Abstract
This chapter discusses the importance of endogenous albumin, the most abundant plasma protein in the body. Albumin has diverse functions such as antioxidant, anti-inflammatory activities, intravascular buffering, drug metabolism, transport, distribution, and restoration of vascular endothelial integrity. It is also crucial for maintaining the endothelial glycocalyx layer in blood vessels. Critically ill patients may experience hypoalbuminemia, defined as serum albumin <35 g/L, due to reduced synthesis, malnutrition, increased loss, or increased catabolism. Observational studies show hypoalbuminemia as an independent predictor of worse outcomes, with a 10 g/L decrease in serum albumin linked to a higher risk of mortality, morbidity, longer ICU/hospital stays, and increased resource utilisation. Administering exogenous albumin targeting serum albumin >30 g/L may reduce complications, but further trials are needed. Exogenous albumin is used in the ICU for various indications, including resuscitation and deresuscitation. Evidence on its use as a plasma expander is inconclusive. Both high- (20%) and low-concentration (4 and 5%) albumin can be used for resuscitation if patients require additional fluid, despite receiving crystalloids. Albumin is safe and effective for plasma expansion in patients with sepsis and septic shock but should be avoided in traumatic brain injury. Judicious and vigilant use of albumin is recommended due to its cost and potential risks. Albumin administration should be based on clinical indications, and monitoring fluid balance and clinical parameters is critical to prevent fluid accumulation and oedema formation.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara IFA Commentary (MLNGM)The plasma oncotic pressure, which is primarily determined by endogenous albumin, is a critical factor in maintaining fluid balance and microvascular fluid dynamics. In addition to its contribution to oncotic pressure, albumin plays a crucial role in endothelial glycocalyx layer function, which affects fluid dynamics in the microvasculature. While some studies have suggested that albumin may be useful for fluid resuscitation in patients with sepsis and septic shock, the evidence supporting this approach is largely based on post-hoc analysis, rather than predefined studies. Furthermore, the use of albumin is associated with a significantly higher cost compared to crystalloids, and its efficacy remains controversial due to a lack of sound clinical evidence. Ongoing randomised trials, such as the ALBumin Italian Outcome Septic Shock-BALANCED Trial (ALBIOSS-BALANCED) and the albumin replacement therapy in septic shock (ARISS), may provide more definitive answers to these issues.
While the role of albumin in sepsis remains a matter of debate, it has a well-established role in the management of patients with decompensated cirrhosis and complications such as hepatorenal syndrome, spontaneous bacterial peritonitis, and large volume paracentesis. In these patients, albumin infusion is a critical component of treatment and has been shown to improve outcomes. Additionally, albumin has been used in other clinical scenarios such as cardiac surgery, burns, and trauma, where it may help to maintain oncotic pressure and prevent fluid shifts. However, further studies are needed to determine the optimal dosing and duration of albumin therapy in these contexts. Despite some controversies, albumin remains an important therapeutic option in critical care, and ongoing research is likely to refine our understanding of its role in fluid management.
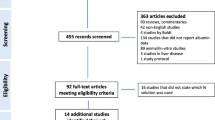
A recent paper addresses 10 myths about albumin therapy (Fig. 10.1).
-
Myth #1. Albumin leaks from the intravascular space into the interstitial compartment and contributes to oedema.
-
No, it does not.
-
Myth #2. Albumin is less effective for intravascular volume expansion than artificial colloids.
-
No, it is more effective.
-
Myth #3. Albumin administration prevents acute kidney injury.
-
Yes, in specific settings.
-
Myth #4. Albumin improves survival in sepsis.
-
Maybe, but it is still uncertain.
-
Myth #5. Albumin improves the effects of diuretics.
-
Yes, but only temporarily.
-
Myth #6. Albumin administration improves fluid removal during KRT.
-
Yes, it does.
-
Myth #7. Albumin decreases mortality in liver cirrhosis.
-
Yes, but only in specific subgroups.
-
Myth #8. Albumin increases mortality in traumatic brain injury (TBI).
-
Maybe, but we are not sure.
-
Myth #9. Albumin substitution to correct hypoalbuminemia from all causes reduces mortality.
-
No, it does not.
In this chapter, we will learn the physiology of albumin and the relation of hypoalbuminemia to clinically meaningful outcomes. We will review the evidence on plasma expansion with exogenous albumin in different indications.
FormalPara Case VignetteA 46-year-old female, 76 kg, with a history of inflammatory bowel disease, presented with pain in the abdomen for three days. On examination, she was anxious, with cold extremities, dry oral mucosa, heart rate of 132/min, and blood pressure (BP) of 78/46 mmHg. She was resuscitated with crystalloids (0.9% sodium chloride and Plasma-Lyte™). Despite, fluid resuscitation with 4.5 L crystalloids, norepinephrine 0.4 μg/kg/min, and vasopressin 0.04 units/min, she stayed hypotensive (MAP 60 mmHg); arterial blood gas showed metabolic acidosis with lactates 4.6. Passive leg raising test using pulse pressure variation confirmed fluid responsiveness.
Questions
-
Q1: Which intravenous fluids will you use for further resuscitation of this patient?
-
Q2: What will be the end points of resuscitation?
Introduction
Endogenous albumin is the most abundant plasma protein in the body. It has various functions (antioxidant and anti-inflammatory), restores vascular endothelial integrity, preserves and restores endothelial glycocalyx, helps in intravascular buffering, and the transport, distribution, and metabolism of various protein-bound drugs [1, 2]. Albumin plays a crucial role in maintaining the integrity of glycocalyx scaffold. Hypoalbuminemia defined as serum albumin <35 g/L is commonly observed in the critically ill.
The pathophysiological explanation of hypoalbuminemia during critical illness is complex and multifactorial. It involves reduced synthesis or malnutrition, increased loss (capillary leak, renal loss, protein-losing enteropathy), and/or increased catabolism [3].
Various observational studies explored the association between hypoalbuminemia and outcomes. In a meta-analysis of 90 cohort studies and five controlled trials, including 291,968 patients, hypoalbuminemia was an independent predictor of worse outcomes. Each 10 g/L drop in serum albumin was associated with a higher risk of mortality (137%), morbidity (89%), ICU or hospital length of stay (28% and 71%, respectively), and increased resource utilisation (66%). Exogenous albumin administration reduced the incidence of complications when targeting serum albumin concentrations of more than 30 g/L. However, the authors recommended prospective well-designed trials to verify the therapeutic effect of exogenous albumin in patients with hypoalbuminemia [4]. Intravenous (IV) exogenous albumin is often used in the intensive care unit (ICU) for various indications, from resuscitation to deresuscitation [5]. However, the evidence on the use of exogenous albumin as a plasma expander is conflicting. In this chapter, we will review the pharmacokinetics of albumin and the use of exogenous albumin for plasma expansion and other indications. More information on crystalloid solutions can be found in Chap. 9, while other colloid solutions like starches and gelatins are discussed in Chap. 11.
Albumin in Health
The human albumin accounts for 50–60% of plasma protein with a median half-life of 18–19 days. Albumin contributes to 70–80% of intravascular colloid oncotic pressure. Albumin is a negatively charged molecule constituted by 585 amino acids in a single polypeptide chain with a molecular weight of 66.5 KDa. Disulphide bridges provide structural resilience to the albumin; denaturation only occurs at highly abnormal conditions (extreme of temperature, pH, or chemical environment).
Serum albumin concentration depends on factors like rate of synthesis, degradation, and distribution in body compartments. The albumin pool measures about 3.5–5.0 g/kg/body weight, nearly 40% intravascular. The distribution half-time of endogenous albumin is 15 hours. Intravascular albumin leaks into the extravascular space at a rate of 5% per hour, known as transcapillary escape rate (TER). However, most of the leaked albumin is absorbed via the lymphatic systems and enters back in the blood. Small amount of albumin is lost in the gastrointestinal tract (1 g/day) and minimally through normal kidneys (10–20 mg/day).
In a normal state, around 9–14 g of albumin is synthesised daily by the liver and released in portal circulation. The liver has a limited capacity to increase the synthesis (by 2–2.7 times) and primarily depends on nutritional intake. Fasting decreases synthesis and insulin in combination with corticosteroids increase synthesis. However, corticosteroid plays a complex role in albumin metabolism as it increases its catabolism too.
Nearly 5% of albumin is degraded daily, with a turnover of around 9–14 g/day. The degradation occurs in most organs of the body, muscle, and skin (40–60%), liver (15%), kidneys, gastrointestinal tract, and others (10% each) .
Albumin plays a crucial role in microvascular fluid dynamics [6]. Greater understanding of the glycocalyx and its impact on fluid dynamics has challenged the “Starling equation” of protein-based transcapillary fluid exchange. The intravascular functional barrier is constituted by endothelial glycocalyx (made up of peptidoglycans, syndecan and glypican, glycoproteins, and plasma constituents, including albumin). The glycocalyx gets damaged during inflammation, sepsis, and trauma.
In healthy volunteers, 20% IV albumin administration causes significant plasma expansion via recruitment of interstitium. The plasma volume expansion peaks at 20 mins post-infusion and lasts beyond 5 h [7]. The low-concentration (4 to 5%) albumin can cause plasma expansion by approximately 80% of the administered volume and high-concentration albumin by approximately 210% (20% albumin) to 260% (25% albumin) [8]. Theoretically, this may translate to one-fourth of 20% albumin compared to balanced crystalloids required for resuscitation.
Albumin in Critical Illness
The critical illness alters the metabolism and distribution of endogenous albumin. During the early phase of illness, there is decreased synthesis and increased degradation, with altered distribution between body compartments. Inflammation, sepsis, and trauma decrease the rate of transcription of albumin mRNA. This may be due to a higher TER because of inflammatory damage to the endothelial barrier function and glycocalyx [1]. In septic shock, TER may increase by 300%, which saturates the absorption capacity of the lymphatic system. The pharmacokinetics of exogenous albumin is also altered in critically ill patients. The ratio of 4% albumin to 0.9% NaCl in the saline versus albumin fluid evaluation (SAFE) study to achieve hemodynamic targets was 1:1.4 [9]. This may be due to a higher TER because of inflammatory damage to the endothelial barrier function and glycocalyx [1].
Evidence on Albumin as a Plasma Expander
The role of albumin for plasma expansion during resuscitation is a matter of investigation for decades. Physiological rationale of albumin as plasma expansion is supported by higher blood pressure, both early and later resuscitation points, higher filling pressures, and lower cumulative fluid balance with albumin [9,10,11].
In a 1998 Cochrane meta-analysis involving 30 randomised controlled trials (RCTs), albumin administration was linked to an increased risk of mortality in critically ill patients [12]. The pooled risk of death with albumin administration was 1.02 (95% CI 0.95 to 1.16). In patients with hypovolemia, the pooled risk was 1.02 (95% CI 0.92 to 1.13). It influenced the practice around the world, especially in the United Kingdom. Since then, various large RCTs have evaluated the role of albumin for fluid resuscitation in the SAFE study, Early Albumin Resuscitation during Septic Shock (EARSS), or albumin replacement (ALBIOS) study in patients with sepsis [8, 13, 14].
The SAFE trial from 16 centres in Australia and New Zealand involving 6997 patients compared 4% albumin vs 0.9% sodium chloride (NaCl) as a resuscitation fluid in a heterogenous population of intensive care unit (ICU). No significant difference was found in day-28 mortality, duration of mechanical ventilation, need for renal replacement therapy, and length of ICU stay. A trend towards increased mortality was found with 4% albumin in the subgroup of patients with trauma (relative risk [RR] 1.36 [95% CI 0.99–1.86]; p = 0.06) [8]. Despite a mega RCT of 7000 patients, the study design had few issues. The study recruited a heterogenous population with mild to moderate severity of illness and recieved only a modest amount of fluid for replacement.
In a post-hoc analysis of the SAFE trial, statistically significant lower mortality was found with 4% albumin resuscitation in patients with severe sepsis (adjusted odds ratio 0.71 (95% CI 0.52–0.97]) [15]. Hence, the SAFE study demonstrated the safety aspect of administering exogenous albumin for fluid resuscitation and a trend towards benefit in patients with sepsis.
The multi-centre, open-label RCT (the EARSS study) from France, presented only in LIVES 2011, Berlin, Germany, comparing 20% albumin (8 hourly for 3 days) vs 0.9% NaCl, did not find any significant mortality difference between the two groups (24.1% vs 26.3%). However, the vasopressor requirement was significantly lower in the albumin group [14].
The ALBIOS trial, involving 1818 patients, compared crystalloids vs crystalloids and 20% albumin to correct hypoalbuminemia (targeting a serum albumin >30 gm/L or more) in the first 28 days of patients with sepsis and septic shock. The study design was different from the SAFE study and EARSS as end point of the study was the correction of albumin. There was no significant difference in day-28 and day-90 mortality [13]. The post-hoc analysis in patients with septic shock showed a significant 6.3% absolute reduction in mortality (43.6% vs 49.9%; RR: 0.87; 95% CI: 0.77–0.99) and quicker resolution of shock in the albumin group (3 vs 4 days, p = 0.007). The albumin group also had a lower cumulative negative fluid balance (347 ml vs 1220 ml, p = 0.004) [15].
Subsequently, the meta-analysis, including these trials, showed mixed results.
The meta-analysis of 16 RCTs by Patel et al. yielded no difference in outcome with albumin vs control fluid. However, most of the trials (13 out of 16) included were small, with fewer than 60 patients [16]. In another meta-analysis of five RCTs, comparing albumin with crystalloid, a trend to lower day-90 mortality was reported in patients with severe sepsis (0.88; 95% CI: 0.76–1.01; P = 0.08) who received albumin, which was significantly lower in patients with septic shock (OR 0.81; 95% CI: 0.67– 0.97; P = 0.03) [17]. An exploratory meta-analysis by Wiedermann et al., including three large RCTs, found a significant reduction in mortality with albumin use. However, this was not a formal meta-analysis and may need further analysis [18].
Recently, the albumin role has been investigated in a specific population of patients with sepsis. A single-centre, double-blind RCT, the Lactated Ringer Versus Albumin in Early Sepsis Therapy (RASP) study, investigated the effects of 4% albumin and Ringer’s lactate compared to Ringer’s lactate alone in 360 cancer patients with sepsis. No significant difference in day-28 (26% vs 22%) and day-90 (53% vs 46%) mortality was found between the groups and any other secondary outcomes [19].
In cirrhotic patients with sepsis, two single-centre RCTs investigated the role of albumin vs 0.9% NaCl (FRISC study) or Plasma-Lyte (ALPS study). The FRISC study reported significantly higher reversal of sepsis-induced hypotension, reduction of heart rate, lactate clearance, and lower day-7 mortality (38.3% vs 43.5%, p = 0.03), with 5% albumin resuscitation [20]. The ALPS study also reported a significantly higher proportion of patients attaining improvement in haemodynamics (mean arterial pressure of 65 mm hg or higher at 3 h) with 20% albumin compared to Plasma-Lyte (62% vs 22%). The albumin group also had higher lactate clearance. However, there was no difference in day-28 survival between the two groups [21].
An open-label pilot study evaluated the role of 100 ml of 20% albumin bolus (up to two treatments) in postoperative cardiac surgery patients with a crystalloid fluid bolus. The albumin group was associated with less median fluid balance at 24 h (1100 vs 1970, p = 0.001), shorter time to cessation of vasopressors (17 vs 28 h, p = 0.002), and decreased overall vasopressors requirement in the first 24 h (19 vs 47 μg/kg/24 h, p = 0.025) [22]. Despite no significant effect on coagulation function and lower volume required for resuscitation than 0.9% NaCl, albumin did not have any advantage over crystalloids in reducing mortality in patients with haemorrhagic shock [23]. The CRISTAL trial also failed to show any survival difference with colloids, including albumin [24].
Timing of Albumin Administration during Resuscitation
In a recent meta-analysis, including 55 RCTs and 27,036 patients, comparing crystalloids vs colloids for fluid resuscitation in ICU, crystalloid was found to be less efficient than colloids, including albumin, in achieving haemodynamic stabilisation end points [9]. The Surviving Sepsis Campaign 2021 guidelines suggested using albumin for fluid resuscitation in patients who received large volumes of crystalloid [25]. However, the optimal time to switch from crystalloids to albumin is still being determined. The SAFE and ALBIOS studies administered albumin within 28 days of randomisation and the RASP study within 6 h of randomisation [8, 13, 18]. No RCT has evaluated the optimal timing of albumin administration during fluid resuscitation. Recently, an expert group from the Chinese Society of Critical Care Medicine gave consensus recommendations on the timing of albumin administration in patients with septic shock. They recommended albumin administration in fluid-responsive patients along with haemodynamically unstablity even after resuscitation with crystalloids. The haemodynamic instability was defined as (1) failure to maintain a MAP ≥65 mmHg, despite receiving at least 30 mL/kg crystalloids and norepinephrine at a dose of ≥0.4 μg/kg/min, (2) frequent fluctuations in blood pressure, and (3) signs of apparent capillary leakage [2].
Comparison of Different Strengths of Albumin
Different concentration of albumin was used in studies, low (4% or 5%) and high concentrations (20% or 25%). Low-concentration albumin was used in the SAFE, FRISC and RASP trials [9120,21], and high-concentration was used in the ALBIOS and ALPS trials [12, 21]. Evidence supports adverse outcomes in patients with a positive cumulative fluid balance after the first week of ICU admission. A proposition of “small-volume resuscitation” using hyperoncotic albumin to reduce the total amount of fluid administered sparked interest in the ICU community. This utilises the oncotic properties of albumin to draw fluid from the interstitium and maximise the proportion of fluid staying in the intravascular compartment. A multi-centre RCT from Australia and the United Kingdom (the SWIPE study) compared 20% albumin vs 5% albumin for fluid resuscitation. The cumulative fluid balance was lower in the 20% albumin group at 48h (median difference: −576 ml; 95% CI: −1033 to −119; p = 0.01). There was no significant difference in secondary outcomes like duration of mechanical ventilation, the need for renal replacement therapy, or proportions of patients discharged from ICU [26]. However, no adverse events were reported with hyperoncotic albumin, and authors recommended further exploration of “small-volume resuscitation” in larger RCTs.
A recent meta-analysis of 26,351 patients in 58 clinical trials indicated no significant difference in the fatality rate or amount of resuscitation fluid between patients with sepsis who were administered low- and high-concentration albumin solutions [27]. Both concentrations of albumin can be used for volume expansion. In a recent survey by the International Fluid Academy, including 1045 participants, 54% agreed to use 20% albumin and 49% agreed to use 5% albumin for sepsis [28].
Albumin beyond Resuscitation
Patients with Liver Disease
Critically ill patients with cirrhosis are often admitted to ICU with complications like variceal bleeding, hepatic encephalopathy, and hepatorenal syndrome (HRS). Hypoalbuminemia is a poor prognostic marker in patients with cirrhosis. However, routine replacement of albumin in patients with decompensated cirrhosis failed to show any survival benefit [29].
Replacement of albumin (the ANSWER study) after large-volume paracentesis (LVP) was found to have lower mortality (HR 0.62; 95% CI: 0.35–0.64) and risk of refractory ascites (HR 0.43; 95% CI: 0.29–0.62) [30]. However, subsequent meta-analysis found conflicting results on the survival benefit of albumin replacement [31, 32].
Combined treatment with albumin with terlipressin is effective for the treatment of acute kidney injury associated with HRS and superior to albumin alone or in combination with other vasoconstrictors like midodrine and octreotide [33]. For patients with spontaneous bacterial peritonitis, albumin replacement with antibiotics can reduce mortality and the risk of AKI [34]. In a recent RCT, terlipressin alone or in combination with albumin was found to be an alternative therapeutic option in high- risk SBP [35].
Treatment of Hypoalbuminemia with Peripheral Oedema
In single-centre RCT, 20% albumin replacement to correct hypoalbuminemia (<31 g/dL) was associated with a greater improvement of organ failure compared to placebo [36]. Subsequent meta-analysis demonstrated that exogenous albumin administration in patients with hypoalbuminemia to achieve a serum albumin level > 30 g/L might be associated with lesser morbidity [4]. However, the multicentre ALBOIS study failed to show any survival benefit with albumin replacement to correct hypoalbuminemia [14].
Deresuscitation
Furosemide is commonly used in ICU for the treatment of fluid accumulation or peripheral oedema. However, hypoalbuminemia reduces the diuretic effect of the furosemide [37]. Combination of albumin and furosemide is synergistic in patients with hypoalbuminemia who need fluid removal. Two small trials have tested this combination for deresuscitation in patients with acute respiratory distress syndrome (ARDS). The retrospective case–control study, evaluated PAL (combination of PEEP, 20% albumin, and furosemide) treatment in patients with ARDS, and found a combination of albumin and furosemide was associated with improved clinical outcomes and lower net negative fluid balance, extravascular lung water, and intrabdominal pressure [38]. See Chap. 25.
In a small RCT of 40 patients, the intervention (albumin) group received a loading dose of 100 mL 25% albumin, followed by the initiation of a furosemide infusion. It was followed by 100 ml 25% albumin IV, repeated every 8 h for 3 days. The control group received 100 mL 0.9% saline every 8 h along with an infusion of furosemide. The albumin group had a significantly higher net negative fluid balance (−5480 mL vs −1490 mL) at the end of the study and greater improvement in their oxygenation index [39].
Other Indications
Albumin is also considered for fluid resuscitation in a patient with burns and extracorporeal membrane oxygenation. Albumin has the theoretical advantage of reducing the net positive cumulative balance, replacing plasma protein lost because of increased capillary permeability. However, the evidence on albumin for the resuscitation of patients with burns is conflicting.
Caution with the Use of Albumin
-
1.
High Sodium chloride load
Chloride-rich fluids administration has been linked to adverse outcomes in critically ill patients. Few commercial low-concentration albumin (4–5% albumin) solutions contain high sodium chloride. On the other hand, 20% albumin as a chloride-limited strategy was associated with a significantly lower incidence of hyperchloremia, despite no benefits in reducing adverse renal outcomes [40].
-
2.
Traumatic Brain Injury
The post-hoc analysis of the SAFE trial (the SAFE-TBI study) involving 460 patients with TBI found higher mortality with 4% albumin compared to 0.9% NaCl. Furthermore, in patients with intracranial pressure (ICP) monitoring, significantly higher ICP and more interventions were required in the albumin group. There was a higher proportion of deaths in the albumin group when the ICP monitoring was discontinued within the first week (34.4% vs 17.4%, p = 0.006) [41]. However, higher mortality could result from hypotonic 4% albumin used in the SAFE study [42]. Hence, these findings need verification in well-planned RCTs, and at present it is pragmatic to avoid albumin in traumatic brain injury.
-
3.
Leakage of albumin and contributes to edema
Systemic inflammation associated with sepsis, trauma, and surgery can affect the endothelial barrier function and glycocalyx. This may cause the extravascular leak of albumin through higher TER. However, albumin does not stay in the interstitium and re-enters the intravascular compartment through absorption into the lymphatic system. Leakage from pulmonary vessels and resulting pulmonary oedema depend on the transcapillary difference between oncotic and interstitial pressures. Exogenous albumin infusion can restore the oncotic pressure gradient because of hypoalbuminemia associated with sepsis [1].
-
4.
Adverse reactions related to blood products
Albumin is produced from pooled human plasma, and the same vigilance is required as other blood products, though pasteurisation during production reduces the risk of microbial transmission [43].
-
5.
Cost-benefit
The cost of albumin is nearly 40–80 times that of a crystalloid. In a cost–benefit analysis based on the post-hoc analysis of the ALBIOS study in patients with sepsis, the number needed to treat is 16. The additional cost per life saved was $14,384 in 2017 [44].
Case Vignette
-
Q1: Which intravenous fluids will you use for further resuscitation of this patient?
-
A1: The patient is haemodynamically unstable and received 4.5 L of crystalloids for fluid resuscitation, and 20% albumin can be considered for further resuscitation if the patient continues to be haemodynamically unstable (MAP <65 mmHg) and fluid responsive.
-
Q2: What will be the end points of resuscitation?
-
A2: The end points of resuscitation can be haemodynamic end points (MAP ≥65 mmHg) or fluid tolerance. Despite fluid-responsive state, if there is evidence of global increased permeability syndrome, vasopressors should be considered early to avoid fluid accumulation.
Conclusion
Albumin is the most promising plasma expander among colloids. The evidence supports the safety of albumin as a plasma expander in patients with septic shock and post-operative cardiac surgery. Albumin has different roles in all phases of fluid management in ICU (resuscitation, stabilisation, optimisation, and deresuscitation) (Fig. 10.2). Appropriate patient selection with cost–benefit analysis may justify its use. Despite reducing the administered volume of IV fluids, the evidence on mortality outcomes is inconclusive. In the era of precision-based medicine, exogenous albumin can be considered for plasma expansion in fluid-responsive patients who have received a considerable amount of crystalloids and/or hypoalbuminemia.
Take-Home Messages
-
Both high- and low-concentration albumin solutions can be used for resuscitation if the patient continues to require fluid, despite receiving a considerable volume of crystalloids.
-
Albumin is a safe and effective plasma expander in patients with sepsis and septic shock.
-
Albumin resuscitation should be avoided in patients with traumatic brain injury.
-
Albumin is a blood product and is costlier than crystalloid. Like any other blood product, judicious and vigilant use of albumin is recommended.
-
There is no evidence to support that exogenous albumin administration contributes to oedema formation in patients with sepsis.
References
Joannidis M, Wiedermann CJ, Ostermann M. Ten myths about albumin. Intensive Care Med. 2022;48(5):602–5.
Yu YT, Liu J, Hu B, Wang RL, Yang XH, Shang XL, et al. Expert consensus on the use of human serum albumin in critically ill patients. Chin Med J. 2021;134(14):1639–54.
Franch-Arcas G. The meaning of hypoalbuminaemia in clinical practice. Clin Nutr Edinb Scotl. 2001;20:265–9.
Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM. Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg. 2003;237(3):319–34.
Malbrain MLNG, Langer T, Annane D, Gattinoni L, Elbers P, Hahn RG, et al. Intravenous fluid therapy in the perioperative and critical care setting: executive summary of the international fluid academy (IFA). Ann Intensive Care. 2020;10(1):64.
Caironi P. POINT: should intravenous albumin be used for volume resuscitation in severe sepsis/septic shock? Yes. Chest. 2016;149(6):1365–7.
Zdolsek M, Hahn RG, Zdolsek JH. Recruitment of extravascular fluid by hyperoncotic albumin. Acta Anaesthesiol Scand. 2018;62(9):1255–60.
Jacob M, Chappell D, Conzen P, Wilkes MM, Becker BF, Rehm M. Small-volume resuscitation with hyperoncotic albumin: a systematic review of randomized clinical trials. Crit Care. 2008;12(2):R34.
Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R. SAFE study investigators: a comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350(22):2247–56.
Martin GS, Bassett P. Crystalloids vs. colloids for fluid resuscitation in the intensive care unit: a systematic review and meta-analysis. J Crit Care. 2019;50:144–54.
Tseng CH, Chen TT, Wu MY, Chan MC, Shih MC, Tu YK. Resuscitation fluid types in sepsis, surgical, and trauma patients: a systematic review and sequential network meta-analyses. Crit Care. 2020;24(1):693.
Cochrane Injuries Group Albumin Reviewers. Human albumin administration in critically ill patients: systematic review of randomised controlled trials. BMJ. 1998;317(7153):235–40.
Charpentier J, Mira JP. EARSS study group: efficacy and tolerance of hyperoncotic albumin administration in septic shock patients: the EARSS study. Intensive Care Med. 2011;37(Suppl 1):S115–S0438.
Caironi P, Tognoni G, Masson S, Fumagalli R, Pesenti A, Romero M, et al. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med. 2014;370:1412–21.
SAFE Study Investigators, Finfer S, Mc Evoy S, Bellomo R, Mc Arthur C, Myburgh J, Norton R. Impact of albumin compared to saline on organ function and mortality of patients with severe sepsis. Intensive Care Med. 2011;37(1):86–96.
Patel A, Laffan MA, Waheed U, Brett SJ. Randomised trials of human albumin for adults with sepsis: systematic review and meta-analysis with trial sequential analysis of all-cause mortality. BMJ. 2014;349:g4561.
Xu JY, Chen QH, Xie JF, Pan C, Liu SQ, Huang LW, et al. Comparison of the effects of albumin and crystalloid on mortality in adult patients with severe sepsis and septic shock: a meta-analysis of randomized clinical trials. Crit Care. 2014;18(6):702.
Wiedermann CJ, Joannidis M. Albumin replacement in severe sepsis or septic shock. N Engl J Med. 2014;371:83.
Park CHL, de Almeida JP, de Oliveira GQ, Rizk SI, Fukushima JT, Nakamura RE, et al. Lactated Ringer’s versus 4% albumin on lactated ringer’s in early sepsis therapy in cancer patients: a pilot single-center randomized trial. Crit Care Med. 2019;47:e798–805.
Philips CA, Maiwall R, Sharma MK, Jindal A, Choudhury AK, Kumar G, et al. Comparison of 5% human albumin and normal saline for fluid resuscitation in sepsis induced hypotension among patients with cirrhosis (FRISC study): a randomized controlled trial. Hepatol Int. 2021;15(4):983–94.
Maiwall R, Kumar A, Pasupuleti SSR, Hidam AK, Tevethia H, Kumar G, et al. A randomized-controlled trial comparing 20% albumin to plasmalyte in patients with cirrhosis and sepsis-induced hypotension [ALPS trial]. J Hepatol. 2022;77(3):670–82.
Wigmore GJ, Anstey JR, St John A, Greaney J, Morales-Codina M, Presneill JJ, et al. 20% human albumin solution fluid bolus administration therapy in patients after cardiac surgery (the HAS FLAIR study). J Cardiothorac Vasc Anesth. 2019;33(11):2920–7.
Roberts I, Blackhall K, Alderson P, Bunn F, Schierhout G. Human albumin solution for resuscitation and volume expansion in critically ill patients. Cochrane Database Syst Rev. 2011;11:CD001208.
Annane D, Siami S, Jaber S, Martin C, Elatrous S, Declère AD, et al. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA. 2013;310:1809–17.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for Management of Sepsis and Septic Shock 2021. Crit Care Med. 2021;49(11):e1063–143.
Mårtensson J, Bihari S, Bannard-Smith J, Glassford NJ, Lloyd-Donald P, Cioccari L, et al. Small volume resuscitation with 20% albumin in intensive care: physiological effects : the SWIPE randomised clinical trial. Intensive Care Med. 2018;44(11):1797–806.
McIlroy D, Murphy D, Kasza J, Bhatia D, Wutzlhofer L, Marasco S. Effects of restricting perioperative use of intravenous chloride on kidney injury in patients undergoing cardiac surgery: the LICRA pragmatic controlled clinical trial. Intensive Care Med. 2017;43(6):795–806.
Nasa P, Wise R, Elbers PWG, Wong A, Dabrowski W, Regenmortel NV, et al. Intravenous fluid therapy in perioperative and critical care setting-knowledge test and practice: an international cross-sectional survey. J Crit Care. 2022;71:154122.
China L, Freemantle N, Forrest E, Kallis Y, Ryder SD, Wright G, et al. A randomized trial of albumin infusions in hospitalized patients with cirrhosis. N Engl J Med. 2021;384:808–17.
Caraceni P, Riggio O, Angeli P, Alessandria C, Neri S, Foschi FG, et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial. Lancet. 2018;391:2417–29.
Kütting F, Schubert J, Franklin J, Bowe A, Hoffmann V, Demir M, et al. Insufficient evidence of benefit regarding mortality due to albumin substitution in HCC-free cirrhotic patients undergoing large volume paracentesis. J Gastroenterol Hepatol. 2017;32:327–38.
Benmassaoud A, Freeman SC, Roccarina D, Plaz Torres MC, Sutton AJ, Cooper NJ, et al. Treatment for ascites in adults with decompensated liver cirrhosis: a network meta-analysis. Cochrane Database Syst Rev. 2020;1:CD013123.
Best LM, Freeman SC, Sutton AJ, Cooper NJ, Tng EL, Csenar M, et al. Treatment for hepatorenal syndrome in people with decompensated liver cirrhosis: a network meta-analysis. Cochrane Database Syst Rev. 2019;9:CD013103.
Salerno F, Navickis RJ, Wilkes MM. Albumin infusion improves outcomes of patients with spontaneous bacterial peritonitis: a meta-analysis of randomized trials. Clin Gastroenterol Hepatol. 2013;11(2):123–30.e1.
Salman TA, Edrees AM, El-Said HH, El-Abd OL, El-Azab GI. Effect of different therapeutic modalities on systemic, renal, and hepatic hemodynamics and short-term outcomes in cirrhotic patients with spontaneous bacterial peritonitis. Eur J Gastroenterol Hepatol. 2016;28(7):777–85.
Dubois MJ, Orellana-Jimenez C, Melot C, De Backer D, Berre J, Leeman M, et al. Albumin administration improves organ function in critically ill hypoalbuminemic patients: a prospective, randomized, controlled, pilot study. Crit Care Med. 2006;34(10):2536–40.
Oh SW, Han SY. Loop diuretics in clinical practice. Electrolyte Blood Press. 2015;13:17–21.
Cordemans C, De Laet I, Van Regenmortel N, Schoonheydt K, Dits H, Martin G, et al. Aiming for a negative fluid balance in patients with acute lung injury and increased intra-abdominal pressure: a pilot study looking at the effects of PAL-treatment. Ann Intensive Care. 2012;2(Suppl 1):S15.
Martin GS, Moss M, Wheeler AP, Mealer M, Morris JA, Bernard GR. A randomized, controlled trial of furosemide with or without albumin in hypoproteinemic patients with acute lung injury. Crit Care Med. 2005;33(8):1681–7.
SAFE Study Investigators, Australian and New Zealand Intensive Care Society clinical trials group, Australian red cross blood service, George Institute for International Health, Myburgh J, Cooper DJ, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874–84.
Cooper DJ, Myburgh J, Heritier S, Finfer S, Bellomo R, Billot L, et al. Albumin resuscitation for traumatic brain injury: is intracranial hypertension the cause of increased mortality? J Neurotrauma. 2013;30(7):512–8.
Melia D, Post B. Human albumin solutions in intensive care: a review. J Intensive Care Soc. 2021;22(3):248–54.
Coz Yataco AO, Flannery AH, Simpson SQ. Counterpoint: should intravenous albumin be used for volume resuscitation in severe sepsis/septic shock? No. Chest. 2016;149(6):1368–70.
Joint Formulary Committee. British national formulary. 79th ed. London: BMJ Group and Pharmaceutical Press; 2020.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Nasa, P., Kumar, R., Juneja, D., Gosh, S. (2024). The Case for Albumin as Volume Expander and beyond. In: Malbrain, M.L., Wong, A., Nasa, P., Ghosh, S. (eds) Rational Use of Intravenous Fluids in Critically Ill Patients. Springer, Cham. https://doi.org/10.1007/978-3-031-42205-8_10
Download citation
DOI: https://doi.org/10.1007/978-3-031-42205-8_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-42204-1
Online ISBN: 978-3-031-42205-8
eBook Packages: MedicineMedicine (R0)