Abstract
We highlight the causal effect of energy poverty on health in France. After collecting original data from 5000 individuals, we first statistically study the correlations between different pathologies and different aspects of energy poverty. Then, using econometric models, we quantify the causal effect of energy poverty on physical health and mental health scores, and also on the risk of occurrence of certain pathologies. Our data show a significant difference in health status between energy-poor individuals and energy-sufficient individuals. Results confirm that falling into energy poverty significantly degrades health scores. Being in energy poverty reduces the World Health Organization’s (WHO) physical health score by 8.14 points. The negative and significant effect on the mental health indicator is 3.78 points. When individuals are in a situation of energy poverty, their self-assessed health scores are on average 3.37 points lower than individuals who are not energy insecure. In addition, individuals living in dwellings with poor roof insulation, humidity, or mold suffer more frequently from chronic disease or psychological distress. Finally, it appears that reducing energy poverty by 1% would save about EUR 476 million. Regarding mental disorders, this could rise to EUR 10.6 million.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
1 Introduction
The COVID-19 health crisis has revealed the vulnerability of a part of the population and has brought to the forefront the need to act collectively to address global challenges. Among these challenges are of course the protection of human health, but also the preservation of resources and the mitigation of climate change. Protecting and improving health and mitigation of climate change therefore have a shared agenda. Combating energy poverty is one of the pillars of public action to address global warming, but also to promote the well-being and health of those who live in inefficient housing.
Many studies have established the impact of poor housing on the health of inhabitants. For example, low temperatures over time are associated with increased cardiovascular and respiratory problems, the latter being even more pronounced among children (Platt et al. 1989; Peat et al. 1998; Maidment et al. 2014). They can also aggravate existing health problems, such as arthritis or rheumatism, and weaken the immune system to the point of causing minor but recurrent disorders such as colds or flu (Oliveras et al. 2021). Dampness and mold are also harmful to health as they cause respiratory problems and asthma (Dales et al. 1991; Peat et al. 1998; Jaakkola et al. 2005). When housing is of poor quality, it may even contain substances that are harmful to health. This is particularly the case with radon, or with formaldehyde from combustion or off-gassing which increases the risk of cancer (Braubach et al. 2011). Various channels have also been identified as potential drivers of mental health. For example, cold weather can force people to adopt behaviors such as wearing coats indoors, sleeping with pets, or living in one room only. These behaviors create a sense of shame and isolate individuals (Anderson et al. 2012). Social isolation is recognized as an antecedent of anxiety and depression. At the same time, the fear of not being able to pay energy bills also generates stress and anxiety in households suffering from poor housing conditions (Liddell and Morris 2010).
Beyond housing quality, the fear of not being able to pay energy bills shows that there is a wider economic issue, that of energy poverty. Energy poverty covers three dimensions including poor housing, the negative effects of which on health have been widely reported, economic insecurity due to low income, and vulnerability to energy price rises. These three dimensions are closely linked and convey a reality beyond poor housing. Each contributes to the other and thus makes energy poverty a material, economic and social situation from which it is difficult to escape.
The aim of this chapter is first to analyze the strong statistical link between the prevalence of several illnesses, both physical and mental, and energy poverty in France in 2020, and second to discuss the health benefits that could be expected from combating energy poverty effectively.
To achieve the objectives mentioned above, we built a rich and original database. The data was collected in France in October 2020. We used a sample of 5000 individuals representative of the French population, containing socio-demographic information on the household, housing and energy consumption, access to the labor market, transportation habits, and reported health. In particular, it includes the World Health Organization quality of life questionnaire (WHOqol), making it possible to compute different health scores. We also gathered information on a range of pathologies and symptoms such as coughing, asthma, rheumatism, chronic diseases, and so on.
Our data clearly show a significant difference in the health status between energy-poor individuals and others. The descriptive approach allows us to confirm that individuals living in poor-quality housing (inadequate roof insulation, presence of humidity or mold, etc.) suffer more frequently from respiratory pathologies or psychological distress. This results in lower physical and mental health scores. The use of econometric models controlling for unobserved heterogeneity potentially affecting health status and energy poverty simultaneously, and also controlling for a number of other characteristics with an impact on health status, clearly confirms that all other things being equal, falling into energy poverty significantly degrades objective physical and mental health scores, but also self-reported and subjective health.
Our work highlights the health aspects that are adversely affected by energy poverty, but also each of the dimensions from the literature. Thus, whether health is measured objectively or subjectively, whether we focus on specific pathologies, whether we estimate the impact of a binary indicator of energy poverty or a specific aspect of this type of precariousness, all our results converge. In addition, being in energy poverty leads to consuming more health services. Our results show that tackling energy poverty is therefore of the utmost importance in addressing social inequality and in mitigating climate change, but effective policies in this area can also lead to substantial savings in health spending.
The chapter is organized as follows. Section 2 is dedicated to the state of the art on the link between energy poverty and health. The third section presents our recent and original database. In Sect. 4 we discuss the empirical analysis. The results and the discussion are presented in Sect. 5, and Sect. 6 concludes.
2 The State of Knowledge on the Link between Energy Poverty and Population Health
In recent years, the literature has taken up public health issues related to energy poverty. This has resulted in several types of scientific research, beginning with timely and localized studies highlighting the direct impact of renovation, housing rehabilitation programs, or energy efficiency on health (Howden-Chapman et al. 2007; Lloyd et al. 2008; Chapman et al. 2009; Ezratty et al. 2009; Thomson and Snell 2013). Health is sometimes only an indirect outcome of this research which has been more focused on indoor temperature (Pollard et al. 2019), indoor air quality (Rosenow and Galvin 2013), or energy consumption (Rosenow and Galvin 2013; Webber et al. 2015; Grimes et al. 2016).
Part of the existing academic literature also makes it possible to establish a direct causal relationship between energy poverty and health (Liddell and Morris 2010; Lacroix and Chaton 2015; Chaton and Lacroix 2018; Charlier and Legendre 2022) in the absence of specific initiatives such as renovations or public policy. This type of non-experimental research has the advantage of employing suitable tools to control several biases inherent to this question, such as the simultaneous effect of unobservable attributes on health and the risk of energy poverty, or a reverse causality between energy poverty and health. Using instrumental approaches or panel data methodologies for example makes it possible to resolve such problems. In a few studies, the use of panel data also made it possible to consider climate risks and the path dependency of health in the analysis (Charlier and Legendre 2022).
Although not all European countries have adopted an official definition of energy poverty, there nevertheless seems to be a consensus on the constituent dimensions of this type of precariousness: the energy insecure face a problem of low income, have poor quality, energy-inefficient housing, and have difficulty coping with energy costs (European Fuel Poverty and Energy 2006; Devalière 2007; Palmer et al. 2008; Liddell and Morris 2010; Charlier and Legendre 2018). This results in cold homes in winter, moisture problems when homes are poorly insulated, and difficulty paying energy bills. The effect of each of these problems on health has been documented.
2.1 The Effect of Cold on Health
The World Health Organization has established that the indoor temperature of homes should not fall below 18 degrees to protect the health of populations in general. When temperatures remain permanently below this threshold, inhabitants may face respiratory infections, cardiovascular troubles, increased blood pressure, or degradation of existing diseases such as arthritis. An equally established consequence is the increased risk of household accidents within the home. A number of studies confirm this. For example, in Ireland, the installation of central heating systems and the improvement of awareness about energy efficiency have led to a significant decrease in the number of households reporting arthritis/rheumatism and other forms of disease (Shortt and Rugkåsa 2007). The installation of central heating in detached or semi-detached houses would also reduce night cough, childhood asthma, and thus reduce school absenteeism (Barton et al. 2007).
If the temperature in a dwelling affects physical health, the same is true for mental health. Indeed, (O’Brien et al. 2011) have shown that insufficient heat in housing has an impact on mental health, emotional well-being, or social isolation. At the root of some of these disorders, we find a number of behaviors to cope with the cold which can isolate individuals, in particular due to a sense of shame. These behaviors affect well-being and mental health (Anderson et al. 2012). Indeed, individuals are forced for example to heat only one room, or to wear coats indoors, or even to sleep with pets to get warmer. This leads to the social isolation described by Hills (2012).
2.2 The Effect of Moisture on Health
Humidity is a problem often found in households in energy poverty, and which remains closely linked to the cold. It appears that the humidity of insufficiently heated dwellings can cause stress and depression (Lowry 1991; Khanom 2000; Shortt and Rugkåsa 2007). Mold can accumulate in cold, damp homes, causing respiratory symptoms, including asthma, coughing, and wheezing (Dales et al. 1991; Peat et al. 1998; Jaakkola et al. 2005). Fisk et al. (2007) concluded from a meta-analysis that moisture and mold are associated with a 30–50% increase in respiratory tract and asthma-related health problems.
2.3 The Effect of Financial Pressure on Health
The monetary dimension of energy poverty relates to the lack of income needed to pay energy bills, whether due to the physical characteristics of the housing as mentioned in the previous paragraphs, or the excessively high cost of energy. The existence of arrears in the payment of energy bills is a variable often analyzed by the European Commission in its work on energy poverty. Households who fear that unpaid bills will accumulate or fear that they will not be able to pay them are under increased stress. Moreover, this stress is a breeding ground for the development of anxiety and depression. More broadly, financial pressure is a source of mental distress (Liddell and Morris 2010).
People in energy poverty may experience embarrassment and shame (Longhurst and Hargreaves 2019). What Longhurst and Hargreaves (2019) call emotions is also described in their qualitative survey as a premise of social isolation. The feeling of failure takes a heavy toll on emotional and mental health, whether faced with financial hardship, the threat of job loss, or the threat of suspension of electricity and other energy services.
3 Data
3.1 The PEPSI Database
A rich and original database, representative of the French population,Footnote 1 was built to assess the question of energy poverty on physical and psychological health. The PEPSIFootnote 2 data were collected in October 2020, i.e., five months after the end of the first pandemic containment measures in France, and about three weeks before the second set of measures. After removing some aberrant observations, the final sample contains 4,194 individuals and remains representative of the French population. Our analysis focuses on individuals, but we also have some information about their households, enabling us to calculate the standard of living within the household, for example.
The survey consists of 302 questions divided into six modules, allowing for a detailed description of individuals and households to which they belong including socio-demographic, health, housing, transport and labor market characteristics, and energy expenditures. Questions to establish the World Health Organization (WHO) Profile are asked in the health module. The World Health Organization quality of life questionnaire (WHOQOL BREF questionnaire) calculates two health scores: a physical health score and a mental health score. The individual has a choice of five responses per question and accumulates more or fewer points depending on the response (very unwell- 1 point to very well- 5 points). To calculate the physical health score, the individual answers seven questions and the points for each response are added to obtain a raw score. Then, to convert it to 100, we refer to the points conversion table provided in the guide. For the psychological health score, the procedure is almost identical except that the individual answers only six questions more focused on their mental well-being.Footnote 3 Values range from 0 (for the worst scores) to 100 for the maximum score. Other variables can be used to assess health status. Dichotomous variables, on the existence of diseases (chronic, respiratory, cardiovascular, rheumatism, psychological, and headache), can be used as a control. These variables also make it possible to better understand what the impact of energy poverty is in terms of pathologies. A variable for a perceived health score and the number of visits to the doctor has been used.
We adopt the definition of the French Observatory on Energy Poverty (Observatoire National de la Précarité Énergétique) for energy poverty, which considers energy poverty to be a threshold of 8% in the energy-income ratio for the first three income deciles.Footnote 4 The first three deciles are determined by equivalizing the reference tax income of the household.Footnote 5 Then, to calculate the energy-income ratio, the annual amount of the total energy bill for all uses and the reference tax income of the household to which the individual belongs is used. These elements allow calculation of the energy-income ratio, which determines the share of income spent on energy. By selecting the poorest 30% of individuals in the sample who have an energy-income ratio higher than 8%, we can build the binary variable of energy poverty Energy Poor (0 = not energy poor, 1 = energy poor). To ensure the robustness of our results, we also compared our results with each dimension of energy poverty. Energy poverty is a convergence of three main elements: household income, household energy requirements, or energy efficiency of homes and fuel prices which influence self-restriction behaviors (Boardman 1991; Hills 2012). Thus, qualitative variables to measure housing quality (quality of roof insulation, quality of wall insulation, and presence of moisture) are also considered.
We calculated the level of income poverty to compare our results. Poor households are those whose income equivalent is below 60% of the median. Finally, we introduced additional variables for controlling for health status: socio-demographic characteristics (age, employment status, gender, children, etc.), physical attributes (physical activity, height, and weight), and local conditions (weather).
The relationship between socioeconomic characteristics and health is well-established. Negative health behaviors and psychosocial characteristics are clustered in socioeconomic status groups, often measured by low income (Lynch et al. 1997; Benzeval and Judge 2001; Contoyannis et al. 2004) or by gender (Vlassoff 2007). Older people are also often in poor health (Ohrnberger et al. 2017) and having a caregiving role has a markedly negative impact on physical and mental health scores (Hegewald et al. 2020; Parra-Saavedra and Miranda 2021). Health status is also related to retirement status (Sickles and Taubman 1986) as well as employment conditions (Barnay and Defebvre 2021). Other health controls have been introduced such as the number of psychologists in the region, to take into account access to health care (Charlier and Legendre 2022), and having contracted COVID-19. On the other hand, being physically active prevents the deterioration of physical and mental health (Maller et al. 2009; Pelletier et al. 2017; Fossati et al. 2021). Telecommuting can generate stress, as people are more likely to be overworked and have difficulty separating their work from their private life (Dimitrova 2003; Mann 2003). Plus, being alone at home without social relationships and isolated can lead to a number of psychological problems such as loneliness and depression (Tavares 2017). Finally, information about location is available in the database. This was matched with meteorological data of Meteo France (unified degree daysFootnote 6) to provide a proxy for actual meteorological conditions and to obtain unified degree days.
3.2 Descriptive Statistics
The main descriptive statistics are presented in Tables 1 and 2. On average, the physical health score stands at 67 points while the mental health score is slightly lower, at 63 points. The self-assessed health rating (71.8) is quite close to the score measured by the World Health Organization. Individuals consult the doctor 1.5 times a year for seasonal diseases. Nevertheless, there is a high degree of heterogeneity among individuals in terms of health since the minimum is generally around 0 and the maximum is equal to 100. About 10% of respondents report respiratory pathologies and 50% chronic pathologies. Cardiovascular problems affect 14.8% of the individuals in the sample, headaches 12.4%, and rheumatism 14.7%. About 7% of respondents report having a mental health disorder. Some 90% of individuals have a referring doctor. Generally speaking, health scores are quite correlated.
Regarding housing conditions, 11% of individuals report mold problems, on the other hand, 60% report good roof insulation and 57% good wall insulation. The average reference tax income is EUR 33,142 and 12.8% can be considered energy poor. Housing quality is correlated with health similar to the correlation between income and health scores (around 0.20). The correlation coefficient between being energy poor and physical and mental health is positive and around 0.14.
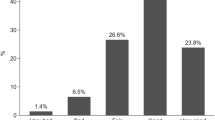
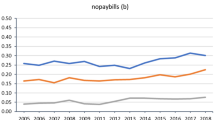
By conducting tests of means comparison between the chronic pathologies reported by individuals, and housing conditions (poor insulation, mold), we see that the difference in the presence of certain pathologies is significant (Table 3). Indeed, individuals reporting problems in housing conditions also report chronic diseases, respiratory diseases, migraines, and psychological problems more often. This observation is confirmed when we look at the differences in health scores and the number of doctor visits (Table 4). These results also translate into being energy poor and monetary poor. We also look at heating restriction behaviorsFootnote 7 which can be one of the manifestations of energy poverty. Again, households reporting restriction behavior have on average more pathologies and lower health scores. Looking at Figs. 1 and 2, these results are confirmed for the number of doctor visits and energy poverty. Energy-poor people visit the doctor more per year on average.Footnote 8 The energy poor are also more likely to report chronic disease (57% against 49%). This results in different reported and measured health scores across population groups (Fig. 3).
4 Model
In this chapter, we assess the impact of energy poverty (EP) and housing conditions on physical and mental health scores (HEALTH) controlling for potential endogeneity more specifically due to unobserved elements that affect EP and health simultaneously (Kahouli 2020; Awaworyi Churchill and Smyth 2021; Charlier and Legendre 2022). Controls for individual characteristicsFootnote 9 (X) and climate measured by Unified degree days (C) are introduced. ProofsFootnote 10 of the robustness are available in Appendix A.2. Thus, we estimate for different health scores (physical, psychological, self-reported, and number of visits to the doctor):
i = 1, …, n
where H, the individual health status, is measured using different indicators (WHO scores, health self-assessment, and number of visits to a primary care physician), Xi the vector of individual characteristics, Ci the climate control (unified degree days), and \(\widehat{{EP_{i} }}\), the estimated value of energy poverty indicating if individual i is energy poor determined as follows:
with COOK (electricity for cooking), ALTITUDE (the altitude at which the dwelling is located), and VOUCHER (when an individual benefits from financial support for energy costs) used as instrumental variables. Indeed, we need exclusion variables that directly explain energy poverty but not health scores (both physical and mental).
Altitude at which the dwelling is located seems perfectly exogenous, and intuitively nothing leads us to believe that altitude can affect health scores, yet it is expected to influence energy needs for heating through the numerator of the energy-income ratio (Katsoulakos and Kaliampakos 2014; Li et al. 2022). Energy cost is also dependent on the quality of building insulation and the energy source. One way to deal with this is to introduce the energy source for cooking (COOK): fuel source and efficiency of appliances during cooking can affect energy use (Hager and Morawicki 2013).
Finally, it is necessary to control for budget (the denominator of the energy-income ratio). French households can benefit from income-based financial support, which directly increases their income level and can decrease the burden of energy expenditures (Hancevic and Sandoval 2022). This subsidy is available to all households whatever the energy source. Only 42% of the energy poor in our dataset benefit from this financial support. We then introduce the instrument VOUCHER in (2). Additional regressions also can be provided to explain the occurrence of different pathologies namely chronic, cardiovascular, respiratory, rheumatic, headache, and psychological diseases, in this case we have the following specification:
where Di is the pathology.
Equations (1) and (2) are estimated simultaneously using a conditional mixed-process (CMP) (Roodman 2011). One main advantage of a CMP is the ability to deal with the different nature of the dependent variable. Conditional mixed-process is employed to estimate simultaneous equations where instruments allow the construction of a recursive set of equations, as in two-stage least squares (2SLS). As energy poverty (Eq. 2) is not a continuous variable, standard IV methods can lead to misspecification. The CMP enables consideration of the binary nature of the variable. The model allows us to jointly estimate a binary variable and a continuous variable. In our case, Eq. (1) is estimated as an OLS, so coefficients can be directly interpreted as margins and in Eq. (2) we interpret only the sign of coefficients and their significance. It is possible to jointly estimate Eqs. (2) and (3). In this case, we have two probits and we only interpret the sign of coefficients and their significance.
In order to provide additional elements, we will also look at the dimensions of energy poverty to explain health scores and the occurrence of pathologies. For this, we will study the impact of the different dimensions (heating restriction, income, quality of the dwelling measured by moisture problems, or quality of roof and wall insulation) measured by vector Z on health scores: physical, psychological, self-reported, and number of visits to the doctor on one hand:
and on the probability of developing chronic, cardiovascular, respiratory, rheumatic, headache, and psychological diseases on the other hand:
In these last two cases, Eq. (3) is a simple OLS and Eq. (4) is a probit.
5 Results and Discussion
5.1 The Effects of Energy Poverty on Health
Our estimates clearly show that energy poverty affects health (Table 5). The estimate of Eq. (2) is reported in the Appendix (Table A.1). The results remain valid whatever the method of capturing the health status (objective health scale, subjective rating, proxy such as doctor visits), and whatever the variables used to measure energy poverty. Whether we use being fuel poor or the energy effort rate directly, our results converge. Being in energy poverty thus reduces the WHO physical health score by 8.14 points. The negative and significant effect on the mental health indicator is 3.78 points. When individuals are in a situation of energy poverty, they also give themselves a lower health score on average (3.37 points lower than the score reported by individuals who are not energy poor). Finally, this poor health consistently translates into increased care consumption, since people in a situation of energy poverty report 2.23 more visits to the doctor on average than others.
In Table 5, we show that several vulnerability factors have an impact on health. Thus, it appears that being a student, retired or unemployed negatively affects physical health scores. The strongest impact corresponds to being unemployed (−6.7 points), followed by being a student (−4 points), and being retired (−3.9 points). Our results also control for the supply of care to populations, since the medical density is integrated (number of psychologists in the region). Increasing the supply of psychologist services improves the mental health score.
Table 6 allows us to delve a little deeper into different dimensions of energy poverty. For comparison purposes, we directly compare our results with a traditional OLS model in which the variable of interest, energy poverty, has been replaced by variables describing energy poverty, namely income, heating restrictions, dampness in the dwelling, and having good quality wall and roof insulation. The results show that insufficient income is not the only cause of deteriorating health. Certainly, the higher the income, the better the objective and subjective health scores, and the less individuals visit the doctor. But this analysis in terms of living standards is far from sufficient. Indeed, each of the variables qualifying the energy efficiency of housing is also statistically significant, just as the variable capturing the restriction is statistically significant for objective health scores.
Thus, having good isolation improves objective mental and physical health scores from 2.6 to 3.9 points. It appears that people living in well-insulated housing feel the benefits since their self-reported score is also higher. The problem of humidity seems to lead to a substantial deterioration in subjective health since the score reported by those concerned is on average 4.22 points lower while the negative effect on the objective scores of physical and mental health are lower by 2.83 and 3.09 points, respectively.
Now we can also look the relationship between being energy poor and the type of pathology in more detail (Table 7). We note that being energy poor increases the likelihood of developing chronic, respiratory, and psychological diseases. But energy poverty is not significant in explaining cardiovascular problems, rheumatism, or headaches (Table 7).
On closer examination, the impact of the dimensions of energy poverty on the different pathologies (Table 8) shows that all the dimensions of energy poverty have an impact on chronic diseases, which means that suffering from a chronic disease is not only a problem of income. It is even shown that the most important marginal effect on the probability of suffering from chronic diseases is related to the presence of humidity in the dwelling followed by heating restriction (11.61% and 7.9%, respectively). Combined cold and humidity are therefore the two factors responsible for this type of pathology. For rheumatism-related pathologies, once again, the marginal effect is stronger for humidity (5.2%) than for an increase in income (-1.4%). Heating restriction increases the probability of suffering from psychological diseases by 24.8%.
Additionally, if we were to prioritize a type of renovation to address health pathologies, we would have to focus on roof insulation, which seems to have more of an impact on the reduction of chronic, cardiovascular, or respiratory diseases. Wall insulation plays a significant role in rheumatism-related problems and psychological problems.
5.2 Policy Recommendations
Our results suggest the importance of tackling energy poverty in reducing the direct and indirect health costs it generates. There is little research estimating the health costs associated with energy poverty. Only a few countries have already addressed the issue. Existing work generally does not make it possible to form a link between energy poverty and health, but more precisely between poor housing and health. Indeed, it seems easier to link observable physical characteristics of housing to the development of pathologies and disorders than to assess a monetary effect whose causality is demonstrated only due to non-experimental studies. When such analysis does exist, it is often informed by work originating in the United Kingdom, which is a pioneer in tackling energy poverty. As early as 1996, the Housing Health and Safety Rating System (HHSRS) method was developed in England. It makes it possible to calculate an indicator of the health risk suffered by the occupants of a dwelling based on its physical characteristics. In its latest report in 2021, the Building Research Establishment concluded that poor housing conditions in England cost the country £1.4 billion each year to treat the affected population. Direct costs include the medical treatment of illnesses that are more prevalent in poor housing situations, and even more so in winter, and more frequent domestic accidents. Indirect costs cover a much wider spectrum, ranging from the persistence of certain pathologies over time to social costs. Moreover, the increase in the prevalence of certain pathologies and the frequency of accidents leads to work stoppages and school absenteeism, which in turn results in a loss of productivity and economic potential in the medium and long term. The total estimated societal cost reaches £ 18.5 billion each year.
By applying our results, it is possible to make a comparative analysis of the direct costs and benefits of a few measures for the French case. In France, there are 30 million primary residences in 2022 (homes, apartments) for 67 million people (Source: INSEE). The total health cost for chronic disease and psychological disease is EUR 104 billion and EUR 23.3 billion each year, respectively. If the roofs of all homes were renovated for example,Footnote 11 France could expect to save EUR 36.4 million related to chronic disease over a year (104 billion multiplied by −0.0325%, the coefficient in Table 8).
Humidity could be addressed by equipping all homes with mechanical ventilation, resulting in a potential savings of EUR 120 million in spending on chronic diseases alone (+0.1161% multiplied by 104 billion) for a total investment of EUR 58.5 billion.Footnote 12 It would also save EUR 4.82 million for mental health spending (+0.0207% % multiplied by 23.3 billion). A measure that would consist of increasing income by EUR 331, i.e., 10% of the average income (the energy subsidy to help the poorest households is at most equal to EUR 277), would lead to health-related savings (chronic diseases and mental health problems) of about EUR 60.1 million (+ 0.079% multiplied by 104 billion and +0.248% multiplied by 23.3 billion; see Table 8 for percentages). In the end, being energy poor increases the probability of developing a chronic disease by 0.458%, which could represent a cost of EUR 476 million (0.458% multiplied by EUR 104 billion; see Table 7 for percentages), and an additional cost for health pathologies of EUR 10.6 million (+0.464% multiplied by EUR 23.3 billion; see Table 7 for percentages). Restricting one’s energy consumption would entail a total additional cost of about EUR 140 million (0.079% multiplied by 104 billion so 82.16 million plus 0.248% multiplied by EUR 23.3 billion so 57.7 million; see Table 8 for percentages). In addition to the results obtained in the study, a Eurofound study focusing on nine types of housing problems established that 2.5 million homes in France have low indoor temperatures, or 9.1% of all private housing. The Housing Health and Safety Rating System (HHRS) method was then employed to identify the health cost related to these cold temperatures. The average health cost associated with the cold would be EUR 726 per dwelling, but EUR 33 would be direct costs related to care. In other words, cold housing in France would cost EUR 1.85 billion per year for health care, of which EUR 84.7 million would be linked to direct spending. The health studies department of Electricité de France (EDF) has estimated that the health costs related to low temperatures in housing would be EUR 639 million (Ezratty et al. 2017).
6 Conclusions
The academic and institutional literature, and also the work of practitioners, has extensively explored the determinants of energy poverty and evaluated the various measures to combat the phenomenon. Other issues have emerged which are much broader than those related to the comfort within housing and the fight against social inequality. Indeed, the COVID-19 health crisis has significantly strengthened the belief that it is necessary to preserve global public goods such as public health. In recent years, considerable work on energy poverty has highlighted the multiple and indirect challenges of the fight against the phenomenon. While many ad hoc and local experiments have established clear links between poor housing and poor health, there is still little non-experimental work in the general population, to make it possible to highlight the causal effects of energy poverty on health, evaluated quantitatively, and objectively, or subjectively. Accordingly, we have used the World Health Organization mental health indicators, as well as the self-reported health ratings of respondents. The richness of our database also enables us to look at the impact on the incidence of certain pathologies in more detail.
The implementation of econometric models clearly confirms that falling into energy poverty significantly degrades objective and subjective health scores. Being in energy poverty thus reduces the WHO physical health score by 8.14 points. The negative and significant effect on the mental health indicator is 3.78 points. When individuals are in a situation of energy poverty, they also give themselves a lower health score on average: 3.37 points lower than the score reported by individuals who are not energy insecure.
In other words, these results show that at the national level, and not just at the level of a specific region, positive spillover effects can be expected from a reduction in energy poverty. Knowing the cost and index of chronic diseases in France, it appears that reducing energy poverty by 1% would save about EUR 476 million each year. Regarding mental disorders, this savings could rise to 10.6 million. It is therefore time to consider the environmental, social, and health issues of the fight against energy poverty simultaneously.
Notes
- 1.
The survey is representative of the French population based on the following criteria: sex, age, professional category, region, housing type (individual home or multiple occupancy housing), and homeownership. Proof of the representativeness of the sample can be provided on request.
- 2.
PEPSI is the acronym for the Energy Poverty, Pollution, and Individual Health project (Précarité Energétique, Pollution et Santé des Individus in French) and financed by the region Auvergne–Rhône Alpes.
- 3.
For more details, please consult the WHO website: https://www.who.int/tools/whoqol/whoqol-bref.
- 4.
Excluding households above the first three income deciles excludes those with a high income who choose to consume more energy but who have the means to finance it without any hardship.
- 5.
The OECD equivalence scale is used.
- 6.
Unified Degree Days express the severity of cold weather in a specific time period taking into consideration actual outdoor temperature and an average reference temperature previously recorded.
- 7.
Restrictive behavior is self-reported. Respondents answer the following question: Do you ever restrict heating for cost reasons?
- 8.
For information, all individuals in France benefit from health coverage, regardless of their employment status or income level.
- 9.
Age, number of children, female, single, retired, student, unemployed, telecommuting, height, weight, number of psychologists, primary care physician, COVID, tenant, caregiving role, physical activity.
- 10.
First, we conducted correlation tests, significance tests, and a Wald test to validate the instruments in the endogenous estimate. Then, to demonstrate the validity and exogeneity of instruments, different statistical tests were carried out such as F statistics, Stock and Yogo tests for weak instruments, and the Hansen J test (Lewbel 2012). To ensure the robustness of our results, we used the energy-income ratio instead of the variable for energy poverty. Finally, estimates were F controlled with simple OLS regression. The instruments were implemented directly in the main Eq. (1) to demonstrate the absence of significance directly on health scores.
- 11.
The total cost of such a measure is equal to EUR 245 billion. This figure is the result of the following calculus: the average cost of roof renovation multiplied by dwellings with poor roof insulation, so EUR 20000 (Source Effy) × 0.409 × 30,000,000). The number of dwellings with poor roof insulation is deduced from descriptive statistics, i.e., Table 1.
- 12.
Cost of mechanical ventilation is EUR 4500 (Souce: Effy) multiplied by the share of dwellings with moisture, based on Table 1 for the total housing stock (0.566 × 30,000,000).
References
Anderson C, Kraus MW, Galinsky AD, Keltner D (2012) The local-ladder effect: social status and subjective well-being. Psychol Sci 23:764–771. https://doi.org/10.1177/0956797611434537
Awaworyi Churchill S, Smyth R (2021) Energy poverty and health: panel data evidence from Australia. Energy Econ 97:105219. https://doi.org/10.1016/j.eneco.2021.105219
Barnay T, Defebvre E (2021) Retired at last? Past working conditions and the role of retirement in health status. Ann Econ Stat:39–74. https://doi.org/10.15609/annaeconstat2009.144.0039
Barton A, Basham M, Foy C et al (2007) The Watcombe Housing Study: the short term effect of improving housing conditions on the health of residents. J Epidemiol Community Health 61:771–777. https://doi.org/10.1136/jech.2006.048462
Benzeval M, Judge K (2001) Income and health: the time dimension. Soc Sci Med 52:1371–1390. https://doi.org/10.1016/s0277-9536(00)00244-6
Boardman B (1991) Fuel poverty: from cold homes to affordable warmth
Braubach M, Jacobs DE, Ormandy D (2011) Environmental burden of disease associated with inadequate housing: a method guide to the quantification of health effects of selected housing risks in the WHO European Region. World Health Organization, Regional Office for Europe
Chapman R, Howden-Chapman P, Viggers H et al (2009) Retrofitting houses with insulation: a cost–benefit analysis of a randomised community trial. J Epidemiol Community Health 63:271–277. https://doi.org/10.1136/jech.2007.070037
Charlier D, Legendre B (2022) Fuel poverty and health: a shared agenda for policy. Revue D’économie Politique 132:245–272. https://doi.org/10.3917/redp.322.0245
Charlier D, Legendre B (2018) A multidimensional approach to measuring fuel poverty
Chaton C, Lacroix E (2018) Does France have a fuel poverty trap? Energy Policy 113:258–268. https://doi.org/10.1016/j.enpol.2017.10.052
Contoyannis P, Jones AM, Rice N (2004) The dynamics of health in the British Household Panel Survey. J Appl Economet 19:473–503. https://doi.org/10.1002/jae.755
Dales RE, Zwanenburg H, Burnett R, Franklin CA (1991) Respiratory health effects of home dampness and molds among canadian children. Am J Epidemiol 134:196–203. https://doi.org/10.1093/oxfordjournals.aje.a116072
Devalière I (2007) Comment prévenir la précarité énergétique ? Situation actuelle et risques inhérents à la libéralisation du service de l’énergie. Les Annales De La Recherche Urbaine 103:137–143. https://doi.org/10.3406/aru.2007.2723
Dimitrova D (2003) Controlling teleworkers: supervision and flexibility revisited. N Technol Work Employ 18:181–195. https://doi.org/10.1111/1468-005X.00120
European Fuel Poverty and Energy (2006)
Ezratty V, Duburcq A, Emery C, Lambrozo J (2009) Liens entre l’efficacité énergétique du logement et la santé des résidents : résultats de l’étude européenne LARES. Environnement, Risques & Santé 8:497–506. https://doi.org/10.1684/ers.2009.0303
Ezratty V, Ormandy D, Laurent M-H et al (2017) Fuel poverty in France: adapting an English methodology to assess the health cost implications. Indoor and Built Environment 26:999–1008. https://doi.org/10.1177/1420326X17710808
Fisk WJ, Lei-Gomez Q, Mendell MJ (2007) Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air 17:284–296. https://doi.org/10.1111/j.1600-0668.2007.00475.x
Fossati C, Torre G, Vasta S et al (2021) Physical exercise and mental health: the routes of a reciprocal relation. Int J Environ Res Public Health 18:12364. https://doi.org/10.3390/ijerph182312364
Grimes A, Preval N, Young C et al (2016) Does retrofitted insulation reduce household energy use? Theory Pract EJ 37:165–186. https://doi.org/10.5547/01956574.37.4.agri
Hager TJ, Morawicki R (2013) Energy consumption during cooking in the residential sector of developed nations: a review. Food Policy 40:54–63. https://doi.org/10.1016/j.foodpol.2013.02.003
Hancevic PI, Sandoval HH (2022) Low-income energy efficiency programs and energy consumption. J Environ Econ Manag 113:102656. https://doi.org/10.1016/j.jeem.2022.102656
Hegewald J, Schubert M, Freiberg A, al, (2020) Traffic noise and mental health: a systematic review and meta-analysis. Int J Environ Res Public Health 17:6175. https://doi.org/10.3390/ijerph17176175
Hills J (2012) Getting the measure of fuel poverty: final report of the Fuel Poverty Review
Howden-Chapman P, Phipps R, Cunningham M (2007) Warmer houses reduce children’s asthma. Build August/september 2007:40–41
Jaakkola JJK, Hwang B-F, Jaakkola N (2005) Home dampness and molds, parental atopy, and asthma in childhood: a six-year population-based cohort study. Environ Health Perspect 113:357–361. https://doi.org/10.1289/ehp.7242
Kahouli S (2020) An economic approach to the study of the relationship between housing hazards and health: the case of residential fuel poverty in France. Energy Econ 85:104592. https://doi.org/10.1016/j.eneco.2019.104592
Katsoulakos NM, Kaliampakos DC (2014) What is the impact of altitude on energy demand? A step towards developing specialized energy policy for mountainous areas. Energy Policy 71:130–138. https://doi.org/10.1016/j.enpol.2014.04.003
Khanom L (2000) Impact of fuel poverty on health in Tower Hamlets. In: Cutting the cost of cold. Routledge
Lacroix E, Chaton C (2015) Fuel poverty as a major determinant of perceived health: the case of France. Public Health 129. https://doi.org/10.1016/j.puhe.2015.02.007
Lewbel A (2012) Using heteroscedasticity to identify and estimate mismeasured and endogenous regressor models. J Bus Econ Stat 30:67–80. https://doi.org/10.1080/07350015.2012.643126
Li Y, Ning X, Wang Z et al (2022) Would energy poverty affect the wellbeing of senior citizens? Evidence from China. Ecol Econ 200:107515. https://doi.org/10.1016/j.ecolecon.2022.107515
Liddell C, Morris C (2010) Fuel poverty and human health: a review of recent evidence. Energy Policy 38:2987–2997. https://doi.org/10.1016/j.enpol.2010.01.037
Lloyd CR, Callau MF, Bishop T, Smith IJ (2008) The efficacy of an energy efficient upgrade program in New Zealand. Energy and Buildings 40:1228–1239. https://doi.org/10.1016/j.enbuild.2007.11.006
Longhurst N, Hargreaves T (2019) Emotions and fuel poverty: the lived experience of social housing tenants in the United Kingdom. Energy Res Soc Sci 56:101207. https://doi.org/10.1016/j.erss.2019.05.017
Lowry S (1991) Housing and health. Br Med J
Lynch JW, Kaplan GA, Salonen JT (1997) Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med 44:809–819. https://doi.org/10.1016/S0277-9536(96)00191-8
Maidment CD, Jones CR, Webb TL et al (2014) The impact of household energy efficiency measures on health: a meta-analysis. Energy Policy 65:583–593. https://doi.org/10.1016/j.enpol.2013.10.054
Maller CJ, Henderson-Wilson C, Townsend M (2009) Rediscovering nature in everyday settings: or how to create healthy environments and healthy people. EcoHealth 6:553–556. https://doi.org/10.1007/s10393-010-0282-5
Mann (2003) The psychological impact of teleworking: stress, emotions and health—New Technology, Work and Employment—Wiley Online Library
O’Brien AJ, McKenna BG, Thom K et al (2011) Use of Tasers on people with mental illness a New Zealand database study. Int J Law Psychiatry 34:39–43. https://doi.org/10.1016/j.ijlp.2010.11.006
Ohrnberger J, Fichera E, Sutton M (2017) The relationship between physical and mental health: a mediation analysis. Soc Sci Med 195:42–49. https://doi.org/10.1016/j.socscimed.2017.11.008
Oliveras L, Peralta A, Palència L et al (2021) Energy poverty and health: trends in the European Union before and during the economic crisis, 2007–2016. Health Place 67:102294. https://doi.org/10.1016/j.healthplace.2020.102294
Palmer G, Maclnnes T, Kenway P (2008) Cold and poor: an analysis of the link between fuel poverty and low income
Parra-Saavedra M, Miranda J (2021) Maternal mental health is being affected by poverty and COVID-19. Lancet Glob Health 9:e1031–e1032. https://doi.org/10.1016/S2214-109X(21)00245-X
Peat JK, Dickerson J, Li J (1998) Effects of damp and mould in the home on respiratory health: a review of the literature. Allergy 53:120–128. https://doi.org/10.1111/j.1398-9995.1998.tb03859.x
Pelletier L, Shamila S, Scott BP, Demers A (2017) Self-management of mood and/or anxiety disorders through physical activity/exercise. Health Promot Chronic Dis Prev Can 37:27–32
Platt SD, Martin CJ, Hunt SM, Lewis CW (1989) Damp housing, mould growth, and symptomatic health state. BMJ 298:1673–1678. https://doi.org/10.1136/bmj.298.6689.1673
Pollard A, Jones T, Sherratt S, Sharpe RA (2019) Use of simple telemetry to reduce the health impacts of fuel poverty and living in cold homes. Int J Environ Res Public Health 16:2853. https://doi.org/10.3390/ijerph16162853
Roodman D (2011) Fitting fully observed recursive mixed-process models with cmp. Stand Genomic Sci 11:159–206. https://doi.org/10.1177/1536867X1101100202
Rosenow J, Galvin R (2013) Evaluating the evaluations: evidence from energy efficiency programmes in Germany and the UK. Energy and Buildings 62:450–458. https://doi.org/10.1016/j.enbuild.2013.03.021
Shortt N, Rugkåsa J (2007) “The walls were so damp and cold” fuel poverty and ill health in Northern Ireland: Results from a housing intervention. Health Place 13:99–110. https://doi.org/10.1016/j.healthplace.2005.10.004
Sickles RC, Taubman P (1986) An analysis of the health and retirement status of the elderly. Econometrica 54:1339–1356. https://doi.org/10.2307/1914302
Tavares AI (2017) Telework and health effects review. Int J Healthcare 3:30
Thomson H, Snell C (2013) Quantifying the prevalence of fuel poverty across the European Union. Energy Policy 52:563–572. https://doi.org/10.1016/j.enpol.2012.10.009
Vlassoff C (2007) Gender differences in determinants and consequences of health and illness. J Health Popul Nutr 25:47–61
Webber P, Gouldson A, Kerr N (2015) The impacts of household retrofit and domestic energy efficiency schemes: a large scale, ex post evaluation. Energy Policy 84:35–43. https://doi.org/10.1016/j.enpol.2015.04.020
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Appendix
Appendix
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Charlier, D., Legendre, B. (2023). Energy Poverty and Health Pathologies: An Empirical Study on the French Case. In: Bardazzi, R., Pazienza, M.G. (eds) Vulnerable Households in the Energy Transition. Studies in Energy, Resource and Environmental Economics. Springer, Cham. https://doi.org/10.1007/978-3-031-35684-1_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-35684-1_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-35683-4
Online ISBN: 978-3-031-35684-1
eBook Packages: Economics and FinanceEconomics and Finance (R0)