Abstract
Many vector-borne and zoonotic diseases are considered to be emerging; since they are either newly reported to cause human disease, or are causing disease in geographical locations or species not previously documented. In the past 15 years, significant outbreaks of Severe Acute Respiratory Syndrome (or SARS) and Middle Eastern Respiratory Syndrome (or MERS), Nipah and Hendra, Ebola virus disease and Zika fever and others have been reported. In this chapter the clinical characteristics, epidemiological aspects, treatment and prevention and information related to the laboratory investigation of important zoonotic and vector-borne diseases that have emerged in the past 10 years, and how this affects children, will be discussed. Furthermore rabies, considered a neglected viral disease with the majority of victims in Africa being children, will also be addressed.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
5.1 Hemorrhagic Fevers
The viral hemorrhagic fevers (VHF) are a specific group of diseases that have in common the propensity for human to human transmission particularly in the hospital setting, have high mortality and require early recognition and a public health response to prevent outbreaks. They are caused by unrelated RNA viruses belonging to the Filovirus, Arenavirus, Bunyavirus and Flavivirus genera (reviewed in [1, 2]) (Table 5.1). Subclinical or mild cases are commonly associated with for example Lassa fever, yellow fever and Crimean-Congo hemorrhagic fever (CCHF), contrasted by Ebola virus and Marburg virus disease (EVD and MVD) which are more often associated with severe and fatal outcomes and case fatality rates of up to 90% recorded during outbreaks.
All of the HF viruses are naturally harbored in distinct animal or invertebrate reservoirs. Outbreaks of the disease are either associated with exposure to the virus through a vector species (for example ticks for CCHF virus or mosquitoes for yellow fever) and little or no human-to-human spread, or a single spill-over event from the animal reservoir with amplification of the outbreak through human-to-human transmission (for example spill-over of Ebola virus from bats or other infected forest dwelling animals to humans). Since these viruses are associated with an animal or invertebrate reservoirs and vectors, the diseases have a specifically geographical expanse, partly related to the distribution of these reservoir and vector species. Another observation is that historically, outbreaks of VHFs have been occurring in low resource settings with many of the outbreaks associated with health care facilities where poor infection control practices allow for the spread of these viruses. Recent outbreaks of yellow fever have occurred in high density urban areas with intense mosquito breeding. Infection prevention and control measures in hospitals remain the most important measure to contain a VHF outbreak [3,4,5,6,7]. This is in the absence of prophylaxis or treatment on the account of most of the VHFs. Currently, the only VHF for which a licensed vaccine is available is yellow fever. The vaccine is administered to children over 9 months of age of as part of the expanded program of immunization in a number of yellow fever endemic countries, in mass campaigns and in response to reported outbreaks. Documentation of a high rate of yellow fever vaccine-associated neurotropic disease in young infants during the 1960s led to institution of age <6 months as a contraindication for yellow fever vaccination except during epidemics when the risk of yellow fever virus transmission may be very high [8].
Ribavirin may be useful for treating Lassa fever and CCHF, although not proven in clinical trials [9,10,11,12].
A number of VHF infections such as CCHF are related to occupational exposure to infected vectors or animals so infections in children are less common.
For the purpose of this chapter further discussions will focus on aspects of Ebola virus disease (EVD).
5.1.1 Epidemiological Aspects of EVD
To date, natural outbreaks of EVD have only been recorded in central and west African countries. Before the outbreak of EVD in Guinea, Sierra Leone and Liberia from 2013 to 2015, outbreaks of the disease were limited to secluded and rural locations in central Africa [29]. A cumulative 31,139 cases with 12,890 deaths have been recorded since the first recognition of EVD in 1976–2015, more than 90% of these cases were reported during the West Africa outbreak [30, 31]. Single exported cases during outbreaks have been recorded in travellers with secondary transmission noted during four such events in South Africa, Nigeria, USA and Mali [29]. The common perception is that children are spared during EVD outbreaks, and in fact this observation was made during several outbreak investigations [32]. This does however not mean that children are not affected. A retrospective study revealed that 20 of the 218 (9%) confirmed EVD cases during the 2000 Gulu, Uganda outbreak were in young children and adolescents [33]. Nearly 20% of the cases reported during the West Africa outbreak involved children below the age of 15 [34]. The putative index case of the West Africa outbreak was a 2 year old child that may have had exposure to bats whilst playing in the forest nearby his home [35, 36]. The risk of EVD in children may be related to cultural factors in handling and caring for ill persons within households. In communities where children are kept away from the sick the risk should be lower, but in many instances young children are co-admitted to hospital with their sick caregivers increasing the risk of them also being infected [33]. During the Gulu-outbreak, it was noted that the under-five age group was more affected during this outbreak than other children. Here children were typically co-admitted to hospital with their symptomatic parents [33].
The natural history of Ebola virus (EBOV) remains an enigma despite intensive research on the topic. Evidence is accumulating that certain forest dwelling fruit bat species (including Hypsignathus monstrosus, Epomops franqueti, Myonycteris torquata and possibly Eidolon helvum) are natural reservoirs of the virus although this occurrence is still not fully understood [37,38,39]. The source of EVD outbreaks has often been associated with direct contact with bushmeat [40]. The latter includes bats, chimpanzee, gorillas and duiker antelope [41]. The risk for contact with bushmeat appears to be related to slaughtering and preparation of the raw meat and not necessarily the consumption of cooked meat [41]. Outbreaks of EVD in the human population are amplified by human-to-human transmission through close and direct contact with infected individuals [23]. These outbreaks are perpetuated in the hospital setting but also in close family and friend circles where caring for the ill and traditional burial practices are the most prominent risk factor for contracting the virus.
5.1.2 Clinical Aspects of EVD
The initial stage of the clinical course of EVD is non-specific, complicating early diagnosis, and follows an incubation period of 2–21 days [42]. The difficulty of clinical diagnosis is compounded by a long list of possible differential diagnoses in the locations where EVD has been described. This includes other VHF such as Lassa fever, but also other infectious diseases such as malaria, cholera and typhoid [42,43,44,45]. EVD is characterized by sudden onset of fever (>40 °C (104 °F)), generalized weakness and anorexia, myalgia, headache and sore throat [42, 46, 47]. These were all common findings in children during the EVD outbreak in West Africa [34]. Noteworthy, is that all of the EVD cases reported in children during the 2000 Gulu outbreak reported fever [33]. Patients infected with EVD rapidly deteriorate and commonly present with gastrointestinal symptoms including vomiting, diarrhea and dehydration. Chertow et al. [48] reported profuse watery diarrhea in EVD patients persisting for a week or more. As with other VHF, and contrary to the naming of the syndrome, most cases do not present with overt bleeding [33, 34, 42, 48]. Less than 20% of children diagnosed with EVD presented with bleeding which was reported as hematochezia, hematemesis, bleeding gums, epistaxis and oozing from needle puncture sites [33, 34]. Patients will then either recover or deteriorate, often displaying neurological signs. Patients typically succumb due to multi-organ failure and hypovolemic shock [42]. Common findings in EVD patients with a poor prognosis are rapidly developing leukopenia, thrombocytopenia and a decrease in coagulopathy markers [42, 49, 50].
The case fatality rate in children is high [51]. During the Gulu-outbreak, the reported case fatality rate among children and adolescents was 40% [33]. During the West Africa outbreak, the case fatality rate in the under-five group was significantly higher than other age groups, with the highest death rate reported in children under-1 year old (90%) [34].
Pregnant woman are more likely to develop severe EVD, and miscarriage is reported universally in pregnant woman diagnosed with EVD [48, 52]. A case report of EVD in a pregnant EVD woman that survived, but still aborted suggests that maternal immunity may have little effect on affording protection to the unborn [53].
5.1.3 Laboratory Diagnosis of EVD
Limited capacity for specialized laboratory diagnosis exists in most countries where EVD has been previously reported. This remains one of the biggest challenges in effective outbreak responses for the future [54, 55]. Laboratory investigations are typically carried out by national reference centres and involve specialized testing to detect the virus, or the body’s response to the infection [24, 54, 56]. Specific laboratory confirmation is by reverse transcription (RT)-PCR which detects the viral RNA in a patient’s sample. Antigen detection using enzyme immunosorbent assays (ELISA) are also commonly used. Live virus may also be isolated in cell culture, but typically serves as a complimentary assay and due to the time required for results, not always useful for diagnosis or a timely outbreak response. Detection of specific IgM responses or rise in specific IgG titre is also indicative of recent infection. The latter is tested using indirect immunofluorescence assays or ELISA. Some laboratories may offer additional testing such as electron microscopy and immunohistochemistry on tissue samples, but this may be viewed as complimentary testing in most cases. It is recommended that blood and tissues of suspected EVD cases be handled in biosafety level 4 facilities; although RT-PCR testing during the West Africa EVD outbreak was done under field conditions working under modified biosafety level 3 conditions. The West Africa outbreak has highlighted the need for rapid and sensitive tests for EVD. Tests that can be conducted at facility level or at the bedside will be helpful in directing clinical decisions [55, 57]. Although testing at reference laboratories may be laborious and more time consuming than facility-level testing, it is still recommended that all investigations be confirmed by experienced reference laboratories. Several rapid EVD assays are being developed in response to the West Africa outbreak, but are not yet widely available [58,59,60,61,62,63].
5.1.4 Treatment and Prevention of EVD
Despite tremendous efforts during and following the West Africa outbreak to develop antiviral treatment and vaccines, neither are (widely) available yet [64,65,66]. Management remains supportive in most instances, although experimental treatment options have been applied for some [67, 68]. Fever and pain is managed with paracetamol and it is recommended to avoid nonsteroidal antipyretics [12]. Chertow et al. [48] who managed more than 700 EVD patients in Liberia in 2014 found that the use of antiemetics, antidiarrheal medications, and rehydration therapy was beneficial. Antimalarial treatment is recommended for all suspected EVD cases, and malaria testing is recommended to guide further actions [12]. Treatment with broad spectrum antibiotics is recommended especially in children, aged less than 5 years [12] as empiric treatment for possible bacterial sepsis. Fluid replacement will be required in many EVD patients and blood transfusions, in those with bleeding, may be beneficial [12].
The Ebola virus has been detected in breast milk up to 9 months after infection, and therefore it is not recommended that woman diagnosed with EVD breastfeed [12, 69].
Historically the use of hyperimmune serum for treatment of EVD, but also other VHF cases, has been reported [70,71,72]. During the West Africa outbreak, the WHO also approved the use of hyperimmune serum for the treatment of patients, although reportedly not widely used [73]. A limited clinical trial during the outbreak indicated the safety, acceptability and feasibility of treatment with hyperimmune sera [74]. Van Griensven and co-authors [74] also argued the scalability of such a product, particularly given the number of potential immune donors now available in Guinea, Liberia and Sierra Leone.
During the West Africa outbreak, experimental drug treatment of patients was also reported. Palich and co-workers [67] reported the survival of a 6 year old child diagnosed with EVD after treating with favipiravir (or T-705) until virus was cleared from his blood. The use of favipiravir in children older than 1 year has been suggested by Bouazza and co-workers [75], but data from ongoing trails are not yet available.
Other treatment option developments have focused on the use of antiviral drugs (such as favipiravir), type I interferon, anti-coagulant drugs, small interfering RNA, monoclonal antibodies and morpholino-oligomers [76,77,78]. A number of experimental vaccines have undergone safety and immunogenicity studies in-vivo in various populations, although children have largely not been included in these studies. In phase 3 studies using a ring vaccination approach for post exposure prevention of EBV disease in potential contacts (>18 years of age) a recombinant vesicular stomatitis virus based vaccine (rVSV-ZEBOV) showed very high efficacy [79]. Social mobilization, patient isolation, infection control and use of personal protection equipment by health workers, contact tracing and monitoring for infection and safe burials are key traditional interventions in outbreaks.
5.2 Arboviral Diseases
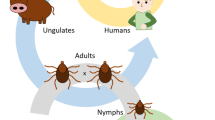
Arboviruses are insect-transmitted viruses belonging to the Flaviviridae, Togaviridae and Bunyaviridae virus families. Hematophagous vectors such as mosquitos, ticks, midges and sandflies transmit the viruses to humans and other susceptible vertebrate hosts. More than 500 arboviruses have been catalogued worldwide, with a little more than a quarter of them reported to cause human disease [80]. The clinical spectrum of arboviral disease is vast ranging from asymptomatic infection to life-threatening febrile and hemorrhagic fever. Arboviral disease typically falls within one of four groups of clinical presentation, namely non-specific systemic febrile disease, encephalitis, polyarthralgia or hemorrhagic fever [81]. Most of the arboviruses are however, not limited to causing only one clinical syndrome. West Nile virus may for example cause unapparent infection in up to 80% of infected individuals but may also cause debilitating encephalitis in others [82]. The distribution of specific arboviruses is geographically defined based on insect vector distribution. Several instances of expanding vector distribution, for example, presumptively due to global climate changes, changes in land use patterns and global transportation have been increasingly linked with the emergence of arboviruses worldwide [83, 84]. Examples include the introduction of West Nile virus to North America in 1999 [85, 86], the re-emergence of dengue in South East Asia, South America and Sub-Sahara Africa [87], the emergence of chikungunya in Indian Ocean Islands and the Caribbean [88], and the emergence of Zika virus (ZIKV) in Latin America in 2014 [89].
Clinical diagnosis of arboviral disease is complicated, and under- or misdiagnosis related to the difficulty of clinical diagnosis in the absence of overt complications is common. In addition, the geographical spread of many arboviruses overlap and have similar clinical manifestations relating to complexity in clinical diagnosis [90]. Specialized diagnostic testing is required to confirm a suspicion of arboviral disease, but is not accessible in many countries where it is probably needed the most. Although RT-PCR detection or virus isolation provide definitive diagnosis, laboratory investigations for arboviral infections mostly rely on serological testing and interpretation due to the typically short viremic period associated with most arboviral infections. Interpretation of serological testing for arboviruses is also challenging and confounded by substantial antigenic cross-reaction between viruses belonging to the same family. The cross-reaction phenomenon particularly applies to flavivirus infections and may be further complicated by possible prior infection with a virus from the same family, or a vaccination for yellow fever or Japanese encephalitis.
For the purpose of this chapter the remainder of the discussion will focus on the newly emerging ZIKV.
5.2.1 Epidemiological Aspects of ZIKV
The WHO declared the ZIKV outbreak in the Americas a Public Health Emergency of International Concern [91]. This followed the rapid emergence of the virus in Brazil and virtually the entire South American subcontinent and the recognition of the potential link in the rise of the number of babies born with microcephaly and other neurological abnormalities observed [92].
The ZIKV was reported for the first time following yellow fever research conducted in the Zika Forest of Uganda in 1947 when it was isolated from a febrile rhesus monkey [93]. It was recognized as a disease causing agent in humans in 1954 when diagnosed in febrile patients in Nigeria [94]. In the years to follow, ZIKV remained mostly a research curiosity with a handful of studies that described its ecology and sero-prevalence in selected human populations and it caused sporadic cases and limited outbreaks without reported mortality or fetal effects [94,95,96,97,98,99] in a number of countries in Africa and Southeast Asia. In 2007, the first major outbreak of ZIKV was reported from the Yap Islands of Micronesia where more than 70% of the Island’s population was affected [100,101,102]. This was followed by an outbreak in French Polynesia in 2013 and 2014, also affecting nearly 70% of the population [103,104,105,106]. The virus continued to spread westward, and was reported in Chile’s Easter Island in February 2014 [107]. This was followed by detection of the virus in Brazil in May 2015, although molecular studies have suggested that the virus may have been introduced as early as late 2014 [108,109,110]. By September 2016, ZIKV was reported from more than 47 countries in Latin America and the Caribbean [111]. In addition, probably related to increased vigilance for the virus, outbreaks of the disease have been reported from Micronesia, Western Samoa, Figi, Singapore, Tonga, Samoa and the Marshal Islands, with possible endemic transmission reported in a dozen other countries in Southeast Asia and the Pacific since 2015 [111]. Although, these reports may relate to endemic occurrence of the virus, the possibility of autochthonous outbreaks due to translocation of virus from Latin America is under investigation for some of these outbreaks [111].
The ZIKV, a flavivirus, is transmitted to humans primarily through the bite of the female, day-feeding Aedes aegypti mosquito [112]. The role of other mosquito species in transmission of the virus to humans is disputed [113,114,115,116,117,118,119,120,121]. Aedes mosquitoes usually thrive during warm and wet seasons in the tropics and subtropics, with Aedes aegypti particularly well suited for breeding in urban settings, hence the risk of transmission of the virus from infected mosquitos to humans. Although, direct mosquito transmission is mostly implicated in transmission of the ZIKV to humans, transmission in-utero, intrapartum and through sexual transmission has been reported [111, 122,123,124,125,126,127,128,129,130,131,132,133]. Transmission in-utero has been most alarming with the probable link to congenital malformations and microcephaly (see Sect. 5.2.2). Rare cases of transmission through blood transfusion and laboratory exposures have also been reported [105, 134].
5.2.2 Clinical Aspects of ZIKV
Following the bite of an infected mosquito, an incubation period of up to 2 weeks follows, after which some infected individuals will develop the signs and symptoms of ZIKV infection [100]. An estimated 80% of humans becoming infected with the virus will not develop any clinical signs of disease. In the remainder, disease is typically acute but mild and self-resolving [100, 135]. This is marked by a low-grade fever (typically not above 38.5 °C (101.3 °F)), arthralgia, a maculopapular rash, conjunctivitis, headache and asthenia, much like dengue fever [100, 135]. Clinical diagnosis of ZIKV infection is complicated due to its non-specific presentation, but also due to the co-circulation of other arboviruses such as dengue and chikungunya viruses which cause clinically indistinguishable disease in most cases. Co-infection of ZIKV and dengue or chikungunya virus has also been reported [90, 136,137,138]. This is not entirely surprising given that these viruses are spread by the same species of mosquitoes. Additionally, other infectious etiologies may also present with similar clinical syndrome including parvovirus infection, rubella, measles, leptospirosis, malaria and rickettsiosis [139].
Hospitalization is rarely required for ZIKV infection [103, 140, 141]. The case fatality rate of ZIKV is considered low and probably associated with comorbidities in such cases [142]. Infants and children present with similar disease as adults and recovery with no sequelae noted in such cases [100, 140, 143, 144].
5.2.2.1 Complications of ZIKV Infection
Neurological complications have been implicated as untoward effects of ZIKV infection. Such neurological deficits have also been reported with other arboviral infections, albeit rarely [145,146,147]. Guillian-Barré syndrome has been reported as a rare complication of ZIKV infection, although the true extent of the association and occurrence remain to be determined [103, 141, 148]. In addition, rare cases of brain ischemia, encephalitis and myelitis have been reported following ZIKV infection [149,150,151,152].
A place and time association was noted with the outbreak of ZIKV in Brazil and concomitant rise in number of babies born with microcephaly in 2015 [153], but studies have subsequently reported significant evidence to support this hypothesis [154]. As such, current opinion is that ZIKV infection during pregnancy can be linked to microcephaly and other congenital neurological and developmental abnormalities, although Koch’s postulates have not been applied to prove causality [155]. Reports of neonates with microcephaly and other malformations and abnormalities are accumulating since early 2016 [125, 130, 131, 156,157,158]. In conjunction with microcephaly, small brain size, ventriculomegaly, hypoplasia or agyria, agenesis of the cerebellar vermis, posterior fossa abnormalities and calcifications have been reported [125, 131, 156, 157]. Other abnormalities have included growth retardation, arthogryposis and ophthalmologic findings [125, 130,131,132, 156, 157, 159]. Fetal losses have also been reported, and a perinatal mortality rate of almost 27% was reported by Oliveira and co-workers [130, 131] in a small cohort study conducted in Brazil. Continued longitudinal monitoring of the development of the birth cohort affected by the ZIKV outbreak will reveal the breadth of neurological damage possibly caused by the virus [160]. A retrospective study has indicated cases of microcephaly and other abnormalities in babies born during the ZIKV outbreak in French Polynesia [161]. The possible link between these cases and ZIKV infection was not made at the time, most likely due to the limited number of cases involved (i.e. the extent of the outbreak in Brazil and South America allowed for the possible correlation to be made).
The risk of the development of fetal abnormalities during pregnancy remains to be fully elucidated. The risk factors and the risk associated with infection at different stages of gestation are not clear yet [162]. It is suggested that infection during the first trimester is the most damaging, although infection at later stages of gestation have also reportedly resulted in malformations and neurodevopmental problems [162].
5.2.3 Laboratory Diagnosis of ZIKV
Specialized laboratory testing is required for confirmation of a ZIKV diagnosis. In some settings this service is provided by national reference laboratories, but with the extent of the problem in Latin America the growing availability of commercially available reagents, these tests are offered by an increasing number of laboratories. Testing is recommended for symptomatic individuals with possible exposure to the virus [163]. Asymptomatic pregnant woman at risk of infection should also be screened for possible infection [163].
It is recommended that laboratory tests for ZIKV infection include RT-PCR detection of the viral RNA in whole blood, serum, plasma or urine which are collected during the acute phase of illness (i.e. <7 days after onset of illness) [163, 164]. The virus has also been detected in saliva, cerebrospinal fluid, female genital tract secretions, semen and breast milk [122, 128, 129, 161, 165,166,167,168,169]. Detection of viral RNA in secretions such as semen and saliva has been noted for extended periods even after viremia in the blood has been cleared [122, 129, 168, 170]. Although viremia in the blood is typically cleared quickly, viral RNA has been detected in blood more than 2 months after onset of illness in a limited number of cases [126, 171].
Detection of ZIKV-specific IgM responses requires verification with plaque reduction assays in order to determine the specificity of such responses and mitigate the risk of erroneous diagnosis due to the high level of cross reactivity expected for the antibody responses to other flaviviruses or flavivirus vaccines [163].
Fetal infection has been confirmed by RT-PCR on amniotic fluid, placenta and fetal serum, cerebrospinal fluid and brain [125, 130, 131, 156, 157]. Immunohistochemistry and electron microscopy of brain tissue has also been reported.
5.2.4 Treatment and Prevention of ZIKV
No specific treatment is yet available for ZIKV infection. Treatment is supportive and constitutes bed rest, oral hydration, antipyretics and pain medication [164]. Aspirin should not be used to manage pain and fever in children under the age of 12 due to the risk of Reye’s syndrome. Pregnant woman, symptomatic or asymptomatic, that may have had exposure to the virus should be screened for the infection [163]. Fetal monitoring including amniocentesis after 21 weeks of gestation and 6 weeks after exposure for microcephaly and other malformations is recommended [149, 164, 172].
No vaccines are currently available for ZIKV infection but current progress is encouraging [173]. Various approaches to the development of such a vaccine are currently underway, with more than 15 such projects initiated by June 2016 [174]. Prevention of infection in the absence of vaccination relies on preventing exposure to the mosquitos that may transmit the ZIKV. This may be achieved by for example applying insect repellents and staying indoors behind screened windows during peak mosquito activity. Many countries have issued travel warnings to pregnant woman, woman planning to become pregnant and their partners not to travel to ZIKV affected areas. Affected countries have advised woman to delay pregnancy at the time of the ZIKV outbreak, which is a difficult approach in countries where up to half of pregnancies are unplanned [175, 176].
5.3 Rabies
Rabies is the most fatal viral infection in recorded history, and although controllable in certain animal populations through vaccine programmes and largely preventable in humans through prevention of exposures and post exposure prophylaxis, clinical rabies disease cannot be treated [177,178,179]. Hampson et al. [180] estimated that 59,000 human cases of rabies occur in dog rabies affected countries annually. Dog rabies is most commonly reported from developing countries and typically affects poor communities where dog rabies control measures are inadequate. In addition, many epidemiological reports have indicated that children are particularly affected [181,182,183,184]. Human cases are underreported in many developing countries due to the lack of specialized diagnostic services to investigate such cases, but also due to the complexities of clinical diagnosis. Consequently, rabies remains an under-recognized and neglected disease in much of the world [180, 185].
The disease is marked by a progressive acute phase culminating in coma and followed by death within a short period in nearly all patients [186, 187]. The disease is caused by viruses belonging to the genus Lyssavirus of the family Rhabdoviridae. The lyssaviruses represent a diverse group of viruses with the International Committee on the Taxonomy of Viruses recognizing rabies lyssavirus and 13 rabies-related viral species in 2016 [188]. Additional lyssaviruses have been described but not classified taxonomically [189]. Not all of the lyssaviruses have been associated with human cases, and by far the public health burden associated with rabies relates to infection with “classic” rabies viruses (previously denoted as genotype 1 viruses) (RABV) [180, 190]. The RABV circulates in diverse terrestrial mammals which vary by geographical location [185]. The public health burden associated with rabies however relates to rabies in domestic dogs since these animals serve as the most common vector of the disease to the human population [180, 185, 191, 192]. Therefore, most human rabies cases are reported from developing countries where dog rabies control efforts are suboptimal [180, 185].
5.3.1 Epidemiological Aspects
The occurrence of lyssaviruses has been reported virtually globally, with the exception of the poles and some islands [193]. Only one of the currently described lyssaviruses, namely the Mokola virus, has not been associated with a bat reservoir [193, 194]. Nonetheless, only single human cases of rabies have been associated with bat exposures related to European bat lyssavirus 1 and 2; Australian bat virus; Duvenhage virus and Irkut virus [190, 195]. No human cases have been associated with Aravan, Bokeloh bat; Ikoma; Khujand, Shimoni bat, West Caucasian bat lyssavirus or the unclassified Lleida Bat virus to date [196].
Uniquely, rabies virus is associated with insectivorous bat reservoirs in the Americas—this phenomenon has not been reported elsewhere [197,198,199]. In addition to bats, cycles of rabies are also reported in various terrestrial mammals in the Americas, for example in raccoons and skunks in the USA. Domestic dog rabies is reported mostly from developing countries in Asia and Africa [180], with elimination achieved in the US and various European countries. The role of wildlife rabies varies from region to region. It should however be noted that all mammalian species are susceptible to rabies and may serve as potential vectors of the disease and this should be considered when evaluating possible exposure.
5.3.2 Clinical Aspects
The virus is transmitted in the saliva of an infected animal. Bites, but any small nicks or scrapes or scratches that break the skin, may constitute exposures. Mucosal exposures, such as licking over the face with contact with the nose, eyes and mouth are also considered exposures. Incubation periods range from 4 days to several years and tend to be shortest with severe bites on the face, head and neck, especially in children [186, 187]. The average incubation period for the RABV is 20–90 days with rare cases reported with an extended incubation period [200, 201]. There are no diagnostic tests possible during this period to predict the likelihood of rabies disease following on a potential exposure. A wide range of non-specific prodromal features including fever, headache, myalgia, fatigue, and change in mood and itching at the initial rabies exposure site may be reported, and in the absence of a report of possible exposure to rabies the disease is difficult to diagnose clinically [186].
Human rabies can take two clinical forms [186, 187]:
-
The more common, furious or agitated rabies which is characterized by hydrophobia, aerophobia and periods of extreme excitement alternating with lucid intervals, features of autonomic system dysfunction and finally by unconsciousness and complete paralysis. Initially spasms affect mainly the inspiratory muscles. Autonomic nervous system problems are frequently reported
-
Dumb or paralytic rabies which affects the medulla, spinal cord and spinal nerves. Paralytic rabies is less common and more difficult to recognize as rabies. Neurological sign include quadriparesis which predominantly involves the proximal muscles, loss of reflexes and paralysis. Cranial nerve involvement may result in ptosis and external ophthalmoplegia. The course of the disease is less acute and even without intensive care patients may survive for up to 30 days before they succumb to bulbar and respiratory paralysis.
The fatal outcome of RABV infection is associated with a progressive encephalitis and eventual multi-organ failure [187, 202]. The differential diagnosis of rabies is broad. A detailed history of previous potential animal exposure is very important, but can also be inaccurate as animal contact may have been forgotten or unnoticed especially as often reported where bats have been involved in the exposures [203]. The differential diagnosis includes other viral causes of encephalitis and bacterial meningitis and cerebral malaria [182, 186]. Tetanus is important in the differential diagnosis and may also be linked to the same animal source, typically there is a short incubation period and the muscle rigidity is constant, without relaxation between spasms. Paralytic rabies can also be confused with poliomyelitis and Guillian-Barré syndrome [204, 205]. Drug intoxications, psychiatric disorders also form part of the differential diagnosis.
5.3.3 Laboratory Diagnosis
Specialized testing is required to confirm a clinical diagnosis of rabies. Ante-mortem demonstration of virus in saliva or nuchal skin biopsies may be helpful in some cases, but demonstration of virus using molecular or immunofluorescence techniques on post mortem brain tissue remains the gold standard. Most often these tests are provided only by national reference laboratories, but remain unavailable in many countries where human rabies cases still occur. Routine blood screens are not informative for rabies diagnosis and are expected to be within normal ranges [186]. Examination of cerebrospinal fluid may be unremarkable and is not specific. Magnetic-resonance imaging and computed topography may be useful for differential diagnosis, but no remarkable findings are expected for rabies [187].
Ante-mortem diagnosis of rabies can be confirmed through RT-PCR detection of viral RNA in saliva, nuchal biopsies and cerebrospinal fluid [8, 206, 207]. Detection of viral RNA in tears, urine and respiratory secretions has also been reported [208]. Serological investigations are not always useful to confirm a rabies diagnosis, but the detection of virus neutralizing antibodies in the serum of a previously unvaccinated person or in cerebrospinal fluid are considered confirmatory findings [8]. The gold standard for rabies confirmation in humans (and animals) remains examination of brain tissue post mortem by PCR or immunofluorescence [8, 206, 207].
Every attempt should be made to confirm the diagnosis of human rabies as this provides critical information regarding the burden of disease, failed prevention and guides and stimulates improved rabies control in animals.
5.3.4 Treatment and Prevention
Clinical rabies disease remains untreatable and is limited essentially to palliative care through pain relief and sedation [186, 187]. Provision of intravenous morphine and benzodiazepines has been recommended [8, 187]. If the diagnosis of rabies is confirmed emotional support of the patient and their families is important. Standard infection control precautions are applied in the management of a suspected rabies patient. Transmission of the virus from patient to health care workers or family members has not been previously documented [8, 209]. Rabies post exposure prophylaxis (see below) should be provided to individuals bitten by an infected patient or who experience a mucosal exposure to patient saliva [8, 209].
Survival in an unvaccinated patient with rabies has been reported following the experimental treatment of a teenager in the USA in 2004 [210]. The patient, an adolescent girl, was exposed to rabies virus through contact with a bat, and was treated through the induction of coma. Remarkably, the patient mounted a potent natural immune response to the infection, an observation not commonly noted in unvaccinated rabies patients [210]. The protocol has since been repeated in a number of patients with discouraging results [177, 178, 211, 212]. Effective therapeutic interventions still remain to be expounded [178].
As humans are mostly exposed to the RABV through contact with domestic dogs, the vaccination of dogs presents a crucial intervention for prevention of the disease in humans [213, 214]. The latter should be complimented by promotion of responsible animal ownership and bite prevention programmes. Ensuring the availability and accessibility of post-exposure prophylaxis (PEP) for potentially exposed humans is key in the prevention of human rabies. Rabies PEP is highly effective in preventing rabies in persons exposed to RABV provided timeous administration of biologicals and recommended regimens are followed [8]. True failures of PEP are very rare [215, 216]. Modern rabies vaccines are highly purified, cell-derived inactivated vaccines with agreeable safety profiles, very few adverse reactions and are highly immunogenic [8]. Wound cleaning and PEP, done as soon as possible after suspected contact with a rabid animal can prevent the onset of rabies in virtually 100% of exposures. Intensive wound cleaning is a critical, affordable and manageable component of rabies prevention especially in communities without access to rabies biological prevention and may play some role in some cases in preventing progression to rabies disease. Management of the wound includes cleaning with copious amounts of water (even for small wounds) and soap. The wound should be disinfected with 70% ethanol and iodine. Wound management should also include the use of antibiotics and provision of tetanus vaccination/booster vaccination as clinically required.
Rabies PEP should start as soon as possible following on an exposure to a suspected rabid animal. Even if there is a delay between exposure and visit to the healthcare facility, there is no cut off point after which it is too late to initiate rabies PEP. The decision to give PEP or not should also be made on the risk of RABV transmission, for example taking into account: the animal species, provoked versus unprovoked attack, animal behavior, animal health and category of exposure and history of rabies vaccination of the animal if possible and reliable. Vaccination is either through the intramuscular or intradermal route in accordance with WHO recommended regimens [8]. In wounds that drew any amount of blood (including small wounds such as scrapes that broke the skin) (also called category III exposures), rabies immunoglobulin (RIG) is essential. The latter provides passive immunity whilst immunity is mounted against the rabies vaccination. The use of RIG is crucial in prevention of rabies in category III exposures and failure to provide has culminated in prophylaxis failures [217]. Human or equine-derived rabies immunoglobulins are highly effective and generally safe to use [8]. It should be noted that the use of equine derived immunoglobulin should be used in facilities that are able to manage potential severe allergic reactions [8]. The RIG is infiltrated locally into wound site as much as possible. If injection locally into wound is painful, particularly in children; especially if the wound is on the head, face or neck, consider some sedation provided it can be done safely. The costs of RIG, and limited access and availability in many developing countries, limit the success of PEP in developing countries.
Pre-exposure vaccination is provided to individuals at high or continual risk of RABV exposure, such as veterinarians and laboratory workers [8]. Rabies vaccination is also provided to travellers visiting areas that are endemic for rabies and if their activities may put them at risk of potential exposure (for example only visiting hotel versus backpacking in the outdoors) [218,219,220]. Pre-exposure regimens using cell-derived vaccines either administered intradermally or intramascularly as three doses have been shown to induce good immune responses, which are long lasting and successfully boosted even after many years if there is specific exposure [8]. Pre-exposure vaccination obviates the need for post exposure rabies immunoglobulin, a generally scarce resource in many areas. The use of pre-exposure vaccines as part of the expanded program for immunization has been used in some areas with high exposure risks and shown to be immunogenic and safe, with persistence of rabies virus-neutralizing antibodies [221,222,223].
5.4 Conclusion
Emerging and vector-borne and neglected viral diseases pose a risk to communities particularly in resource poor settings. While adults are disproportionately affected by some of these as a result of occupational exposure, the burden of rabies and Zika infections is borne by children and the fetus respectively. Treatment options overall are very limited or not possible, so early identification of emergence and prevention of spread, are key strategies. The development of vaccines for a number of emerging diseases show promise but clinical trials are still needed. A “One Health” approach addressing environmental, animal and human aspects of emerging and zoonotic diseases are key in prevention, early detection and control.
References
Fhogartaigh CN, Aarons E. Viral haemorrhagic fever. Clin Med. 2015;15(1):61–6.
Fletcher TE, Brooks TJ, Beeching NJ. Ebola and other viral haemorrhagic fevers. BMJ. 2014;349:g5079.
Colebunders R, Van Esbroeck M, Moreau M, Borchert M. Imported viral haemorrhagic fever with a potential for person-to-person transmission: review and recommendations for initial management of a suspected case in Belgium. Acta Clin Belg. 2002;57(5):233–40.
Ftika L, Maltezou HC. Viral haemorrhagic fevers in healthcare settings. J Hosp Infect. 2013;83(3):185–92.
Iroezindu MO, Unigwe US, Okwara CC, et al. Lessons learnt from the management of a case of Lassa fever and follow-up of nosocomial primary contacts in Nigeria during Ebola virus disease outbreak in West Africa. Trop Med Intern Health. 2015;20(11):1424–30.
Moore LS, Moore M, Sriskandan S. Ebola and other viral haemorrhagic fevers: a local operational approach. Br J Med. 2014;75(9):515–22.
Roy KM, Ahmed S, Inkster T, et al. Managing the risk of viral haemorrhagic fever transmission in a non-high-level intensive care unit: experiences from a case of Crimean-Congo haemorrhagic fever in Scotland. J Hosp Infect. 2016;93(3):304–8.
Vaccines and vaccination against yellow fever. WHO position paper—June 2013. Wkly Epidemiol Rec 2013;88(27):269–83.
Asogun AD, Ochei O, Moody V, et al. Clinical presentation and outcome of ribavirin treated RT-PCR confirmed Lassa fever patients in ISTH Irrua: a pilot study. Res Health Sci. 2016;1(2):68–77.
Hartnett JN, Boisen ML, Oottamasathien D, et al. Current and emerging strategies for the diagnosis, prevention and treatment of Lassa fever. Future Virol. 2015;10(5):559–84.
Ozbey SB, Kader Ç, Erbay A, Ergönül Ö. Early use of ribavirin is beneficial in Crimean-Congo hemorrhagic fever. Vect Zoonotic Dis. 2014;14(4):300–2.
World Health Organization. Clinical management of patients with viral haemorrhagic fever: a pocket guide for front-line health workers: interim emergency guidance for country adaptation. Geneva: WHO; 2016.
Uyar Y, Christova I, Papa A. Current situation of Crimean Congo hemorrhagic fever (CCHF) in Anatolia and Balkan Peninsula. Tűrk Higj Den Biyol Derg. 2011;68(3):139–51.
Ergönül Ö. Crimean–Congo hemorrhagic fever virus: new outbreaks, new discoveries. Curr Opin Virol. 2012;2(2):215–20.
Bente DA, Forrester NL, Watts DM, et al. Crimean-Congo hemorrhagic fever: history, epidemiology, pathogenesis, clinical syndrome and genetic diversity. Antiviral Res. 2013;100(1):159–89.
Mardani M, Pourkaveh B. Crimean-Congo hemorrhagic fever. Arch Clin Infect Dis. 2013;7(1):36–42.
Elaldi N, Kaya S. Crimean-Congo hemorrhagic fever. J Microbiol Infect Dis. 2014;4(5):s1–9.
Messina JP, Pigott DM, Duda KA, et al. A global compendium of human Crimean-Congo haemorrhagic fever virus occurrence. Sci Data. 2015;2:150016.
Shayan S, Bokaean M, Shahrivar MR, Chinikar S. Crimean-Congo Hemorrhagic Fever. Lab Med. 2015;46(3):180–9.
Leblebicioglu H, Ozaras R, Fletcher TE, Beeching NJ. Crimean-Congo haemorrhagic fever in travellers: a systematic review. Travel Med Infect Dis. 2016;14(2):73–80.
Brauburger K, Hume AJ, Mühlberger E, Olejnik J. Forty-five years of Marburg virus research. Viruses. 2012;4(10):1878–927.
Olival KJ, Hayman DT. Filoviruses in bats: current knowledge and future directions. Viruses. 2014;6(4):1759–88.
Brainard J, Hooper L, Pond K, Edmunds K, Hunter PR. Risk factors for transmission of Ebola or Marburg virus disease: a systematic review and meta-analysis. Int J Epidemiol. 2015.
Rougeron V, Feldmann H, Grard G, et al. Ebola and Marburg haemorrhagic fever. J Clin Virol. 2015;64:111–9.
Richmond JK, Baglole DJ. Clinical review. Lassa fever: epidemiology, clinical features and social consequences. BMJ. 2003;327:1271.
Ogbu O, Ajuluckuwu E, Uneke CJ. Lassa fever in West African sub-region. An overview. J Vect Borne Dis. 2007;44(1):1–11.
Gardner CL, Ryman KD. Yellow fever: a reemerging threat. Clin Lab Med. 2010;30:237–60.
Garske T, Van Kerkhove MD, Yactayo S, et al. Yellow Fever in Africa: estimating the burden of disease and impact of mass vaccination from outbreak and serological data. PLoS Med. 2014;11:e1001638.
Weyer J, Grobbelaar A, Blumberg L. Ebola virus disease: history, epidemiology and outbreaks. Curr Infect Dis Rep. 2015;17(5):1–8.
Centers for Disease Control and Prevention (2016) Outbreak chronology: Ebola virus disease. http://wwwcdcgov/vhf/ebola/outbreaks/history/chronologyhtml . Accessed 16 Sept 2016
Centers for Disease Control and Prevention. Question and answers: Zika virus infection (Zika) and pregnancy. http://www.cdc.gov/zika/pregnancy/question¬answers.html . Accessed 5 Feb 2016
Scott FD. Ebola haemorrhagic fever: why were children spared? Paediatr Infect Dis J. 1996;15:189–91.
Mupere E, Kaducu OF, Yoti Z. Ebola haemorraghic fever among hospitalized children and adolescents in northern Uganda: epidemiologic and clinical observations. Afr Health Sci. 2001;1(2):60–5.
World Health Organization Ebola Response Team. Ebola virus disease among children in West Africa. N Engl J Med. 2015;372:1274–7.
Baize S, Pannetier D, Oestereich L, et al. Emergency of Zaire Ebola virus disease in Guinea—preliminary report. N Engl J Med. 2014;371(15):1418–28.
Saéz M, Weiss S, Nowak K, et al. Investigating the zoonotic origin of the West Africa Ebola epidemic. EMBO Mol Med. 2014;7(1):17–23.
Leendertz SAJ, Gogarten JF, Düx A, et al. Assessing the evidence supporting fruit bats as the primary reservoirs for Ebola viruses. Ecohealth. 2016;13(1):18–25.
Leroy EM, Kumulungui B, Pourrut X, et al. Fruit bats as reservoirs of Ebola virus. Nature. 2007;438:575–6.
Pourrut X, Délicate A, Rollin P, et al. Spatial and temporal patterns of Zaire ebolavirus antibody prevalence in the possible reservoir bat species. J Infect Dis. 2007;196(2):S176.
Mann E, Streng S, Bergeron J, Kircher A. A review of the role of food and the food system in the transmission and spread of Ebola virus. PLoS Negl Trop Dis. 2015;9(12):e0004160.
Pourrut X, Kumulungui B, Wittmann T, et al. The natural history of Ebola virus in Africa. Microbes Infect. 2005;7:1005–14.
Formenty P. Ebola virus disease. In: Ergönül O, Can F, Akova M, Madoff L, editors. Emerging infectious diseases, clinical case studies. London: Academic; 2014. p. 121–34.
Goba A, Khan SH, Fonnie M, et al. An outbreak of Ebola virus disease in the Lassa fever zone. J Infect Dis. 2016.
Martines RB, Ng DL, Greer PW, et al. Tissue and cellular tropism, pathology and pathogenesis of Ebola and Marburg viruses. J Pathol. 2015;235(2):153–74.
O’Shea MK, Clay KA, Craig DG, et al. Diagnosis of febrile illnesses other than Ebola virus disease at an Ebola treatment unit in Sierra Leone. Clin Infect Dis. 2015;61(5):795–8.
Ansumana R, Jacobsen KH, Idris MB, et al. Ebola in Freetown area, Sierra Leone - a case study of 581 patients. N Engl J Med. 2015;372(6):587–8.
Barry M, Traoré FA, Sako FB, et al. Ebola outbreak in Conakry, Guinea: epidemiological, clinical, and outcome features. Med Mal Infect. 2014;44(11):491–4.
Chertow DS, Kleine C, Edwards JK, et al. Ebola virus disease in West Africa - clinical manifestations and management. N Engl J Med. 2014;371(22):2054–7.
Ansari AA. Clinical features and pathobiology of Ebolavirus infection. J Autoimmun. 2014;55:1–9.
Bwaka MA, Bonnet MJ, Calain P, et al. Ebola hemorrhagic fever in Kikwit, Democratic Republic of the Congo: clinical observations in 103 patients. J Infect Dis. 1999;179(Suppl 1):S1–7.
Olupot-Olupot P. Ebola in children: Epidemiology, clinical features, diagnosis and outcomes. Pediatr Infect Dis J. 2015;34(3):314–6.
Bebell LM, Riley LE. Ebola virus disease and Marburg disease in pregnancy: a review and management considerations for filovirus infection. Obstet Gynecol. 2015;125(6):1293–8.
Baggi F, Taybi A, Kurth A, et al. Management of pregnant women infected with Ebola virus in a treatment centre in Guinea, June 2014. Eurosurveillance. 2014;19(49):2–5.
Broadhurst MJ, Brooks TJ, Pollock NR. Diagnosis of Ebola virus disease: past, present, and future. Clin Microbiol Rev. 2016;29(4):773–93.
Chua AC, Cunningham J, Moussy F, et al. The case for improved diagnostic tools to control Ebola virus disease in West Africa and how to get there. PLoS Negl Trop Dis. 2015;9(6):e0003734.
Martin P, Laupland KB, Frost EH, Valiquette L. Laboratory diagnosis of Ebola virus disease. Intensive Care Med. 2015;41(5):895–8.
Nouvellet P, Garske T, Mills HL, et al. The role of rapid diagnostics in managing Ebola epidemics. Nature. 2015;528(7580):S109–16.
Ahrberg CD, Manz A, Neužil P. Palm-sized device for point-of-care Ebola detection. Anal Chem. 2016;88(9):4803–7.
Broadhurst MJ, Kelly JD, Miller A, et al. ReEBOV Antigen Rapid Test kit for point-of-care and laboratory-based testing for Ebola virus disease: a field validation study. Lancet. 2015;386(9996):867–74.
Kurosaki Y, Magassouba NF, Oloniniyi OK, et al. Development and evaluation of reverse transcription-loop-mediated isothermal amplification (RT-LAMP) assay coupled with a portable device for rapid diagnosis of Ebola virus disease in Guinea. PLoS Negl Trop Dis. 2016;10(2):e0004472.
Semper AE, Broadhurst MJ, Richards J, et al. Performance of the GeneXpert Ebola Assay for diagnosis of Ebola virus disease in Sierra Leone: a field evaluation study. PLoS Med. 2016;13(3):e1001980.
Walker NF, Brown CS, Youkee D, et al. Evaluation of a point-of-care blood test for identification of Ebola virus disease at Ebola holding units, Western Area, Sierra Leone, January to February 2015. Euro Surveill. 2015;20(12):64.
Weller SA, Bailey D, Matthews S, et al. Evaluation of the Biofire FilmArray BioThreat-E Test (v2. 5) for rapid identification of Ebola virus disease in heat-treated blood samples obtained in Sierra Leone and the United Kingdom. J Clin Microbiol. 2016;54(1):114–9.
Geisbert TW. Emergency treatment for exposure to Ebola virus: the need to fast-track promising vaccines. JAMA. 2015;313(12):1221–2.
Kilgore PE, Grabenstein JD, Salim AM, Rybak M. Treatment of Ebola virus disease. Pharmacotherapy. 2015;35(1):43–53.
Li H, Ying T, Yu F, et al. Development of therapeutics for treatment of Ebola virus infection. Microbes Infect. 2015;17(2):109–17.
Palich R, Gala JL, Petitjean F, et al. A 6-year-old child with severe Ebola virus disease: laboratory-guided clinical care in an Ebola Treatment Center in Guinea. PLoS Negl Trop Dis. 2016;10(3):e0004393.
http://apps.who.int/medicinedocs/documents/s22501en/s22501en.pdf. Accessed 6 Oct 2016
Bausch DG. Assessment of the risk of Ebola virus transmission from bodily fluids and fomites. J Infect Dis. 2007;196:S142–7.
Kudoyarova-Zubavichene NM, Sergeyev NN, Chepurnov AA, Netesov SV. Preparation and use of hyperimmune serum for prophylaxis and therapy of Ebola virus infections. J Infect Dis. 1999;179(1):S218–23.
Maruyama T, Rodriguez LL, Jahrling PB, et al. Ebola virus can be effectively neutralized by antibody produced in natural human infection. J Virol. 1999;73(7):6024–30.
Mupapa K, Massamba M, Kibadi K, et al. Treatment of Ebola hemorrhagic fever with blood transfusions from convalescent patients. J Infect Dis. 1999;179(1):S18–23.
Gulland A. First Ebola treatment is approved by WHO. BMJ. 2014;349:g5539.
Van Griensven J, De Weiggheleire A, Delamou A, et al. The use of Ebola convalescent plasma to treat Ebola virus disease in resource constrained settings: a perspective from the field. Clin Infect Dis. 2015.
Bouazza N, Treluyer JM, Foissac F, et al. Favipiravir for children with Ebola. Lancet. 2015;385(9968):603–4.
Bishop BM. Potential and emerging treatment options for Ebola virus disease. Ann Pharmacother. 2014;49(2):196–206.
Madelain V, Nguyen THT, Olivo A, et al. Ebola virus infection: review of the pharmacokinetic and pharmacodynamic properties of drugs considered for testing in human efficacy trials. Clin Pharmacokinet. 2016;55(8):907–23.
Sivanandy P, Sin SH, Ching OY, et al. A review on current trends in the management of Ebola virus disease. Int J Pharm Teaching Pract. 2016;7(1):2657–65.
Henao-Restrepo AM, Longini IM, Egger M, et al. Efficacy and effectiveness of an rVSV-vectored vaccine expressing Ebola surface glycoprotein: interim results from the Guinea ring vaccination cluster-randomised trial. Lancet. 2015;386(9996):857–66.
Gubler DJ. Human arbovirus infections worldwide. Ann N Y Acad Sci. 2001;951(1):13–24.
Alatoom A, Payne D. An overview of arboviruses and bunyaviruses. Lab Med. 2009;40(4):237–40.
Hayes EB, Sejvar JJ, Zaki SR, et al. Virology, pathology, and clinical manifestations of West Nile virus disease. Emerg Infect Dis. 2005;11(8):1174–9.
Gubler DJ. The global emergence/resurgence of arboviral diseases as public health problems. Arch Med Res. 2002;33(4):330–42.
Weaver SC, Barrett AD. Transmission cycles, host range, evolution and emergence of arboviral disease. Nat Rev Microbiol. 2004;2(10):789–801.
Garmendia AE, Van Kruiningen HJ, French RA. The West Nile virus: its recent emergence in North America. Microbes Infect. 2001;3(3):223–9.
Nash D, Mostashari F, Fine A, et al. The outbreak of West Nile virus infection in the New York City area in 1999. N Engl J Med. 2001;344(24):1807–14.
Messina JP, Brady OJ, Scott TW, et al. Global spread of dengue virus types: mapping the 70 year history. Trends Microbiol. 2014;22(3):138–46.
Weaver SC. Arrival of chikungunya virus in the new world: prospects for spread and impact on public health. PLoS Negl Trop Dis. 2014;8(6):e2921.
Fauci AS, Morens DM. Zika virus in the Americas—yet another arbovirus threat. N Engl J Med. 2016;374(7):601–4.
Moulin E, Selby K, Cherpillod P, Kaiser L, Boillat-Bianco N. Simultaneous outbreaks of dengue, chikungunya and Zika virus infections: diagnosis challenge in a returning traveller with nonspecific febrile illness. New Microbes New Infect. 2016;11:6–7.
Gulland A. Zika virus is a global public health emergency, declares WHO. BMJ. 2016;352:i657.
Heymann DL, Hodgson A, Freedman DO, et al. Zika virus and microcephaly: why is this situation a PHEIC? Lancet. 2016;387(10020):719–21.
Dick GWA, Kitchen SF, Haddow AJ. Zika virus (I). Isolations and serological specificity. Trans R Soc Trop Med Hyg. 1952;46(5):509–20.
Fagbami AH. Zika virus infections in Nigeria: virological and seroepidemiological investigations in Oyo State. J Hygiene. 1979;83(02):213–9.
Darwish MA, Hoogstraal H, Roberts TJ, et al. A sero-epidemiological survey for certain arboviruses (Togaviridae) in Pakistan. Trans R Soc Trop Med Hyg. 1983;77(4):442–5.
Haddow AJ, Williams MC, Woodall JP, et al. Twelve isolations of Zika virus from Aedes (Stegomyia) africanus (Theobald) taken in and above a Uganda forest. Bull World Health Organ. 1964;31(1):57.
Macnamara FN. Zika virus: a report on three cases of human infection during an epidemic of jaundice in Nigeria. Trans R Soc Trop Med Hyg. 1954;48(2):139–45.
Olson JG, Ksiazek TG. Zika virus, a cause of fever in Central Java, Indonesia. Trans R Soc Trop Med Hyg. 1981;75(3):389–93.
Simpson DIH. Zika virus infection in man. Trans R Soc Trop Med Hyg. 1964;58(4):335–8.
Duffy MR, Chen TH, Hancock WT, et al. Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med. 2009;360:2536.
Hayes EB. Zika virus outside Africa. Emerg Infect Dis. 2009;15:1347.
Lanciotti RS, Kosoy OL, Laven JJ, et al. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis. 2008;14:1232.
Cao-Lormeau V-M, Blake A, Mons S, et al. Guillain-Barré Syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. Lancet. 2016;387(10027):1531–9.
Musso D, Nilles EJ, Cao-Lormeau V-M. Rapid spread of emerging Zika virus in the Pacific area. Clin Microbiol Infect. 2014;20(10):O595–6.
Musso D, Nhan T, Robin E, et al. Potential for Zika virus transmission through blood transfusion demonstrated during an outbreak in French Polynesia, November 2013 to February 2014. Euro Surveill. 2014;19(14):20761.
Cao-Lormeau V-M, Roche C, et al. Zika virus: French Polynesia, South Pacific, 2013. EID. 2014;20(6):1085–6.
Tognarelli J, Ulloa S, Villagra E, Lagos J, Aguayo C, Fasce R, Parra B, Mora J, Becerra N, Lagos N, Vera L. A report on the outbreak of Zika virus on Easter Island, South Pacific, 2014. Arch Virol. 2016;161(3):665–8.
Campos GS, Bandeira AC, Sardi SI. Zika virus outbreak, Bahia, Brazil. Emerg Infect Dis. 2015;21(10):1885.
Faria NR, Azevedo Rdo S, Kraemer MU, et al. Zika virus in the Americas: early epidemiological and genetic findings. Science. 2016;352:345.
Zanluca C, Melo VCAD, Mosimann ALP, Santos GIVD, Santos CNDD, Luz K. First report of autochthonous transmission of Zika virus in Brazil. Mem Inst Oswaldo Cruz. 2015;110(4):569–72.
World Health Organization (2016). Zika virus. Microcephaly Guillian-Barré syndrome situation report 29 September 2016. http://apps.who.int/iris/bitstream/10665/250244/1/zikasitrep29Sep16-eng.pdf?ua=1. Accessed 6 Oct 2016.
Gubler D, Kuno G, Markoff L. Flaviviruses. In: Knipe DM, Howley PM, editors. Fields virology. Philadelphia: Lippincott, Williams and Wilkins; 2007. p. 1153–252.
Chouin-Carneiro T, Vega-Rua A, Vazeille M, et al. Differential susceptibilities of Aedes aegypti and Aedes albopictus from the Americas to Zika Virus. PLoS Negl Trop Dis. 2016;10(3):e0004543.
Diagne CT, Diallo D, Faye O, et al. Potential of selected Senegalese Aedes spp. mosquitoes (Diptera: Culicidae) to transmit Zika virus. BMC Infect Dis. 2015;15(1):1.
Diallo D, Sall AA, Diagne CT, et al. Zika virus emergence in mosquitoes in southeastern Senegal, 2011. PLoS One. 2014;9(10):e109442.
Faye O, Faye O, Diallo D, et al. Quantitative real-time PCR detection of Zika virus and evaluation with field-caught mosquitoes. Virol J. 2013;10(1):1.
Grard G, Caron M, Mombo IM, et al. Zika virus in Gabon (Central Africa) - 2007: a new threat from Aedes albopictus? PLoS Negl Trop Dis. 2014;8(2):e2681.
Ledermann JP, Guillaumot L, Yug L, et al. Aedes hensilli as a potential vector of Chikungunya and Zika viruses. PLoS Negl Trop Dis. 2014;8(10):e3188.
Li MI, Wong PSJ, Ng LC, Tan CH. Oral susceptibility of Singapore Aedes (Stegomyia) aegypti (Linnaeus) to Zika virus. PLoS Negl Trop Dis. 2012;6(8):e1792.
Marcondes CB, Ximenes MDFFD. Zika virus in Brazil and the danger of infestation by Aedes (Stegomyia) mosquitoes. Rev Soc Bras Med Trop. 2016;49(1):4–10.
Wong PSJ, Li MZI, Chong CS, et al. Aedes (Stegomyia) albopictus (Skuse): a potential vector of Zika virus in Singapore. PLoS Negl Trop Dis. 2013;7(8):e2348.
Atkinson B, Hearn P, Afrough B, et al. Detection of Zika virus in semen. Emerg Infect Dis. 2016;22(5):940.
Besnard M, Lastere S, Teissier A, Cao-Lormeau VM, Musso D. Evidence of perinatal transmission of Zika virus, French Polynesia, December 2013 and February 2014. Euro Surveill. 2014;19(13):20751.
Brooks JT. Update: interim guidance for prevention of sexual transmission of Zika virus - United States, July 2016. MMWR Morb Mortal Wkly Rep. 2016;65:120–1.
Calvet G, Aguiar RS, Melo AS, Sampaio SA, de Filippis I, Fabri A, Araujo ES, de Sequeira PC, de Mendonça MC, de Oliveira L, Tschoeke DA. Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: a case study. Lancet Infect Dis. 2016;16:653–60.
Driggers RW, Ho CY, Korhonen EM, et al. Zika virus infection with prolonged maternal viremia and fetal brain abnormalities. N Engl J Med. 2016;374(22):2142–51.
Foy BD, Kobylinski KC, Chilson Foy JL, Blitvich BJ, Travassos da Rosa A, Haddow AD, Lanciotti RS, Tesh RB. Probable non-vector-borne transmission of Zika virus, Colorado, USA. Emerg Infect Dis. 2011;17(5):880–2.
Musso D, Roche C, Nhan TX, et al. Detection of Zika virus in saliva. J Clin Virol. 2015;68:53–5.
Musso D, Roche C, Robin E, et al. Potential sexual transmission of Zika virus. Emerg Infect Dis. 2015;21(2):359–61.
Oliveira MAS, Aguiar RS, Ramos Amorim MR, et al. Congenital zika virus infection: beyond neonatal microcephaly. JAMA Neurol. 2016.
Oliveira MAS, Malinger G, Ximenes R, et al. Zika virus intrauterine infection causes fetal brain abnormality and microcephaly: tip of the iceberg? Ultrasound Obstet Gynecol. 2016;47(1):6–7.
Sarno M, Sacramento GA, Khouri R, do Rosário MS, Costa F, Archanjo G, Santos LA, Nery Jr N, Vasilakis N, Ko AI, de Almeida AR. Zika virus infection and stillbirths: a case of hydrops fetalis, hydranencephaly and fetal demise. PLoS Negl Trop Dis. 2016;10(2):e0004517.
Venturi G, Zammarchi L, Fortuna C, Remoli ME, Benedetti E, Fiorentini C, Trotta M, Rizzo C, Mantella A, Rezza G, Bartoloni A. An autochthonous case of Zika due to possible sexual transmission, Florence, Italy, 2014. Euro Surveill. 2016;21(8):30148.
Filipe AR, Martins CMV, Rocha H. Laboratory infection with Zika virus after vaccination against yellow fever. Arch Gesamte Virusforsch. 1973;43(4):315–9.
Brasil P, Calvet GA, Siqueira AM, Wakimoto M, de Sequeira PC, Nobre A, Quintana MDSB, de Mendonça MCL, Lupi O, de Souza RV, Romero C. Zika virus outbreak in Rio de Janeiro, Brazil: clinical characterization, epidemiological and virological aspects. PLoS Negl Trop Dis. 2016;10(4):e0004636.
Dupont-Rouzeyrol M, O’Connor O, Calvez E, et al. Co-infection with Zika and dengue viruses in 2 patients, New Caledonia, 2014. Emerg Infect Dis. 2015;21(2):381–2.
Roth A, Mercier A, Lepers C, et al. Concurrent outbreaks of dengue, chikungunya and Zika virus infections-an unprecedented epidemic wave of mosquito-borne viruses in the Pacific 2012-2014. Euro Surveill. 2014;19(41):20929.
Villamil-Gómez WE, González-Camargo O, Rodriguez-Ayubi J, et al. Dengue, chikungunya and Zika co-infection in a patient from Colombia. J Infect Public Health. 2016;9(5):684–6.
LaBeaud AD (2016) Zika virus infection: an overview. In: Hirsch MS, Baron EL, editors. UptoDate.com Wolters Kluwer. Topic 106169, Version 93.0.
Goodman AB, Dziuban EJ, Powell K, et al. Characteristic of children age < 18 years with zika virus disease acquired postnatally—US States, January 2015-July 2016. MMWR Morb Mortal Wkly Rep. 2016;65:1082–5.
Oehler E, Watrin L, Larre P, et al. Zika virus infection complicated by Guillain-Barre syndrome—case report, French Polynesia, December 2013. Euro Surveill. 2014;19(9):20720.
Sarmiento-Ospina A, Vásquez-Serna H, Jimenez-Canizales CE, et al. Zika virus associated deaths in Colombia. Lancet Infect Dis. 2016;16(5):523–4.
Fleming-Dutra KE, Nelson JM, Fischer M, et al. Update: Interim guidelines for Health Care Providers caring for infants and children with possible Zika Virus infection United States. MMWR Morb Mortal Wkly Rep. 2016;65(7):182–7.
Karwowski MP, Nelson JM, Staples JE, et al. Zika virus disease: A CDC update for pediatric health care providers. Paediatrics. 2016;137(5):e20160621.
Gérardin P, Sampéris S, Ramful D, et al. Neurocognitive outcome of children exposed to perinatal mother-to-child chikungunya virus infection: the CHIMERE cohort study on Reunion Island. PLoS Negl Trop Dis. 2014;8:e2996.
O’Leary DR, Kuhn S, Kniss KL, et al. Birth outcomes following West Nile virus infection of pregnant women in the United States: 2003-2004. Paediatrics. 2006;117:e537–45.
Sips GJ, Wilschut J, Smit JM. Neuroinvasive flavivirus infections. Rev Med Virol. 2011;22:69–87.
Smith DW, Mackenzie J. Zika virus and Guillain-Barré syndrome: another viral cause to add to the list. Lancet. 2016;387:1486–8.
Baud D, Van Mieghem T, Musso D, et al. Clinical management of pregnant women exposed to Zika virus. Lancet Infect Dis. 2016;16(5):523.
Carteaux G, Maquart M, Bedet A, et al. Zika virus associated with meningoencephalitis. N Engl J Med. 2016;374:1595–6.
Mécharles S, Herrmann C, Poullian P, et al. Acute myelitis due to Zika virus infection. Lancet. 2016;387:1481.
Rozé B, Najioullah F, Signate A et al (2016) Zika virus detection in cerebrospinal fluid from two patients with encephalopathy, Martinique, February 2016. Euro Surveill 21(16), pii: 30205.
Schuler-Faccini L, Ribeiro EM, IML F, et al. Possible association between Zika virus infection and microcephaly—Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(3):59–62.
Rodrigues LC. Microcephaly and Zika virus infection. Lancet. 2016;387(10033):2070–2.
Tetro JA. Zika and microcephaly: causation, correlation, or coincidence. Microbes Infect. 2016;18(3):167–8.
de Araújo TVB, Rodrigues LC, de Alencar Ximenes RA et al (2016). Association between Zika virus infection and microcephaly in Brazil, January to May, 2016: preliminary report of a case-control study. Lancet Infect Dis. http://dx.doi.org/10.1016/
Mlakar J, Korva M, Tul N, et al. Zika virus associated with microcephaly. N Engl J Med. 2016;374(10):951–8.
Rubin EJ, Greene MF, Baden LR. Zika virus and microcephaly. N Engl J Med. 2016;374(10):984–5.
Jampol LM, Goldstein DA. Zika virus infection and the eye. JAMA Ophthalmol. 2016;134(5):535–6.
Barton MA, Salvadori MI. Zika virus and microcephaly. Can Med Assoc J. 2016;188(7):E118–9.
Besnard M, Eyrolle-Guignot D, Guillemette-Artur P, et al. Congenital cerebral malformations and dysfunction in fetuses and newborns following the 2013 to 2014 Zika virus epidemic in French Polynesia. Euro Surveill. 2016;21(13):30181.
Ticconi C, Pietropolli A, Rezza G. Zika virus infection and pregnancy: what we do and do not know. Pathog Glob Health. 2016.
World Health Organization (2016) Laboratory testing for Zika virus infection. Interim guidance. WHO/ZIKV/LAB/16.1. Available from: http://apps.who.int/iris/bitstream/10665/204671/1/WHO_ZIKV_LAB_16.1_eng.pdf. Accessed on 20 Oct 2016.
Falcao MB, Cimerman S, Luz KG, et al. Management of infection by the Zika virus. Ann Clin Microbiol Antimicrob. 2016;15:57.
Barzon L, Pacenti M, Berto A, et al. Isolation of infectious Zika virus from saliva and prolonged viral RNA shedding in a traveller returning from the Dominican Republic to Italy, January 2016. Euro Surveill. 2016;21(10):Article 1.
Dupont-Rouzeyrol M, Biron A, O’Connor O, et al. Infectious Zika viral particles in breastmilk. Lancet. 2016;387(10023):1051.
Fréour T, Mirallié S, Hubert B, et al. Sexual transmission of Zika virus in an entirely asymptomatic couple returning from a Zika epidemic area, France, April 2016. Euro Surveill. 2016;21(23):30254.
Mansuy JM, Dutertre M, Mengelle C, et al. Zika virus: high infectious viral load in semen, a new sexually transmitted pathogen. Lancet Infect Dis. 2016;16(405):00138–9.
Prisant N, Bujan L, Benichou H, et al. Zika virus in the female genital tract. Lancet Infect Dis. 2016;16(9):1000–1.
Harrower J, Kiedrzynski T, Baker S, et al. Sexual transmission of Zika virus and persistence in semen, New Zealand, 2016. Emerg Infect Dis. 2016;22(10):1855–7.
Lustig Y, Mendelson E, Paran N, et al. Detecton of Zika virus RNA in whole blood in imported Zika virus disease cases up to 2 months after symptom onset, Israel, December 2015-April 2016. Euro Surveill. 2016;21(26):30269.
Vouga M, Musso D, Van Mieghem T, Baud D. CDC guidelines for pregnant woman during the Zika virus outbreak. Lancet. 2016;387:843–4.
Kennedy RB. Pushing forward with Zika vaccines. EBioMedicine. 2016.
Tripp RA, Ross TM. Development of a Zika vaccine. Expert Rev Vaccines. 2016;15(9):1083–5.
Ndeffo-Mbah ML, Parpia AS, Galvani AP. Mitigating prenatal zika virus infection in the America. Ann Intern Med. 2016;165:551–9.
Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. 2014;45:301–14.
Jackson AC. Therapy of human rabies. In: Jackson AC, editor. Advances in virus research: advances in rabies research. Boston: Academic; 2011. p. 365–75.
Jackson AC. Current and future approaches to the therapy of human rabies. Antiviral Res. 2013;99(1):61–7.
Warrell MJ, Warrell DA. Rabies: the clinical features, management and prevention of the classic zoonosis. Clin Med. 2015;15(1):78–81.
Hampson K, Coudeville L, Lembo T, et al. Estimating the global burden of endemic canine rabies. PLoS Negl Trop Diseases. 2015;9(4):e0003709.
Ichhpujani RL, Mala C, Veena M, et al. Epidemiology of animal bites and rabies cases in India. A multicentric study. J Commun Dis. 2008;40(1):27–36.
Mallewa M, Fooks AR, Banda D, et al. Rabies encephalitis in malaria-endemic area, Malawi, Africa. Emerg Infect Dis. 2007;13(1):136–9.
Sriaroon C, Sriaroon P, Daviratanasilpa S, et al. Retrospective: animal attacks and rabies exposures in Thai children. Travel Med Infect Dis. 2006;4(5):270–4.
Schalamon J, Ainoedhofer H, Singer G, et al. Analysis of dog bites in children who are younger than 17 years. Pediatrics. 2006;117(3):e374–9.
Taylor LH, Nel LH. Global epidemiology of canine rabies: past, present, and future prospects. Vet Med Res Rep. 2015;6:361–71.
Hemachudha T, Laothamatas J, Rupprecht CE. Human rabies: a disease of complex neuropathogenetic mechanisms and diagnostic challenges. Lancet Neurol. 2002;1(2):101–9.
Hemachudha T, Ugolini G, Wacharapluesadee S, et al. Human rabies: neuropathogenesis, diagnosis, and management. Lancet Neurol. 2013;12(5):498–513.
Afonso CL, Amarasinghe GK, Bányai K, et al. Taxonomy of the order Mononegavirales: update 2016. Arch Virol. 2016;161(8):1–10.
Ceballos NA, Morón SV, Berciano JM, et al. Novel lyssavirus in bat, Spain. Emerg Infect Dis. 2013;19(5):793–5.
Banyard AC, Evans JS, Luo T, Fooks AR. Lyssaviruses and bats: emergence and zoonotic threat. Viruses. 2014;6(8):2974–90.
Overall KL, Love M. Dog bites to humans-demography, epidemiology, injury and risk. J Am Vet Med Assoc. 2001;218(12):1923–34.
World Health Organisation. WHO Expert Consultation on Rabies. Second report. World Health Organization technical report series 982. Geneva: WHO; 2013.
Kuzmin IV, Rupprecht CE. Bat lyssaviruses. In: Wang L-F, Cowled C, editors. Bats and viruses: a new frontier of emerging infectious diseases. India: Wiley Blackwell; 2015. p. 47–97.
Kgaladi J, Wright N, Coertse J, et al. Diversity and epidemiology of Mokola virus. PLoS Negl Trop Dis. 2013;7(10):e2511.
Johnson N, Vos A, Freuling C, et al. Human rabies due to lyssavirus infection of bat origin. Vet Microbiol. 2010;142(3-4):151–9.
Kuzmin IV. Basic facts about Lyssaviruses. In: Rupprecht CE, Nagarajan T, editors. Current laboratory techiques in rabies diagnosis, research and prevention. New York: Elsevier; 2014. p. 3–24.
Davis AD, Gordy PA, Bowen RA. Unique characteristics of bat rabies viruses in big brown bats (Eptesicus fuscus). Arch Virol. 2013;158(4):809–20.
Johnson N, Aréchiga-Ceballos N, Aguilar-Setien A. Vampire bat rabies: ecology, epidemiology and control. Viruses. 2014;6(5):1911–28.
Patyk K, Turmelle A, Blanton JD, Rupprecht CE. Trends in national surveillance data for bat rabies in the United States: 2001–2009. Vector Borne Zoonotic Dis. 2012;12(8):666–73.
Grattan-Smith PJ, O’Regan WJ, Ellis PS, et al. Rabies. A second Australian case, with a long incubation period. Med J Aust. 1992;156(9):651–4.
Johnson N, Fooks A, McColl K. Reexamination of human rabies case with long incubation, Australia. Emerg Infect Dis. 2008;14(12):1950–2.
Fu ZF, Jackson AAC. Neuronal dysfunction and death in rabies virus infection. J Neurovirol. 2005;11(1):101–6.
Messenger SL, Smith JS, Rupprecht CE. Emerging epidemiology of bat-associated cryptic cases of rabies in humans in the United States. Clin Infect Dis. 2002;35(6):738–47.
Cohen R, Babushkin F, Shapiro M, et al. Paralytic rabies misdiagnosed as Guillain-Barre syndrome in a guest worker: a case report. J Neuroinfect Dis. 2016;7:208.
Sheikh KA, Ramos-Alvarez M, Jackson AC, et al. Overlap of pathology in paralytic rabies and axonal Guillain–Barré syndrome. Ann Neurol. 2005;57(5):768–72.
Fooks AR, Johnson N, Freuling CM, et al. Emerging technologies for the detection of rabies virus: challenges and hopes in the 21st century. PLoS Negl Trop Dis. 2009;3(9):e530.
Hanlon CA, Nadin-Davis SA. Laboratory diagnosis of rabies. In: Jackson A, editor. Rabies: scientific basis of the disease and its management. Third ed. Boston: Academic; 2013. p. 409–59.
Wacharapluesadee S, Hemachudha T. Urine samples for rabies RNA detection in the diagnosis of rabies in humans. Clin Infect Dis. 2002;34(6):874–5.
Stantic-Pavlinic M. Rabies treatment of health care staff. Swiss Med Wkly. 2002;132:129–31.
Willoughby RE, Tieves KS, Hoffman GM, et al. Survival after treatment of rabies with induction of coma. N Engl J Med. 2005;352(24):2508–14.
Hemachudha T, Sunsaneewitayakul B, Desudchit T, et al. Failure of therapeutic coma and ketamine for therapy of human rabies. J Neurovirol. 2006;12(5):407–9.
Wilde H, Hemachudha T, Jackson AC. Viewpoint: management of human rabies. Trans R Soc Trop Med Hyg. 2008;102(10):979–82.
Cleaveland S, Kaare M, Knobel D, Laurenson MK. Canine vaccination—providing broader benefits for disease control. Vet Microbiol. 2006;117(1):43–50.
Cleaveland S, Kaare M, Tiringa P, et al. A dog rabies vaccination campaign in rural Africa: impact on the incidence of dog rabies and human dog-bite injuries. Vaccine. 2003;21(17):1965–73.
Rupprecht CE, Gibbons RV. Prophylaxis against rabies. N Engl J Med. 2004;351(25):2626–35.
Wilde H. Failures of post-exposure rabies prophylaxis. Vaccine. 2007;25(44):7605–9.
Wilde H, Khawplod P, Hemachudha T, Sitprija V. Postexposure treatment of rabies infection: can it be done without immunoglobulin? Clin Infect Dis. 2002;34:477–80.
Christiansen AH, Rodriguez AB, Nielsen J, Cowan SA. Should travellers to rabies-endemic countries be pre-exposure vaccinated? An assessment of post-exposure prophylaxis and pre-exposure prophylaxis given to Danes travelling to rabies-endemic countries 2000–12. Journal of Travel Medicine. 2016;23(4):taw022.
LeGuerrier P, Pilon PA, Deshaies D, Allard R. Pre-exposure rabies prophylaxis for the international traveller: a decision analysis. Vaccine. 1996;14(2):167–76.
Pandey P, Shlim DR, Cave W, Springer MF. Risk of possible exposure to rabies among tourists and foreign residents in Nepal. J Travel Med. 2002;9(3):127–31.
Dodet B, Asian Rabies Expert Bureau (AREB). Report of the sixth AREB meeting, Manila, The Philippines, 10-12 November 2009. Vaccine. 2010;28(19):3265–8.
Kamoltham T, Thinyounyong W, Phongchamnaphai P, et al. Pre-exposure rabies vaccination using purified chick embryo cell rabies vaccine intradermally is immunogenic and safe. J Pediatr. 2007;151(2):173–7.
Malerczyk C, Vakil HB, Bender W. Rabies pre-exposure vaccination of children with purified chick embryo cell vaccine (PCECV). Hum Vaccin Immunother. 2013;9(7):1454–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Weyer, J., Blumberg, L.H. (2017). Emerging Zoonotic and Vector-Borne Viral Diseases. In: Green, R. (eds) Viral Infections in Children, Volume I. Springer, Cham. https://doi.org/10.1007/978-3-319-54033-7_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-54033-7_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-54032-0
Online ISBN: 978-3-319-54033-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)