Abstract
In paediatric patients fluid management has various aspects that differ from adults. One of the reasons is the different physiology of body fluids in children. Dehydration occurs commonly in children and requires resuscitation. Administration of fluid resuscitation is essential in critically ill children. Early and appropriate resuscitation improves outcomes and reduces mortality in children. In this chapter, we present an evidence-based approach for fluid management in critically ill children.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
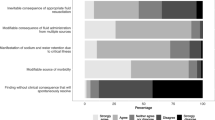
FormalPara IFA Commentary (MLNGM)In critically ill children, the administration of fluids is a crucial aspect of their management. The type and amount of fluid given to a critically ill child depends on their clinical condition and fluid status. Resuscitation fluids are used to treat hypovolemia and hypotension in critically ill children in shock. The aim of resuscitation is to restore and maintain adequate tissue perfusion, oxygenation, and organ function. Commonly used fluids include crystalloids (such as normal saline, lactated Ringer’s solution, and balanced salt solutions) and colloids (such as albumin). The choice of resuscitation fluid depends on the underlying condition of the child, the degree of hypovolemia, and the presence of any comorbidities. It is important to monitor the child’s response to resuscitation fluids closely and adjust the type and amount of fluid as needed. Replacement fluids are used to correct fluid and electrolyte imbalances in critically ill children. The aim of replacement therapy is to maintain homeostasis and prevent complications associated with fluid and electrolyte disturbances. Replacement fluids are usually isotonic solutions such as normal saline, lactated Ringer’s solution, and balanced salt solutions. In some cases, hypotonic solutions, such as 0.45% saline, may be used to correct hypernatremia or hypertonic dehydration. The amount and composition of replacement fluids depend on the child’s clinical condition and fluid status. Maintenance fluids are used to maintain hydration and electrolyte balance in critically ill children who are unable to take fluids orally. The aim of maintenance fluid therapy is to replace ongoing losses and prevent dehydration and electrolyte disturbances. The amount and composition of maintenance fluids depend on the child’s age, weight, and clinical condition. The most commonly used fluids for maintenance therapy are isotonic solutions such as normal saline, lactated Ringer’s solution, and balanced salt solutions. The rate of maintenance fluid administration should be adjusted according to the child’s ongoing fluid losses and response to therapy. In contrast to adults where there is a shift towards hypotonic intravenous maintenance fluid therapy (IV-MFT), in children isotonic maintenance is still preferred because of the risk for hyponatremia. The recently published ESPNIC guidelines propose 16 recommendations based on a literature search and expert consensus (Table 20.1) [1]. Although there is a high level of consensus, the level of evidence for most recommendations is low. The recommendations are consistent with previous guidelines, including the use of isotonic fluids, reduced infusion volumes, and the use of the enteral route when possible. However, the researchers note that the reporting of key outcomes was inconsistent, which prevented further meta-analyses. The study raises several implications for practice, including highlighting the importance of IV fluid composition, glucose and plasma electrolyte monitoring, and the potential harm of excessive fluids and volume overload. The authors acknowledge the challenge of implementing these recommendations, particularly due to the lack of availability of ready-to-use IV-MFT solutions in some countries. In summary, resuscitation, replacement, and maintenance fluids are used in the management of critically ill children to restore and maintain fluid and electrolyte balance, correct imbalances, and prevent complications associated with fluid and electrolyte disturbances. The choice of fluid, amount, and composition of fluids depends on the underlying condition and clinical status of the child, and should be closely monitored and adjusted as needed.
Suggested Reading
-
1.
Brossier DW, Tume LN, Briant AR, Jotterand Chaparro C, Moullet C, Rooze S, Verbruggen S, Marino LV, Alsohime F, Beldjilali S et al: ESPNIC clinical practice guidelines: intravenous maintenance fluid therapy in acute and critically ill children—a systematic review and meta-analysis. Intensive Care Med. 2022;48(12):1691–708.
After reading this chapter, you will:
-
1.
To learn about the physiology of body fluids in children.
-
2.
The difference in distribution of body fluids at different stages of paediatric age group.
-
3.
Evidence-based approach for choosing the type of fluid for resuscitation, replacement and maintenance fluid.
-
4.
To learn about the fluid management in various common clinical scenarios in paediatric age group.
A 2-year-old boy presented to the emergency department with a 2-day history of watery loose stools. His oral intake was poor, and he had passed urine once since morning. His eyes appeared sunken and had a weak cry. On examination his peripheral pulses were very feeble, peripheries were cool, capillary filling time was prolonged (>3 s) and blood pressure was at fifth centile for his age.
Question
-
Q1. What are the clinical considerations while managing this child?
Introduction
Children are more prone to water and electrolyte imbalances compared to adults for a number of reasons: (a) higher total body water content [1], (b) relatively higher insensible losses due to a higher surface area to body mass ratio [2, 3] and (c) possible presence of immature regulatory mechanisms [4, 5]. Hence fluid therapy in children should be considered challenging in all respects and should be treated as a pharmacological intervention with precise indications, contraindications and adverse effects.
Physiology of Body Fluid in Children
In children, the relative amount of body water varies considerably with age [6]. Total body water (TBW) is 90% of the body weight in the fetus, predominantly in the extracellular compartment (ECF represents ~65% of TBW). In a full-term newborn baby, TBW constitutes 75–80% of body weight; the intracellular fluid (ICF) increases to ~45% of TBW and consequently, the proportion of ECF undergoes a relative decrease to ~55% of TBW. In the first year of life due to an increase in fat, TBW reduces to around 60%. The ratio of ECF to ICF continues to change, with increase in ICF to 60% of TBW at the end of the first year and ECF accounting for the remaining 40%. The relative drop in ECF is mainly due to a reduction in interstitial fluid, while the percentage of intravascular fluid appears to be fairly constant. In a child, TBW is ≈60% with ICF being 35% of TBW. A similar ratio is seen in adults (Table 20.2).
The composition of intra-/extracellular fluids and regulation of body water in children is not different from that of normal adults and is detailed in Chaps. 2 and 3. The composition of different intravenous fluids is described in Chap. 9. Briefly, isotonic fluids have a composition similar to ECF, whereas hypotonic fluids are lower in tonicity and potassium concentration compared to plasma (Table 20.3). Isotonic fluids are used for fluid resuscitation, to correct an acute intravascular fluid deficit and for the replacement of extracellular fluid losses. Most intravenous fluids employed in the paediatric population contain glucose, ranging between 5% and 10%.
Fluids for the Paediatric Population: Resuscitation, Replacement and Maintenance
There is a strong consensus in favour of using isotonic, possibly balanced fluids peri-operatively and for resuscitation and replacement in the paediatric intensive care unit [7] although there remains significant heterogeneity in clinical practice. In a survey by Way et al., about 10% of anesthesiologists reported a prescription practice of using a bolus of hypotonic dextrose saline to treat intraoperative hypovolemia in the paediatric population [8].
The ideal tonicity of maintenance fluids in the paediatric population is still debated [9,10,11,12]. The physiological rationale is to prescribe maintenance fluids in children to replace fluids lost through urinary output and insensible losses when oral or enteral intake is not possible. In theory, at least, the composition of maintenance fluids should be similar to that of lost fluids. Additionally, maintenance fluids should be able to hydrate both the extracellular and the intracellular compartments. Table 20.4 gives an overview of the composition of the different compartments. Since fluids lost through skin, lung and stool (insensible loss) or through urine are hypotonic, a number of experts argue that maintenance fluids should be hypotonic. They believe that hypotonic fluid will reduce plasma osmolarity, generate osmotic driving pressure and allow water movement from the extra- to the intracellular compartment, hydrating both compartments.
Reduction in plasma osmolarity should suppress anti diuretic hormone (ADH) secretion. Hence in physiologic conditions, there will be excretion of electrolyte-free water through diluted urine. However, in critically ill or hospitalized children, ADH secretion is stimulated by the presence of several non-osmotic stimuli, resulting in an inability to excrete free water. In the presence of inappropriately high ADH levels, administration of hypotonic fluid in critically ill children is likely to result in positive water balance and may increase the risk of water intoxication and hyponatremia with consequent neurologic disorders. For these reasons, another group of experts advocates the use of isotonic instead of hypotonic fluids for maintenance therapy in hospitalized children.
In a single-centre study from Canada, 258 post-operative patients from 6 months to 16 years of age were randomized to receive either isotonic (0.9% saline) or hypotonic (0.45% saline) as maintenance solution for 48 h. Hypotonic fluids significantly increased the risk of hyponatremia, compared to isotonic saline (40.8% vs 22.7%), but 0.9% saline was not associated with increased risk of hypernatremia. Interestingly, ADH levels and risk of adverse events were not different between the two groups [13].
The risk of developing hyponatremia in the paediatric population was recognized by the American Academy of Pediatrics (AAP). AAP recommends that paediatric patients in the age group between 28 days and 18 years requiring intravenous maintenance fluid should receive isotonic solutions with appropriate potassium and dextrose [14].
In acutely ill children there is limited evidence regarding the optimal fluid therapy. In a recent trial by Lehtiranta et al. to evaluate the risk of electrolyte disorders and fluid retention in a group of acutely ill children receiving plasma-like isotonic fluid therapy. It was conducted at Oulu University Hospital, Finland, from October 2016 to April 2019. A total of 614 children were randomized to receive commercially available plasma-like isotonic fluid (140 mmol/L of sodium and 5 mmol/L potassium in 5% dextrose) or moderately hypotonic fluid (80 mmol/L sodium and 20 mmol/L potassium in 5% sextrose). It was found that the risk of electrolyte disorders was 6.7 times greater in children who received isotonic fluids compared to hypotonic fluids. Hypokalemia was found to be a significant electrolyte disorder [22].
Individual Clinical Scenarios
Children with Dehydration
Dehydration is the most common cause of fluid and electrolyte disturbance-related critical illness in children globally. The first step in management is to assess the degree of dehydration. Table 20.5 describes the assessment criteria for degree of dehydration.
After the initial assessment, the patient must be regularly re-evaluated during treatment. A good history can reveal the cause of dehydration. It may also help to predict isotonic, hypotonic or hypertonic dehydration. A neonate having poor intake of breast milk or a child with plenty of watery stools and poor oral intake often develop hypernatremic dehydration. On the other hand, a child with watery diarrhea who is only drinking large quantities of plain water or low-salt fluid will have hyponatremic dehydration. Physical examination can determine the degree of dehydration but it may be difficult to assess the skin pinch in premature infants or severely malnourished children.
Calculation of Fluid Deficit
Assess the degree of dehydration and multiply the percentage of dehydration with patient’s weight (converting the unit to litre). For example, a 10 kg child with 10% dehydration has a fluid deficit of 1 L.
Fluid Management
A child with severe dehydration needs acute intervention in the form of adequate fluid resuscitation. The resuscitation phase ensures rapid restoration of intravascular volume. Initial fluid choices are crystalloids e.g. 0.9% saline or Ringer’s lactate. Colloids like 5% albumin, blood and FFP are not the initial choice but can be considered if the patient has bleeding manifestations with underlying coagulopathy. The initial fluid bolus is 20 mL/kg of crystalloids, given within 10–20 min. Children with severe dehydration may require multiple fluid boluses for adequate restoration of intravascular volume.
After initial resuscitation, the maintenance plus deficit is to be calculated for 24 h. After deducting the fluid boluses, the rest of the calculated fluid needs to be administered over 24 h. Let us now take an example of a 10 kg child with 10% dehydration:
-
Total deficit volume = 1000 mL (by multiplying the percentage of dehydration with body weight of the child in litre).
-
Maintenance fluid requirement = 1000 mL (by applying is Holiday Segar formula, 100 mL/kg for first 10 kg i.e. 1000 mL).
-
Fluid bolus given once = 200 mL (20 mL/kg).
-
The remaining deficit plus maintenance fluid volume of 1800 mL (1000 mL + 1000 mL − 200 mL) is to be given over 24 h.
Potassium is added to the maintenance fluid once the child passes urine. Children in whom significant ongoing losses are present need to receive replacement solutions.
Holliday-Segar formula for maintenance fluid requirements by weight | |||
|---|---|---|---|
Weight (kg) | Water | Electrolytes (mEq/L H2O and mmol/L H2O) | |
mL/day | mL/h | ||
0–10 | 100/kg | 4/kg | Sodium 30 |
Potassium 20 | |||
11–20 | 1000 + 50/kg for each kg >10 | 40 + 2/kg for each kg >10 | Sodium 30 |
Potassium 20 | |||
>20 | 1500 + 20/kg for each kg >20 | 60 + 1/kg for each kg >20 | Sodium 30 |
Potassium 20 | |||
Hypernatremic Dehydration is dangerous due to complications of hypernatremia as well as its therapy. The child is usually lethargic and irritable and can manifest with neurologic symptoms. In hypernatremia, the movement of water from intracellular to extracellular space helps to preserve intravascular volume. By the time they receive medical attention, they would already be profoundly intracellularly dehydrated. Initial fluid resuscitation for hypernatremic dehydration should be with 0.9% saline with the aim of restoring intravascular volume. Ringer’s lactate should be avoided as it may lead to a rapid reduction of sodium levels. To minimize the risk of cerebral edema, serum Na should not decrease by >12 mEq/L in 24 h. The rate of correction will depend on the initial sodium level.
Once the intravascular volume is restored, further correction of dehydration can be achieved with 5% dextrose with ½ normal saline that has a higher content (50% more) of free water than 0.9% saline. The sodium concentration of the IV fluids should be adjusted according to serum sodium levels. One way of achieving the target is to use two different fluids with varying sodium concentrations e.g. 5% Dextrose with 1/4 normal saline and 5% Dextrose with normal saline. If serum sodium levels decrease rapidly, the rate of 5% Dextrose with normal saline may be increased with a simultaneous decrease in the rate of 5% Dextrose with 1/4 normal saline. Rapid reduction in serum sodium may precipitate seizures as a manifestation of cerebral edema, requiring acute correction with an infusion of 3% saline at a dose of 4 mL/kg. When the child is conscious and ready to accept oral fluids, plain water or hypotonic fluids should be avoided.
Hyponatremic Dehydration involves loss of both sodium and water in stools with a higher loss of sodium relative to water. Also, volume depletion stimulates ADH synthesis resulting in a reduction of renal excretion of free water. The initial goal is to correct intravascular volume losses with isotonic fluids; most patients respond well to basic management as outlined for dehydration. Care should be taken to avoid overly rapid correction of Na > 12 mEq/L in 24 h as this can be associated with the risk of central pontine myelinolysis. Serum sodium should be monitored closely; if the patient presents with neurologic symptoms as a result of hyponatremia, 3% saline should be given to raise serum sodium rapidly.
Sepsis and Septic Shock
There is no specific recommendation regarding the optimal type of resuscitation fluid in the management of paediatric sepsis. Isotonic crystalloids are recommended as the initial fluid of choice [15]. Fluid boluses of 20 mL/kg over 5 min up to 60 mL/kg can be given till perfusion improves; these can be given by push or pressure bag devices while simultaneously observing for signs of fluid overload i.e. rales, gallop rhythm, hepatomegaly [15] .
However, the concept of administering fluid boluses in paediatric septic shock has recently been challenged following the landmark FEAST study [16]. In this study, Maitland and colleagues randomized 3170 children with evidence of hypoperfusion into three groups: (a) albumin-bolus group that received 20–40 mL of 5% albumin solution per kg of body weight, (b) saline-bolus group receiving 20–40 mL of 0.9% saline solution per kg of body weight and (c) control group, which received no fluid bolus. All three groups received maintenance fluids at a rate of 2.5–4 mL/kg/h. Compared to the control group, mortality rate was significantly higher in both bolus groups at 48 h and also at 4 weeks; mortality was related mostly to cardiovascular failure. Interestingly, mortality rates were not significantly different between the bolus groups. However, criticisms of the study include its external validity in high- and middle-income countries (the study was conducted in sub-Saharan Africa), large number of children with malaria being enrolled and possibility of worsening pre-existing anemia by hemodilution in bolus groups.
Fish Trial (Fluids in Shock)
It was a pilot RCT conducted across 13 hospitals in England from July 2016 to April 2017. It aimed to evaluate whether a restricted fluid bolus of 10 ml/kg compared with the current recommendation of 20 mL/kg is associated with improved outcomes in children presenting to UK emergency departments with presumed septic shock. Seventy-five participants were randomized. The volume of study bolus fluid after 4 h was 44% lower in the 10 mL/kg group. Length of hospital stay, PICU free days at 30 days did not differ significantly between the groups. It was observed that severity of illness in participants in the trial group was less than expected.
Further fluid administration after the initial resuscitation should be guided with hemodynamic variables and must be re-evaluated periodically.
Diabetic Ketoacidosis
In diabetic ketoacidosis (DKA) extracellular fluid deficit is usually in the range of 5–10%. In moderate DKA ECF volume deficit is 5–7% and in severe DKA 7–10%. Unfortunately, clinical estimation of volume depletion is often inaccurate. Some simple means of diagnosing ECF contraction are increases in urea nitrogen and hemoglobin concentration. Serum sodium concentration, an otherwise important marker for extracellular volume status, becomes unreliable in DKA, as osmotic effects of hyperglycemia cause a shift of water from intracellular to extracellular space, leading to dilutional hyponatremia. A simple formula can be utilized to calculate expected sodium, correcting the sodium level for hyperglycemia. In contrast, serum sodium should increase following correction of hyperglycemia with fluid infusion and insulin. Failure of serum sodium to rise or a paradoxical fall in sodium level following correction of glucose levels can be a sign of impending cerebral edema.
The goals of fluid therapy in DKA are:
-
Restoration of circulating volume.
-
Replacement of extracellular and intracellular fluid deficit.
-
Replacement of Na, K, Mg, PO4 and other electrolytes.
Fluid Therapy
Despite large overall volume deficits, patients in DKA rarely present in shock as their intravascular volume is usually preserved. Traditionally 0.9% saline is considered the fluid of choice for initial resuscitation and replacement of volume deficit. Current guidelines still recommend 0.9% saline over other fluids [17], though recent studies support the use of balanced salt solutions as the initial resuscitation fluid of choice for DKA in both adults and children because balanced salt solutions can restore the pH faster and avoid the risk of dilutional hyperchloremic metabolic acidosis [18, 19]. In a double-blind randomized control trial of 77 children with diabetic ketoacidosis, Yung and colleagues compared the effect of Hartman’s solution and 0.9% saline in achieving serum bicarbonate level >15 mmol/L [19]. In the overall population, the time to reach the primary end-point and time to normalize pH were not different between the two groups. However, in sicker patients, Hartman’s solution was able to normalize pH more quickly. Patients in the Hartman’s solution group also received less total fluid per kg [19]. There is no data to support the use of colloids in managing DKA.
-
Deficit replacement is calculated according to the percentage of dehydration. Maintenance fluid is calculated using the Holliday Segar formula. The daily maintenance requirement plus the deficit fluid is given over 24–48 h.
-
Initially, isotonic fluid may be administered at 10 mL/kg over 30–60 min.
-
If the peripheral perfusion is poor, a fluid bolus may be given more rapidly over 15–30 min and may be repeated till perfusion is restored. The bolus fluid is not calculated in the total fluid requirement.
-
Once the peripheral perfusion is restored, recent guidelines suggest using 0.45–0.9% saline to restore total body volume deficit [17].
-
Once RBS is below 250 mg/dL, 5% dextrose is added to fluids.
-
Clinical assessment of hydration status and effective osmolality are used to guide fluid therapy. Repeated measurements of electrolytes are also essential.
-
Rapid correction of hyperglycemia and high-volume fluid resuscitation in the first few hours are associated with an increased risk of cerebral edema. The risk of cerebral edema is also related to initial low sodium levels [20].
-
The use of chloride-rich fluids like isotonic saline leads to the development of hyperchloremia and dilutional hyperchloremic acidosis that may mask the resolution of ketoacidosis. To avoid this confusion, measurement of beta hydroxyl butyrate can be performed.
Case Vignette
In the vignette at the start of this chapter, this child is in moderate dehydration due to acute gastroenteritis. A fluid bolus of 0.9% normal saline at 20 mL/kg needs to be given as tissue perfusion is poor. The child needs to be reassessed for perfusion parameters and the possible need for a repeated bolus. If no further boluses are required, considering 10% dehydration, the deficit needs to be calculated by multiplying the percentage of dehydration by weight. This along with the maintenance fluid needs to be given over 24 h.
Conclusion
The decisions surrounding resuscitation with intravenous fluids vary according to disease states in sick children. Fluid therapy should be guided according to fluid status, electrolyte and glucose levels. If the initial assessment shows a poor peripheral perfusion, fluid boluses need to be given. Fluid therapy in cases of dehydration includes calculating the deficit volume and the maintenance volume. Sodium levels should be monitored as the type of fluid will change accordingly. In paediatric septic shock, the initial fluid bolus is still 20 mL/kg which can be given at a rapid rate up to 40–60 mL/kg, but signs of fluid overload must be monitored for. In DKA, if patient is in a volume-depleted state, the initial fluid bolus is 10 mL/kg which needs to be given slowly. Isotonic saline is still the fluid of choice for resuscitation. There is some evidence supporting balanced salt solutions in resuscitation but more studies are needed.
Take Home Messages
-
Fluid therapy should be guided according to the initial clinical assessment of the patient.
-
Children are more prone to fluid and electrolyte disturbances.
-
The type and rate of fluid administration will depend upon whether we use it for resuscitation, replacement or as maintenance fluid.
-
There is a strong consensus for using isotonic fluid as resuscitation and replacement fluid.
-
The ideal tonicity of maintenance fluid is still debated.
References
Friis-Hansen BJ, Holiday M, Stapleton T, et al. Total body water in children. Pediatrics. 1951;7(3):321–7.
Darrow DC, Pratt EL, Darrow DC, et al. Fluid therapy; relation to tissue composition and the expenditure of water and electrolyte. J Am Med Assoc. 1950;143(4):432–9.
Heeley AM, Talbot NB. Insensible water losses per day by hospitalized infants and children. AMA Am J Dis Child. 1955;90(3):251–5.
O’Brien F, Walker IA. Fluid homeostasis in the neonate. Paediatr Anaesth. 2014;24(1):49–59.
Mårild S, Jodal U, Jonasson G, et al. Reference values for renal concentrating capacity in children by the desmopressin test. Pediatr Nephrol. 1992;6(3):254–7.
Friis-Hansen B. Body water compartments in children: changes during growth and related changes in body composition. Pediatrics. 1961;28:169–81.
Sümpelmann R, Becke K, Crean P, et al. German Scientific Working Group for Paediatric Anaesthesia. European consensus statement for intraoperative fluid therapy in children. Eur J Anaesthesiol. 2011;28(9):637–9.
Way C, Dhamrait R, Wade A, et al. Perioperative fluid therapy in children: a survey of current prescribing practice. Br J Anaesth. 2006;97(3):371–9.
Duke T, Molyneux EM. Intravenous fluids for seriously ill children: time to reconsider. Lancet. 2003;362(9392):1320–3.
Moritz ML, Ayus JC. Prevention of hospital-acquired hyponatremia: a case for using isotonic saline. Pediatrics. 2003;111(2):227–30.
Holliday MA. Isotonic saline expands extracellular fluid and is inappropriate for maintenance therapy. Pediatrics. 2005;115(1):193–4.
Mattheij M, Van Regenmortel N. Maintenance fluids for children: hypotonic fluids are still the best choice. Pediatr Emerg Care. 2016;32(2):e4.
Choong K, Arora S, Ji C, et al. Hypotonic versus isotonic maintenance fluids after surgery for children: a randomized controlled trial. Pediatrics. 2011;128(5):857–66.
Feld LG, Neuspiel DR, Foster BA, Leu MG, Garber MD, Austin K, et al. Clinical practice guideline: maintenance intravenous fluids in children. Pediatrics. 2018;142(6):e20183083.
Davis AL, Carcillo JA, Aneja RK, Deymann AJ, Lin JC, Nguyen TC, et al. American College of Critical Care Medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med. 2017;45:1061–93.
Maitland K, Kiguli S, Opoka RO, Engoru C, Olupot P, Akech SO, et al. Mortality after fluid bolus in African children with severe infection. N Engl J Med. 2011;364:2483–95.
Wolfsdorf JI, Glaser N, Agus M, Fritsch M, Hanas R, Rewers A, Sperling MA, Codner E. ISPAD clinical practice consensus guidelines 2018: diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Pediatr Diabetes. 2018;19(Suppl 27):155–77.
Chua HR, Venkatesh B, Stachowski E, Schneider AG, Perkins K, Ladanyi S, Kruger P, Bellomo R. Plasma-Lyte 148 vs 0.9% saline for fluid resuscitation in diabetic ketoacidosis. J Crit Care. 2012;27:138–45.
Yung M, Letton G, Keeley S. Controlled trial of Hartmann’s solution versus 0.9% saline for diabetic ketoacidosis. J Paediatr Child Health. 2017;53:12–7.
Edge JA, Jakes RW, Roy Y, Hawkins M, Winter D, Ford-Adams ME, Murphy NP, Bergomi A, Widmer B, Dunger DB. The UK case-control study of cerebral oedema complicating diabetic ketoacidosis in children. Diabetologia. 2006;49:2002–9.
Langer T, Limuti R, Tommasino C, van Regenmortel N, Duval ELIM, Caironi P, Malbrain MLNG, Pesenti A. Intravenous fluid therapy for hospitalized and critically ill children: rationale, available drugs and possible side effects. Anaesthesiol Intensive Ther. 2018;50(1):49–58. https://doi.org/10.5603/AIT.a2017.0058. Epub 2017 Nov 18. PMID: 29151001.
Lehtiranta S, Honkila M, Kallio M, et al. Risk of electrolyte disorders in acutely ill children receiving commercially available plasmalike isotonic fluids: a randomized clinical trial. JAMA Pediatr. 2021;175(1):28–35. https://doi.org/10.1001/jamapediatrics.2020.3383.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Ghosh, S. (2024). Fluid Management in Paediatric Patients. In: Malbrain, M.L., Wong, A., Nasa, P., Ghosh, S. (eds) Rational Use of Intravenous Fluids in Critically Ill Patients. Springer, Cham. https://doi.org/10.1007/978-3-031-42205-8_20
Download citation
DOI: https://doi.org/10.1007/978-3-031-42205-8_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-42204-1
Online ISBN: 978-3-031-42205-8
eBook Packages: MedicineMedicine (R0)