. A chemically defined surface for the co-culture of melanocytes and keratinocytes. Biomaterials. 2005;26:7068–81.
Beck AJ, Phillips J, Smith-Thomas L, Short RD, Mac Neil S. Development of a plasma-polymerised surface suitable for the transplantation of keratinocyte-melanocyte cocultures for patients with vitiligo. Tissue Eng. 2004;9:1123–1131.
MacNeil S, Eves P, Beck A, Gawkrodger D. Practical issues of delivering cultured melanocytes to vitiligo patients. Proceedings of the 19th International Pigment Cell Conference, VA, USA; 2005.
Gauthier Y, Surleve-Bazeille J. Autologous grafting with noncultured melanocytes: a simplified method for treatment of depigmented lesions. J Am Acad Dermatol. 1992;26:191–4.
Olsson MJ, Juhlin L. Leucoderma treated by transplantation of a basal cell layer enriched suspension. Br J Dermatol. 1998;138:644–8.
Van Geel N, Ongenae K, De Mil M, Naeyaert JM. Modified technique of autologous noncultured epidermal cell transplantation for repigmenting vitiligo: a pilot study. Dermatol Surg. 2001;27:873–6.
Van Geel N, Ongenae K, De Mil M, Haeghen YV, Vervaet C, Naeyaert JM. Double-blind placebo-controlled study of autologous transplanted epidermal cell suspensions for repigmenting vitiligo. Arch Dermatol. 2004;140:1–6.
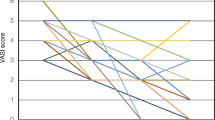
Gan EY, Kong YL, Tan WD, Thng ST, Goh BK. Twelve-month and sixty-month outcomes of noncultured cellular grafting for vitiligo. J Am Acad Dermatol. 2016;75:564–71.
Olsson MJ, Juhlin L. Long-term follow-up of leucoderma patients treated with transplants of autologous cultured melanocytes, ultrathin epidermal sheets and basal cell layer suspension. Br J Dermatol. 2002;147:893–904.
Mulekar SV. Long-term follow-up study of segmental and focal vitiligo treated by autologous, noncultured melanocyte- keratinocyte cell transplantation. Arch Dermatol. 2004;140:1211–5.
Van Geel N, Wallaeys E, Goh BK, De Mil M, Lambert J. Long-term results of noncultured epidermal cellular grafting in vitiligo, halo naevi, piebaldism and naevus depigmentosus. Br J Dermatol. 2010;163:1186–93.
Rao A, Gupta S, Dinda AK, et al. Study of clinical, biochemical and immunological factors determining stability of disease in patients with generalized vitiligo undergoing melanocyte transplantation. Br J Dermatol. 2012;166:1230–6.
Tegta GR, Parsad D, Majumdar S, Kumar B. Efficacy of autologous transplantation of noncultured epidermal suspension in two different dilutions in the treatment of vitiligo. Int J Dermatol. 2006;45:106–10.
Inger R, Hans R. An estimation of the melanocyte mass in humans. J Invest Dermatol. 1983;81:278–81.
Mulekar SV, Ghwish B, Al Issa A, Al Eisa A. Treatment of vitiligo lesions by ReCell® vs. conventional melanocyte–keratinocyte transplantation: a pilot study. Br J Dermatol. 2008;158:45–9.
Goh BK, Chua XM, Chong KL, De Mil M, Van Geel NAC. Simplified cellular grafting for treatment of vitiligo and piebaldism: the “6-well plate” technique. Dermatol Surg. 2010;36:203–7.
Kumar R, Parsad D, Singh C, Yadav S. Four compartment method: a simplified and cost-effective method of noncultured epidermal cell suspension for the treatment of vitiligo. Br J Dermatol. 2014;170:581–5.
Gupta S, Sahni K, Tembhre MJ, Mathur S, Sharma VK. A novel point-of-care in vivo technique for preparation of epidermal cell suspension for transplantation in vitiligo. J Am Acad Dermatol. 2015;72:e65–6.
Randall VA, Jenner TJ, Hibberts NA, et al. Stem cell factor/c-Kit signalling in normal and androgenetic alopecia hair follicles. J Endocrinol. 2008;197:11–23.
Tobin DJ, Paus R. Graying: gerontobiology of the hair follicle pigmentary unit. Exp Gerontol. 2001;36:29–54.
Legue E, Sequeira I, Nicolas JF. Hair follicle renewal: authentic morphogenesis that depends on a complex progression of stem cell lineages. Development. 2010;137:569–77.
Vanscheidt W, Hunziker T. Repigmentation by outer-root-sheath-derived melanocytes: proof of concept in vitiligo and leucoderma. Dermatology. 2009;218:342–3.
Kumar A, Gupta S, Mohanty S, Bhargava B, Airan B. Stem cell niche is partially lost during follicular plucking: a preliminary pilot study. Int J Trichol. 2013;5(2):97–100.
Mohanty S, Kumar A, Dhawan J, Sreenivas V, Gupta S. Noncultured extracted hair follicle outer root sheath cell suspension for transplantation in vitiligo. Br J Dermatol. 2011;164:1241–6.
Vinay K, Dogra S, Parsad D, Kanwar AJ, Kumar R, Minz RW, Saikia UN. Clinical and treatment characteristics determining therapeutic outcome in patients undergoing autologous non-cultured outer root sheath hair follicle cell suspension for treatment of stable vitiligo. J Eur Acad Dermatol Venereol. 2015;29:31–7.
Singh C, Parsad D, Kanwar AJ, Dogra S, Kumar R. Comparison between autologous noncultured extracted hair follicle outer root sheath cell suspension and autologous non cultured epidermal cell suspension in the treatment of stable vitiligo: a randomized study. Br J Dermatol. 2013;169:287–93.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Annex A: Surgical Protocol for NCES (Adopted and Modified from [27])
Annex A: Surgical Protocol for NCES (Adopted and Modified from [27])
-
1.
The first step is always the most important. It is crucial to harvest an ultrathin split skin graft. We usually choose the left lateral hip as the donor site, and the size is one-third to one-fifth the vitiligo area to be transplanted. The donor site is cleansed with chlorhexidine 4% and outlined with skin marking ink, before performing an anaesthetic field block using 2% lignocaine. A silver dermatome is used to harvest a split skin graft not beyond the papillary dermis, which can be gauged by the translucency of the graft (Fig. 36.3a). Too thick a graft will impede trypsinization and can lead to scarring of the donor site. This is a skill to be acquired and a learning curve. It requires the help from an assistant in stretching the skin taut (using, e.g. a sterilized wooden spatula), so that the surface is as flat as possible. Sterile liquid paraffin provides good lubrication for the dermatome to glide on the donor skin surface.
-
2.
The split skin graft is placed in a sterile tray and washed in normal saline, before placing it in a petri dish containing 10 ml of trypsin-EDTA 0.25%, pre-warmed to 37 °C (Fig. 36.3b). The graft is then cut into smaller pieces, and the petri dish is covered and placed in an incubator, set at 37 °C, for 30 min (Fig. 36.3c).
-
3.
After incubation, the petri dish containing the donor tissue is placed in a laminar flow chamber, wherein the extraction of epidermal cells takes place. The lid of the petri dish is lifted, inverted and placed on the benchtop of the chamber. The tissue pieces are removed from trypsin and placed on the inverted lid. Here, using fine forceps, the epidermis is peeled away from the dermis and their surfaces scraped with the forceps to dislodge the epidermal cells including melanocytes.
-
4.
The tissue-cell mixture is then collected and placed into a 50 ml Falcon tube containing 10 ml of PBS. The tube is capped and the suspension mixed by shaking and twirling tube for 30 s. In so doing, the cells will be further dislodged and suspended in the PBS.
-
5.
The suspension is decanted into a petri dish, and 10 ml of soybean trypsin inhibitor is added to neutralize trypsin. The tissue debris are physically removed and discarded from the mixture. The neutralized suspension is then pipetted into a 50-ml Falcon tube, through a 40-μm filter, to remove the residual tissue debris.
-
6.
The filtrate, containing the cell suspension, is then centrifuged at 120 × g for 5–8 min. Epidermal cells will settle to the bottom of the tube as a pellet (Fig. 36.3d). The supernatant is discarded, and the cell pellet is resuspended in 2–5 ml of PBS (depending on the size of the pellet and the area of recipient site).
-
7.
The final suspension is then applied onto laser-ablated or dermabraded vitiliginous recipient sites. The depth of ablation of the recipient area is gauged by pinpoint bleeding. The application of the cell suspension is carried out using a pipetter which offers good control of the amount dispensed. A small amount is applied to avoid run-off, controlled by surface tension of the fluid (Fig. 36.3e). Collagen dressing (Neuskin-F, Eucare, India), cut into small pieces, is then applied to hold the suspension in place (Fig. 36.3f), and the area is further secured with Hypafix dressings (Smith & Nephew, UK) (Fig. 36.3g).
-
8.
The dressings are kept in place for 5–7 days before removal. Post-grafting phototherapy is not required in our experience. Patients can expose the recipient sites to sunlight daily for 5–10 min.
-
9.
If the grafting is successful, signs of repigmentation are usually evident by 4 weeks in Indian, 8 weeks in Chinese (Fig. 36.4a, b) and 12 weeks in Caucasian patients.
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Goh, B.K. (2019). Surgical Therapies. In: Picardo, M., Taïeb, A. (eds) Vitiligo. Springer, Cham. https://doi.org/10.1007/978-3-319-62960-5_36
Download citation
DOI: https://doi.org/10.1007/978-3-319-62960-5_36
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-62958-2
Online ISBN: 978-3-319-62960-5
eBook Packages: MedicineMedicine (R0)