Abstract
In the past, before 2016, brain tumors were classified into several types, and their respective grades based largely on histology. While this allowed for categorization of tumors, the grading did not always correlate with overall survival. At the same time, neuro-oncology research work demonstrated that tumoral molecular genetics allowed for a better correlation with overall survival. This led to the Revised 2016 WHO classification of brain tumors, which for the first time in neuro-pathology saw the incorporation of mutation profiles applied to classification of brain tumors. Continued development in the field of neuro-oncology meant better categorization of previously described tumors, and the description of newer tumors. This led to another update, the 2021 classification of brain tumors. This chapter provides an overview of these revised brain tumor classification systems, and discusses the imaging profiles of certain select yet important tumor types in detail.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Primary brain tumors
- WHO classification
- IDH
- 1p-19q codeletion
- TP53 mutation status in adults
- BRAF and H3K27 altered tumors in children
- Imaging features
- Prognosis
- Treatment strategies
-
To familiarize radiologists with the revised classification of CNS tumors in terms of certain important mutation profiles including IDH mutation, 1p/19q-codeletion status, TP53 mutation, BRAF mutation, and H3K27M-mutation, and their influence on improving diagnostic accuracy, treatment strategies, and overall survival.
-
To provide an overview of the imaging phenotypes for the different glioma genotypes.
1 Introduction
The World Health Organization (WHO) Classification of Tumors of central nervous system (CNS) provided an update in 2016 nearly 10 years after the 2007 version to help more systematically categorize brain tumors. The revised system for the first time uniquely included molecular and genetic parameters of the individual tumor types, in addition to the always incorporated histological features. Accordingly, each tumor is now identified by both its phenotype (based on histology) and genotype (based on its molecular and genetic parameters) [1]. Subsequently, another update was published in 2021 as the fifth edition of the WHO Classification of tumors of the central nervous system [2]. This focused on further advancing the role of molecular profiling in CNS tumor classification. Also, it emphasized the importance of integrated diagnosis and layered reports. New tumor types and subtypes have been introduced.
2 Goals of the Revised Classification
The goals are multi-fold:
-
1.
To resolve some of the confusion created by classifying brain tumors based only on histology
-
2.
Provide greater diagnostic accuracy.
-
3.
Aid better treatment strategies.
-
4.
Allow for an improved assessment of the prognosis based on the specific tumor type.
3 Background
A classic example of uncertainty created in the past where tumors were classified based only on histology included the group “oligoastrocytoma.” These were tumors which exhibited features of both oligodendroglioma and astrocytoma on histology and were therefore lumped together as oligoastrocytomas [3,4,5]. Accordingly, their management was not definitive which in turn influenced their prognosis. Categorizing this tumor group based on the underlying 1p/19q codeletion (genetic mutation) status, allows them to be clearly distinguished almost always into either (1p/19q-codeleted) oligodendroglioma or (1p-19q-intact) astrocytoma [6,7,8]. Only a few tumors cannot be categorized into either group and are known as oligoastrocytoma, NOS (not otherwise specified) [1, 2, 9,10,11]. This clear distinction allows more accurate diagnosis, which therefore influences more appropriate tumor specific treatment strategies, and a better sense for the overall prognosis. Another perplexing prognostic feature was noted in terms of the overall survival of certain grade 1 low grade gliomas, which surprisingly despite their lower grade performed much worse than grade 3 astrocytomas. This can now be explained based on their IDH mutation status, with IDH-wildtype grade 1 gliomas performing much poorer than IDH-mutant grade 3 astrocytomas [6, 7]. Thus, it is the mutation status which influences the overall prognosis much more than the histology.
Utilizing the background above, the discussion below will mention the salient features of how the revised WHO classification system better classifies infiltrating gliomas in adults, gliomas in children, and certain new tumor types. Please note that a description of all CNS tumor types included in the revised 2016 and 2021 classifications of CNS tumors is beyond the scope of this text.
4 Infiltrating Gliomas in Adults
Several mutations have been described associated with infiltrating gliomas in adults. Of these, some of the important ones include IDH mutation, 1p-19q codeletion, and TP53 mutation status [12].
The primary deterministic mutation includes the IDH mutation status—presence suggests IDH-mutant, and absent an IDH-wildtype tumor [12, 13].
5 IDH-Mutant Gliomas
There are 2 types of IDH mutation, IDH1 and IDH2 mutated tumors. Most tumors are IDH1 mutated. Hence when a tumor is considered as IDH-mutated, it is the IDH1 status which is considered. Less than 3% of IDH-mutated tumors and exclusively IDH2 mutant tumors [13, 14].
5.1 Clinical Relevance and Prognosis
IDH-mutant tumors are seen more commonly in the middle-aged population (30–60 years of age), than IDH-wildtype tumors which are more frequently seen in the older population (>60–65 years of age). The overall survival of IDH-mutant tumors is far better than IDH-wild type tumors. In fact, as mentioned previously low grade (grade 1 by histology), IDH-wild type gliomas have an overall survival close to that of grade 4 IDH-wildtype glioblastomas, but much worse than grade III IDH-mutant gliomas. It is the IDH mutation status which is the driving force in terms of overall prognosis, much more than the histological grade. Furthermore, even among the grade 4 glioblastomas, it has been noted that IDH-mutant glioblastomas have an overall survival much better than IDH-wildtype glioblastomas. Supporting this is the fact that most IDH-mutant glioblastomas are the secondary type, while most IDH-wildtype glioblastomas are the de novo or primary type [15].
It is a known fact in glioma surgery that the wider the resection the better is the overall survival. Knowing preoperatively that the tumor is an IDH-mutant type can influence the surgeon to go for a more complete surgical resection, including the FLAIR signal abnormality surrounding the enhancing mass, especially if the margins of the FLAIR signal abnormality extend into a non-eloquent region of the brain [16].
Key Points
-
IDH-mutant tumors, seen more commonly in the middle-aged population (third to sixth decade of life), have a far better overall survival than IDH-wildtype tumors, which are seen more commonly in the older patients (>60–65 years of age).
5.2 Radiological Features
Both IDH1 and IDH2 mutations change the role of IDH in the citric acid cycle. This results in accumulation of 2-HG within tumor cells. *2-Hydroxyglutarate (2-HG) can be detected on MR spectroscopy and is therefore considered to be the imaging hallmark of all IDH-mutant tumors [17]. However, reliable detection is challenging and is possible only at some select centers with special MR spectroscopists on site [17,18,19,20].
It has been noted that most IDH-mutated tumors occur in a single lobe, frontal lobe being the most common, followed by temporal, parietal, and occipital lobes [21]. Most such tumors demonstrate a sharp margin and inhomogeneous but mild contrast enhancement. In contrast, IDH-wildtype tumors are frequently multilobar in location, though involvement of only the temporal or frontal lobes is occasionally seen. Preferred site involves the insula with extension into the adjacent temporal, frontal, and parietal lobes [21, 22]. In terms of their morphological appearance, these IDH-wildtype tumors demonstrate ill-defined margins with the adjacent brain especially on FLAIR/T2WI. Necrosis and moderate-to-intense heterogeneous, especially peripheral enhancement are seen (Fig. 4.1). The presence of necrosis, more intense enhancement, and ill-defined margins suggests more oxygen demand, more robust neoangiogenesis, and infiltrative nature of the wildtype tumors than their IDH-mutant counterparts.
A 69-year-old male with change in mental status. (a) Coronal T2WI demonstrates a heterogeneous centrally necrotic mass in the left insular region extending to involve the frontal lobe. (b) Axial FLAIR image demonstrates FLAIR signal abnormality surrounding this lesion which shows indistinct margin with the adjacent brain. (c) Axial T1 post-contrast image demonstrates heterogeneous but predominantly peripheral intense enhancement. (d) Corresponding axial DSC (dynamic susceptibility contrast) perfusion map demonstrates increased relative blood volume from the enhancing component of this lesion. Diagnosis: IDH-wildtype glioblastoma
6 1p/19q-Codeletion
IDH-mutant gliomas can subsequently be classified into those which are 1p/19q-codeleted tumors or 1p/19q-intact tumors. Of these, those gliomas which are 1p/19q-codeleted are the oligodendrogliomas, while those which are 1p/19q-intact are astrocytomas [1, 12]. Astrocytomas typically also show TP53 mutation, a mutation which is never seen in oligodendrogliomas, another distinguishing feature that separates these two tumors. As mentioned previously, this 1p/19q-codeleted status and TP53 mutation help clearly separate the confusing oligoastrocytoma group into either oligodendroglioma or astrocytoma (which was not possible based on histological features alone), which helps to better manage these patients.
Key Points
-
1p/19q-codeletion status in an IDH-mutant tumor is diagnostic of oligodendroglioma;1p/19q-intact status with TP53 mutation is diagnostic of astrocytoma.
6.1 Clinical Relevance and Prognosis
It has been shown in two large randomized control trials that chemotherapeutic agents including procarbazine, lomustine, and vincristine (PCV) when added to radiation therapy significantly improve the overall survival in patients with 1p/19q-deleted tumors when compared with radiation therapy alone [23,24,25,26]. This therefore is now the standard of care for all 1p/19q-codeleted oligodendrogliomas.
6.2 Radiological Features
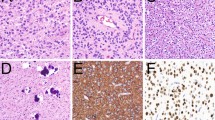
Frontal lobe is the most common location of 1p/19q-codeleted tumors. Other common sites include the parietal and occipital lobes. In contrast, 1p/19q-intact tumors are seen most often in the temporal lobes and the insular cortex. In terms of their morphological appearance, 1p/19q-codeleted tumors demonstrate a more heterogeneous appearance. Also, calcification is a common feature of such tumors. In fact, presence of florid calcification and enhancement favors a higher grade (grade 3) oligodendroglioma (Fig. 4.2) [14, 21]. An intact margin favors a 1p/19q-intact tumor while ill-defined margins can be seen in both types. T2-FLAIR mismatch sign demonstrates a high positive predictive value for 1p/19q-intact tumors, i.e., mass lesion which appears bright on T2WI and dark of FLAIR sequences (Fig. 4.3).
A 48-year-old man with seizures. (a) Axial T2WI demonstrates a heterogeneous mass involving the right frontal lobe. (b) Corresponding axial T1 post-contrast image demonstrates heterogeneous but minimal enhancement. (c) Axial CT scan from the same patient demonstrates multiple arcs of calcification within this mass. Diagnosis: oligodendroglioma, IDH-mutant, 1p/19a codeleted tumor
A 34-year-old man with headache. (a) Axial T2WI demonstrates a well-defined expansile mass involving the left insula, which appears predominantly bright in its signal intensity when compared to the gray matter. (b) Corresponding axial FLAIR image demonstrates the mass to be predominantly hypointense to the gray matter. Diagnosis: diffuse astrocytoma, IDH-mutant, 1p/19q-noncodeleted (intact) tumor
7 Gliomatosis Cerebri
Gliomatosis cerebri as a specific tumor subtype was included in the 2007 version of the WHO classification of CNS tumors. This term is deleted from the 2016 update [1]. A diffusely infiltrating non-enhancing tumor extending to involve 3 or more lobes is no longer to be considered as gliomatosis cerebri. It is recognized as a diffuse glioma type, with its subtype dependent on further genetic, molecular testing and histological evaluation [1].
Key Points
-
Gliomatosis cerebri as a tumor term is no longer recognized.
8 CNS Tumor Nomenclature, Integrated Diagnosis, and Layered Reports
The term “anaplastic” previously used to describe grade 3 tumors is no longer used. Also, Roman numerals to grading tumors is no longer recommended. It is thought that a typographical error, such as grade II instead of grade III, and similar such mistakes can lead to bad clinical consequences. Hence, Arabic numerals used for other body parts to grade tumors are recommended to describe CNS tumors. It is now recommended that a layered report be used to describe a CNS tumor, which provides histological diagnosis, grade of the tumor, and the mutation status in that order. For example, if oligodendroglioma has to be described, it should be mentioned as oligodendroglioma, grade 3, and IDH-mutant 1p/19q codeleted tumor. Also, the mutation status establishes the grading and not the histology, i.e., if a tumor by histology appears as grade 1, but it carries a TERT-promoter or similar poor prognostic mutation commonly associated with grade 4 tumors, the tumor under consideration in the final report should be read out as a grade 4 tumor [2].
Other terms clearly outlined in the 2021 WHO classification of tumors include NOS (not otherwise specified) and NEC (not elsewhere classified). NOS refers to a tumor which after extensive molecular work-up does not demonstrate a clear molecular signature for it be appropriately classified. NEC refers to a tumor which despite an adequate pathological work-up does not conform to a standard WHO diagnosis [2].
Key Points
-
Arabic and non-Roman numerals are now recommended to be used to describe CNS tumors.
-
Integrated diagnosis, including histology, grade of tumor, molecular profile is the correct way to completely describe a tumor.
-
Molecular profile dictates grade of tumor and not histology.
9 Gliomas in Children
Gliomas in children have been known to behave differently than those seen in the adult population. This is related to the fact that mutations seen commonly in gliomas in adults including IDH mutation and 1p/19q-codeletion occur uncommonly in children. The two common mutation types commonly seen in children, include BRAF mutation and histone H3K27 altered [27, 28].
10 BRAF Mutation
These tumors are usually well circumscribed and carry an excellent prognosis.
10.1 Radiological Features
Cystic lesions with a mural enhancing nodule are common imaging features (Fig. 4.4). This mutation type encompasses pilocytic astrocytoma, pilomyxoid astrocytoma, and ganglioglioma.
An 18-year-old boy with seizures. (a) Axial T2WI demonstrates a well-defined cystic appearing lesion in the right temporal lobe. (b) Corresponding axial T1 post-contrast image demonstrates a mural enhancing nodule along the lateral aspect of this lesion. Diagnosis: pleomorphic xanthoastrocytoma, BRAF-mutant tumor
Key Points
-
BRAF mutation is one of the most common mutations seen in the pediatric population and includes tumor types such as pilocytic astrocytoma, pilomyxoid astrocytoma, and ganglioglioma.
11 Histone H3K27 Altered Tumors
These are diffuse midline gliomas (previously known as diffuse infiltrating pontine glioma) and carry an extremely poor prognosis. Often times they are seen in the brainstem. Location of this tumor type makes it difficult to biopsy these tumors or attempt a surgical resection [28]. They are now known to occur at other sites including the thalami, spinal cord, and sometimes, the cerebral parenchyma. Radiation and chemotherapy are not particularly helpful.
11.1 Radiological Features
Brainstem (pons) is the most common location. Other common locations include thalami and spinal cord. As previously described, this is a diffusely infiltrating lesion which results in secondary expansion of the structure involved. Enhancement is variable. Occasionally, heterogeneous enhancement and cyst(s) can be seen. Leptomeningeal dissemination is seen in about one-third of all autopsies.
Key Points
-
H3K27 altered glioma now includes the previously known diffuse infiltrating pontine glioma in its genetic profile of tumors and carries a dismal prognosis.
12 Solitary Fibrous Tumor (SFT) and Hemangiopericytoma (HPC)
Both these tumors share the same genetic feature which includes genomic inversion at the 12q13 locus, fusing the NAB2 and STAT6 genes. Hence, these 2 previously distinct tumors were combined as SFT/HPC tumor as per the 2016 revised WHO classification of CNS tumors [1]. This was further revised to document these as SFT tumors deleting the term hemangiopericytoma (HPC) to clearly indicate the soft tissue origin of the tumor by the 2021 update on classification of CNS tumors [2]. Three grades have been described with SFT grade 1 a slowly growing tumor carrying excellent prognosis, while SFT grades 2 and 3 have a slightly poor prognosis, carry a high risk to recur following resection, and are associated with metastasis.
Newly recognized tumor types in the revised 2021 WHO classification of CNS tumors diffuse leptomeningeal glioneuronal tumor (first described in 2016).
This is a rare glioneuronal neoplasm mainly seen in children. It is largely localized to the leptomeningeal compartment [1]. Oligodendroglioma-like tumor cells are seen at histology.
12.1 Radiological Features
Cluster of diffuse leptomeningeal enhancement is noted. Frequently, the basal cisterns are involved with associated extensive involvement of the subarachnoid space along the surface of the cord. Secondary hydrocephalus is commonly noted. Parenchymal involvement can also be seen. When present, it is seen to involve the spinal cord and the brain stem.
In addition, at least 22 new tumor types have been recognized in the revised 2021 WHO classification of CNS tumors (Table 4.1) [2]. A discussion of all of these is beyond the scope of this text. One of the more common of these entities is the multinodular and vacuolating neuronal tumor as outlined below.
13 Multinodular Vacuolating Neuronal Tumor
This rare entity first received mention in the 2016 revised CNS tumor classification. At that time, it was unclear if this was distinct tumor or in the tumor-dysplasia category. In the 2021 revised classification, it has been recognized as a tumor. It carries an excellent prognosis and is believed to be a “Touch-Me-Not” lesion [29].
13.1 Radiological Features
It is known to occur anywhere in the brain but commonly in the supratentorial compartment and especially in the frontal and temporal lobes. On morphological appearance, the lesion is seen as a cluster of FLAIR and T2 bright lesions typically in the subcortical white matter. Involvement of the overlying cortex and periventricular white matter has been reported. The lesion appears hypointense on T1WI and does not demonstrate contrast enhancement or diffusion restriction. No susceptibility is seen.
14 Conclusion
Concluding Remarks
The revised 2016 and subsequently 2021 classification systems of CNS tumors by including the genetic profile improve diagnostic accuracy of brain tumors. This allows neuro-oncologists and the surgeons to optimize treatment strategies targeted to the specific tumor type, thus allowing for a better prognosis and improved overall survival. The neuroradiologist by identifying the imaging phenotype of the particular glioma genotype plays an important role in guiding the clinical team in their treatment planning.
Take-Home Messages
-
IDH-mutated tumors are more solid in their imaging profile and demonstrate less enhancement than IDH-wildtype counterparts.
-
1p/19q-codeleted tumors are more heterogeneous in their imaging appearance and exhibit calcification more frequently than their 1p/19q-intact counterparts.
-
BRAF mutant tumors seen more commonly in the pediatric population. These include pilocytic astroctyoma, pilomyxoid astrocytoma, and ganglioglioma in their molecular profile spectrum.
-
H3K27 altered tumors are also seen more commonly in the pediatric population. They are more diffuse and aggressive. These mutant tumors encompass the previously described diffuse infiltrating pontine glioma spectrum of tumors.
-
New tumor types now recognized have helped us better classify and understand CNS tumors.
References
Louis DN, et al. The 2016 World Health Organization classification of tumors of the central nervous system. Acta Neuropathol. 2016;131(6):803–20.
Louis DN, et al. The 2021 WHO classification of the central nervous system: a summary. Neuro-Oncology. 2021;23(8):1231–51.
Louis DN, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114(2):97–109.
Giannini C, et al. Oligodendrogliomas: reproducibility and prognostic value of histologic diagnosis and grading. J Neuropathol Exp Neurol. 2001;60:248–62.
van den Bent MJ. Interobserver variation of the histopathological diagnosis in clinical trials on glioma: a clinician’s perspective. Acta Neuropathol. 2010;120:297–304.
Cancer Genome Atlas Research Network, Brat DJ, et al. Comprehensive integrative genomic analysis of diffuse lower-grade gliomas. N Engl J Med. 2015;372:2481–98.
Metellus P, et al. Absence of IDH mutation identifies a novel radiologic and molecular subtype of WHO grade II gliomas with dismal prognosis. Acta Neuropathol. 2010;120(6):719–29.
Sahm F, et al. Farewell to oligoastrocytoma: in situ molecular genetics favor classification as either oligodendroglioma or astrocytoma. Acta Neuropathol. 2014;128:551–9.
Wiestler B, et al. Integrated DNA methylation and copy-number profiling identify three clinically and biologically relevant groups of anaplastic glioma. Acta Neuropathol. 2014;128:561–71.
Huse JT, et al. Mixed glioma with molecular features of composite oligodendroglioma and astrocytoma: a true “oligoastrocytoma”? Acta Neuropathol. 2015;129:151–3.
Wilcox P, et al. Oligoastrocytomas: throwing the baby out with the bathwater? Acta Neuropathol. 2015;129:147–9.
Appin CL, et al. Molecular pathways in gliomagenesis and their relevance to neuropathologic diagnosis. Adv Anat Pathol. 2015;22(1):50–8.
Cohen AL, et al. IDH1 and IDH2 mutations in gliomas. Curr Neurol Neurosci Rep. 2013;13(5):345.
Smits M, et al. Imaging correlates of adult glioma genotypes. Radiology. 2017;284:316–31.
Yan H, et al. IDH1 and IDH2 mutations in gliomas. N Engl J Med. 2009;360(8):765–73.
Beiko J, et al. IDH1 mutant malignant astrocytomas are more amenable to surgical resection and have a survival benefit associated with maximal surgical resection. Neuro-Oncology. 2014;16(1):81–91.
Esmaeili M, et al. 2-hydroxyglutarate as a magnetic resonance biomarker for glioma subtyping. Transl Oncol. 2013;6(2):92–8.
Andronesi OC, et al. Detection of 2-hydroxyglutarate in IDH-mutated glioma patients by in vivo spectral-editing and 2D correlation magnetic resonance spectroscopy. Sci Transl Med. 2012;4(116):116ra4.
Bertolino N, et al. Accuracy of 2-hydroxyglutarate quantification by short-echo proton-MRS at 3T: a phantom study. Phys Med. 2014;30(6):702–7.
Pope WB, et al. Non-invasive detection of 2-hydroxyglutarate and other metabolites in IDH1 mutant glioma patients using magnetic resonance spectroscopy. J Neurosci. 2012;107(1):197–205.
Khalid L, et al. Imaging characteristics of oligodendrogliomas that predict grade. AJNR Am J Neuroradiol. 2012;33(5):852–7.
Willman M, et al. Update for astrocytomas: medical and surgical management considerations. Explor Neurosci. 2023;2:1–26.
Weller J, et al. PCV chemotherapy alone for WHO grade 2 oligodendroglioma: prolonged disease control with low risk of malignant progression. J Neuro-Oncol. 2021;153:283–91.
Cairncross G, et al. Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402. J Clin Oncol. 2013;31:337–43.
van den Bent MJ, et al. Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of EORTC brain tumor group study 26951. J Clin Oncol. 2013;31:344–50.
Patel SH, et al. T2-FLAIR mismatch, an imaging biomarker for IDH and 1p/19q status in lower-grade gliomas: a TCGA/TCIA project. Clin Cancer Res. 2017;23:6078–85.
Tan JY, et al. Paediatric gliomas: BRAF and histone H3 as biomarkers, therapy and perspective of liquid biopsies. Cancers (Basel). 2021;13:607.
Nunes RH, et al. Multinodular and vacuolating neuronal tumor of the cerebrum: a new “leave me alone” lesion with a characteristic imaging pattern. AJNR Am J Neuroradiol. 2017;38:1899. https://doi.org/10.3174/ajnr.A5281.
Louis DN, Perry A, Wesseling P, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021;23(8):1231–51.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Fatterpekar, G.M., Sundgren, P.C. (2024). Cerebral Neoplasms. In: Hodler, J., Kubik-Huch, R.A., Roos, J.E. (eds) Diseases of the Brain, Head and Neck, Spine 2024-2027. IDKD Springer Series. Springer, Cham. https://doi.org/10.1007/978-3-031-50675-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-50675-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-50674-1
Online ISBN: 978-3-031-50675-8
eBook Packages: MedicineMedicine (R0)