Abstract
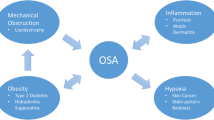
Skin disorders are a common comorbidity of sleep apnea, and sleep apnea itself may deteriorate the skin. Obstructive sleep apnea (OSA) is an inflammatory disease that is associated with obesity and mechanical obstruction of the airways leading to episodes of tissue hypoxia. This chapter reviews the literature on the association between OSA and dermatologic disorders. Four etiopathogenic mechanisms may explain the relationship of many dermatologic processes with OSA: systemic bidirectional inflammation associated with OSA and inflammatory skin disease (best exemplified by psoriasis and atopic dermatitis) in which each condition exacerbates the other; obesity itself and the conditions associated (diabetes, hidradenitis suppurativa, polycystic ovary syndrome); mechanical obstruction of the upper airways; and finally, the hypoxia related to OSA may be associated with skin cancer, in particular melanoma. Many of these associations are clear and have been well studied and documented. However, more research is needed to describe better the mechanisms underlying the clinical associations between skin diseases and OSA and the potential therapeutic effects on skin diseases when treating OSA with CPAP or other interventions.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014.
Jennum P, Ibsen R, Kjellberg J. Morbidity prior to a diagnosis of sleep-disordered breathing: a controlled national study. J Clin Sleep Med. 2013;9:103–8.
Jennum P, Ibsen R, Kjellberg J. Morbidity and mortality in children with obstructive sleep apnoea: a controlled national study. Thorax. 2013;68:949–54.
Drager LF, Togeiro SM, Polotsky VY, et al. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62:569–76.
Gupta MA, Gupta AK. Psychiatric and psychological co-morbidity in patients with dermatologic disorders: epidemiology and management. Am J Clin Dermatol. 2003;4:833–42.
Gupta MA, Simpson FC. Obstructive sleep apnea and psychiatric disorders: a systematic review. J Clin Sleep Med. 2015;11:165–75.
Gupta MA, Gupta AK. Sleep-wake disorders and dermatology. Clin Dermatol. 2013;31:118–26.
Savransky V, Jun J, Li J, et al. Dyslipidemia and atherosclerosis induced by chronic intermittent hypoxia are attenuated by deficiency of stearoyl coenzyme A desaturase. Circ Res. 2008;103:1173–80.
McNicholas WT, Bonsigore MR. Management Committee of ECAB. Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J. 2007;29:156–78.
Hirotsu C, Nogueira H, Albuquerque RG, Tomimori J, Tufik S, Andersen ML. The bidirectional interactions between psoriasis and obstructive sleep apnea. Int J Dermatol. 2015;54:1352–8.
Gaines J, Vgontzas AN, Fernandez-Mendoza J, et al. Inflammation mediates the association between visceral adiposity and obstructive sleep apnea in adolescents. Am J Physiol Endocrinol Metab. 2016;311:E851–8.
Can M, Uygur F, Tanriverdi H, et al. Effect of continuous positive airway pressure (CPAP) therapy on IL-23 in patients with obstructive sleep apnea. Immunol Res. 2016;64:1179–84.
Phillips BG, Wang Y, Ambati S, Ma P, Meagher RB. Airways therapy of obstructive sleep apnea dramatically improves aberrant levels of soluble cytokines involved in autoimmune disease. Clin Immunol. 2020;221:108601.
Polat D, Demirtaş E, Ahmet B, Yarali H. Decreased serum paraoxonase 1 (PON1) activity: an additional risk factor for atherosclerotic heart disease in patients with PCOS? Hum Reprod. 2006;21:104–8.
Van Cauter E. Sleep disturbances and insulin resistance. Diabet Med. 2011;28:1455–62.
Gupta MA, Simpson FC, Gupta AK. Psoriasis and sleep disorders: a systematic review. Sleep Med Rev. 2015;29:63–75.
Gowda S, Goldblum OM, McCall WV, et al. Factors affecting sleep quality in patients with psoriasis. J Am Acad Dermatol. 2010;63:114–23.
Machado-Pinto J, Diniz Mdos S, Bavoso NC. Psoriasis: new comorbidities. An Bras Dermatol. 2016;91:8–14.
Egeberg A, Khalid U, Gislason GH, et al. Psoriasis and sleep apnea: a Danish nationwide cohort study. J Clin Sleep Med. 2016;12:663–71.
Bissonnette R, Maari C, Bolduc C, et al. Prevalence of obstructive sleep apnea in obese patients with psoriasis. J Am Acad Dermatol. 2012;66:AB133.
Chiu HY, Hsieh CF, Chiang YT, et al. Concomitant sleep disorders significantly increase the risk of cardiovascular disease in patients with psoriasis. PloS One. 2016;11:e0146462.
Cohen JM, Jackson CL, Li TY, et al. Sleep disordered breathing and the risk of psoriasis among US women. Arch Dermatol Res. 2015;307:433–8.
Duffin KC, Woodcock J, Walsh J, et al. Increased prevalence of sleep apnea in patients with psoriasis compared to matched controls. Clin Transl Sci. 2012;5:170.
Papadavid E, Vlami K, Dalamaga M, et al. Sleep apnea as a comorbidity in obese psoriasis patients: a cross-sectional study. Do psoriasis characteristics and metabolic parameters play a role? J Eur Acad Dermatol Venereol. 2013;27:820–6.
Tsai TF, Wang TS, Hung ST, et al. Epidemiology and comorbidities of psoriasis patients in a national database in Taiwan. J Dermatol Sci. 2011;63:40–6.
Yang YW, Kang JH, Lin HC. Increased risk of psoriasis following obstructive sleep apnea: a longitudinal population-based study. Sleep Med. 2012;13:285–9.
Papadavid E, Dalamaga M, Vlami K, Koumaki D, Gyftopoulos S, Christodoulatos GS, et al. Psoriasis is associated with risk of obstructive sleep apnea independently from metabolic parameters and other comorbidities: a large hospital-based case-control study. Sleep Breath. 2017;21:949–58.
Shalom G, Dreiher J, Cohen A. Psoriasis and obstructive sleep apnea. Int J Dermatol. 2016;55:e579–84.
Castello-Branco RC, Cerqueira-Silva T, Andrade AL, Gonçalves BM, Pereira CB, Felix IF, Santos LS, Porto LM, Marques ME, Catto MB, et al. Association between risk of obstructive sleep apnea and cerebrovascular reactivity in stroke patients. J Am Heart Assoc. 2020;9:e015313.
Saçmaci H, Gürel G. Sleep disorders in patients with psoriasis: across-sectional study using non-polysomnographical methods. Sleep Breath. 2019;23:893–8.
Gabryelska A, Białasiewicz P. Is autonomic activation a middleman between obstructive sleep apnea syndrome and psoriasis? J Clin Sleep Med. 2018;14:1087–8.
Gowda S, Goldblum OM, McCall WV, Feldman SR. Factors affecting sleep quality in patients with psoriasis. J Am Acad Dermatol. 2010;63:114–23.
Maari C, Bolduc C, Nigen S, Marchessault P, Bissonnette R. Effect of adalimumab on sleep parameters in patients with psoriasis and obstructive sleep apnea: a randomized controlled trial. J Dermatol Treat. 2014;25:57–60.
Vakil M, Park S, Broder A. The complex associations between obstructive sleep apnea and auto-immune disorders: a review. Med Hypotheses. 2018;110:138–43.
Kim J, Kim BE, Leung DYM. Pathophysiology of atopic dermatitis: Clinical implications. Allergy Asthma Proc. 2019;40:84–92.
Cabanillas B, Brehler AC, Novak N. Atopic dermatitis phenotypes and the need for personalized medicine. Curr Opin Allergy Clin Immunol. 2017;17:309–15.
Darsow U, Raap U, Ständer S. Atopic dermatitis. In: Carstens E, Akiyama T, editors. Itch: mechanisms and treatment. Boca Raton, FL: CRC Press; 2014. Chapter 3.
Wolter S, Price HN. Atopic dermatitis. Pediatr Clin North Am. 2014;61:241–60.
Tien KJ, Chou CW, Lee SY, Yeh NC, Yang CY, Yen FC, et al. Obstructive sleep apnea and the risk of atopic dermatitis: a population-based case control study. PloS One. 2014;9:e89656.
Arens R, Marcus CL. Pathophysiology of upper airway obstruction: a developmental perspective. Sleep. 2004;27:997–1019.
Olusesi AD, Undie NB, Amodu JE. Allergy history as a predictor of early onset adenoids/adenotonsillar hypertrophy among Nigerian children. Int J Pediatr Otorhinolaryngol. 2013;77:1032–5.
Alexopoulos EI, Bizakis J, Gourgoulianis K, Kaditis AG. Atopy does not affect the frequency of adenotonsillar hypertrophy and sleep apnoea in children who snore. Acta Paediatr. 2014;103:1239–43.
Huo Z, Shi J, Shu Y, Xiang M, Lu J, Wu H. The relationship between allergic status and adenotonsillar regrowth: a retrospective research on children after adenotonsillectomy. Sci Rep. 2017;7:46,615.
Kheirandish-Gozal L, Bandla HP, Gozal D. Montelukast for children with obstructive sleep apnea: results of a double-blind, randomized, placebo-controlled trial. Ann Am Thorac Soc. 2016;13:1736–41.
Dayyat E, Serpero LD, Kheirandish-Gozal L, Goldman JL, Snow A, Bhattacharjee R, et al. Leukotriene pathways and in vitro adenotonsillar cell proliferation in children with obstructive sleep apnea. Chest. 2009;135:1142–9.
Fishbein AB, Lor J, Penedo FJ, Forrest CB, Griffith JW, Paller AS. Patient-reported outcomes for measuring sleep disturbance in pediatric atopic dermatitis: cross sectional study of PROMIS pediatric sleep measures and actigraphy. J Am Acad Dermatol. 2020;
Association between obstructive sleep apnea and atopic dermatitis in children: a nationwide, population-based cohort study. Pediatr Allergy Immunol. 2018;29:260–6.
Fishbein AB, Mueller K, Kruse L, Boor P, Sheldon S, Zee P, et al. Sleep disturbance in children with moderate/severe atopic dermatitis: a case-control study. J Am Acad Dermatol. 2018;78:336–41.
Treister AD, Stefek H, Grimaldi D, Rupani N, Zee P, Yob J, et al. Sleep and limb movement characteristics of children with atopic dermatitis coincidentally undergoing clinical polysomnography. J Clin Sleep Med. 2019;15:1107–13.
Reuveni H, Chapnick G, Tal A, et al. Sleep fragmentation in children with atopic dermatitis. Arch Pediatr Adolesc Med. 1999;153:249–53.
Bozkurt B, Serife Ugur K, Karamanli H, et al. Polysomnographic findings in persistent allergic rhinitis. Sleep Breath. 2016. [Epub ahead of print].
Tahrani AA, Ali A, Raymond NT, Begum S, Dubb K, Mughal S, et al. Obstructive sleep apnea and diabetic neuropathy: a novel association in patients with type 2 diabetes. Am J Respir Crit Care Med. 2012;186:434–41.
Altaf QA, Ali A, Piya MK, Raymond NT, Tahrani AA. The relationship between obstructive sleep apnea and intra-epidermal nerve fiber density, PARP activation and foot ulceration in patients with type 2 diabetes. J Diabetes Complications. 2016;30:1315–20.
Vas PR, Ahluwalia R, Manas AB, Manu CA, Kavarthapu V, Edmonds ME. Undiagnosed severe sleep apnoea and diabetic foot ulceration—a case series based hypothesis: a hitherto under emphasized factor in failure to heal. Diabet Med. 2016;33:e1–4.
van der Zee HH, de Ruiter L, van den Broecke DG, et al. Elevated levels of tumour necrosis factor (TNF)-a, interleukin (IL)-1b and IL-10 in hidradenitis suppurativa skin: a rationale for targeting TNF-a and IL-1b. Br J Dermatol. 2011;164:1292–8.
Alberti A, Sarchielli P, Gallinella E, et al. Plasma cytokine levels in patients with obstructive sleep apnea syndrome: a preliminary study. J Sleep Res. 2003;12:305–11.
Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80:40–52.
Wertenteil S, Strunk A, Garg A. Incidence of obstructive sleep apnoea in patients with hidradenitis suppurativa: a retrospective population-based cohort analysis. Br J Dermatol. 2018;179:1398–9.
Vinkel C, Thomsen SF. Risk factors for cardiovascular disease in patients with hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2017;31:e411–3.
Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62:569–76.
Matusiak L, Bieniek A, Szepietowski JC. Increased serum tumour necrosis factor-alpha in hidradenitis suppurativa patients: is there a basis for treatment with anti-tumour necrosis factor-alpha agents? Acta Dermatovenereol. 2009;89:601–3.
Kelly A, Meurling J, Kirthi Jeyarajah S, Ryan C, Hughes R, Garvey J, Kirby B. Obstructive sleep apnoea in psoriasis and hidradenitis suppurativa. Br J Dermatol. 2021;184:1183–5.
Fogel RB, Malhotra A, Pillar G, et al. Increased prevalence of obstructive sleep apnea syndrome in obese women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2001;86:1175–80.
Vgontzas AN, Legro RS, Bixler EO, et al. Polycystic ovary syndrome is associated with obstructive sleep apnea and daytime sleepiness: role of insulin resistance. J Clin Endocrinol Metab. 2001;86:517–20.
Tasali E, Van Cauter E, Ehrmann DA. Relationships between sleep disordered breathing and glucose metabolism in polycystic ovary syndrome. J Clin Endocrinol Metab. 2006;91:36–42.
Gopal M, Duntley S, Uhles M, et al. The role of obesity in the increased prevalence of obstructive sleep apnea syndrome in patients with polycystic ovarian syndrome. Sleep Med. 2002;3:401–4.
Chatterjee B, Suri J, Suri JC, et al. Impact of sleep-disordered breathing on metabolic dysfunctions in patients with polycystic ovary syndrome. Sleep Med. 2014;15:1547–53.
Nandalike K, Agarwal C, Strauss T, et al. Sleep and cardiometabolic function in obese adolescent girls with polycystic ovary syndrome. Sleep Med. 2012;13:1307–12.
Kahal H, Kyrou I, Tahrani A, Randeva H. Obstructive sleep apnoea and polycystic ovary syndrome: a comprehensive review of clinical interactions and underlying pathophysiology. Clin Endocrinol (Oxf). 2017;87:313–9.
Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet. Respir Med. 2015;3:310–8.
Tasali E, Chapotot F, Leproult R, et al. Treatment of obstructive sleep apnea improves cardiometabolic function in young obese women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2011;96:365–74.
Tasali E, Van Cauter E, Hoffman L, et al. Impact of obstructive sleep apnea on insulin resistance and glucose tolerance in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2008;93:3878–84.
Mokhlesi B, Scoccia B, Mazzone T, et al. Risk of obstructive sleep apnea in obese and nonobese women with polycystic ovary syndrome and healthy reproductively normal women. Fertil Steril. 2012;97:786–91.
Yang HP, Kang JH, Su HY, et al. Apnea-hypopnea index in nonobese women with polycystic ovary syndrome. Int J Gynaecol Obstet. 2009;105:226–9.
Lin TY, Lin PY, Su TP, et al. Risk of developing obstructive sleep apnea among women with polycystic ovarian syndrome: a nationwide longitudinal follow-up study. Sleep Med. 2017;36:165–9.
Analysis of the proportion and clinical characteristics of obstructive sleep apnea in women with polycystic ovary syndrome. Sleep Breath. 2022;26:497–503.
Hoppin AG, Katz ES, Kaplan LM, et al. Case records of the Massachusetts General Hospital. Case 31–2006. A 15-year-old girl with severe obesity. N Engl J Med. 2006;355:1593–602.
Ismailogullari S, Ferahbas A, Aksu M, et al. Effects of isotretinoin treatment on sleep in patients with severe acne: a pilot study. J Eur Acad Dermatol Venereol. 2012;26:778–81.
Haynes D, Topham C, Greiling T. Acne keloidalis nuchae and obstructive sleep apnoea: a retrospective case series. Clin Exp Dermatol. 2019;44:e214–5.
Kelly AP. Pseudofolliculitis barbae and acne keloidalis nuchae. Dermatol Clin. 2003;21:645–53.
Verma SB, Wollina U. Acne keloidalis nuchae: another cutaneous symptom of metabolic syndrome, truncal obesity, and impending/overt diabetes mellitus? Am J Clin Dermatol. 2010;11:433–6.
Buyuktas D, Arslan E, Celik O, Tasan E, Demirkesen C, Gundogdu S. Elephantiasis nostras verrucosa on the abdomen of a Turkish female patient caused by morbid obesity. Dermatol Online J. 2010;16:14.
Shanmugam VK, Tsagaris KC, Attinger CE. Leg ulcers associated with Klinefelter's syndrome: a case report and review of the literature. Int Wound J. 2012;9:104–7.
Hegele RA, Al-Attar SA, Rutt BK. Obstructive sleep apnea in 2 women with familial partial lipodystrophy due to a heterozygous LMNA R482Q mutation. CMAJ. 2007;177:743–5.
Carr A, Cooper DA. Adverse effects of antiretroviral therapy. Lancet. 2000;356(9239):1423–30.
Epstein LJ, Strollo PJ Jr, Donegan RB, Delmar J, Hendrix C, Westbrook PR. Obstructive sleep apnea in patients with human immunodeficiency virus (HIV) disease. Sleep. 1995;18:368–76.
Abdeen Y, Al-Halawani M, Kaako A, Hao IFY, Dazley J, Katpally R, Klukowicz A, Miller R, Slim J. Effect of the duration of protease inhibitor therapy in HIV-infected individuals on the severity of obstructive sleep apnea. J Res Med Sci. 2019;24:65.
Harsch IA, Bergmann T, Koebnick C, Wiedmann R, Ruderich F, Hahn EG, et al. Adiponectin, resistin and subclinical inflammation—the metabolic burden in Launois Bensaude Syndrome, a rare form of obesity. J Physiol Pharmacol. 2007;58(Suppl 1):65–76.
Hanson RD, Olsen KD, Rogers RS III. Upper aerodigestive tract manifestations of cicatricial pemphigoid. Ann Otol Rhinol Laryngol. 1988;97:493–9.
Hubbard M, Masters IB, Williams GR, et al. Severe obstructive sleep apnea secondary to pressure garments used in the treatment of hypertrophic burn scars. Eur Respir J. 2000;16:1205–7.
Gozal D, Ham SA, Mokhlesi B. Sleep apnea and cancer: analysis of a nationwide population sample. Sleep. 2016;39:1493–500.
Gozal D, Farré R, Nieto FJ. Putative links between sleep apnea and cancer from hypotheses to evolving evidence. Chest. 2015;148:1140–7.
Martínez-García MÁ, Campos-Rodriguez F, Barbé F. Cancer and OSA: current evidence from human studies. Chest. 2016;150:451–63.
Martínez-García MA, Martorell-Calatayud A, Nagore E, et al. Association between sleep disordered breathing and aggressiveness markers of malignant cutaneous melanoma. Eur Respir J. 2014;43:1661–8.
Almendros I, Montserrat JM, Torres M, et al. Intermittent hypoxia increases melanoma metastasis to the lung in a mouse model of sleep apnea. Respir Physiol Neurobiol. 2013;186:303–7.
Santamaria-Martos F, Benítez I, Girón C, Barbé F, Martínez-García MA, Hernández L, et al. Biomarkers of carcinogenesis and tumour growth in patients with cutaneous melanoma and obstructive sleep apnoea. Eur Respir J. 2018;51:1701885.
Almendros I, Martínez-García M, Campos-Rodríguez F, Riveiro-Falkenbach E, Rodríguez-Peralto JL, Nagore E, et al. Intermittent hypoxia is associated with high hypoxia inducible factor-1α but not high vascular endothelial growth factor cell expression in tumors of cutaneous melanoma patients. Front Neurol. 2018;9:272.
Martinez-Garcia MA, Campos-Rodriguez F, Nagore E, Martorell A, Rodriguez-Peralto JL, Riveiro-Falkenbach E, et al. Sleep-disordered breathing is independently associated with increased aggressiveness of cutaneous melanoma: a multicenter observational study in 443 patients. Chest. 2018;154:1348–58.
Martinez-Garcia MA, Campos-Rodriguez F, Almendros I, et al. Relationship between sleep apnea and cancer. Arch Bronconeumol. 2015;51:456–61.
Tan NKW, Yap DWT, Tan BKJ, et al. The association of obstructive sleep apnea with melanoma incidence and mortality: a meta-analysis of 5,276,451 patients. Sleep Med. 2021;88:213–20.
Almendros I, Martínez-García MA, Campos-Rodríguez F, et al. Intermittent hypoxia is associated with high hypoxia inducible factor-1a but not high vascular endothelial growth factor cell expression in tumors of cutaneous melanoma patients. Front Neurol. 2018:9.
Hunyor I, Cook KM. Models of intermittent hypoxia and obstructive sleep apnea: molecular pathways and their contribution to cancer. Am J Physiol Regul Integr Comp Physiol. 2018;315(R669):r87.
Li H, Chen J, Wang X, et al. Nodal induced by hypoxia exposure contributes todacarbazine resistance and the maintenance of stemness in melanoma cancer stem-like cells. Oncol Rep. 2018;39:2855–64.
Sun X, Lv X, Yan Y, et al. Hypoxia-mediated cancer stem cell resistance and targeted therapy. Biomed Pharmacother. 2020;130:110623.
Lin Y, Xu J, Lan H. Tumor-associated macrophages in tumor metastasis: biological roles and clinical therapeutic applications. J Hematol Oncol. 2019;12:76.
Cole SW, Sood AK. Molecular pathways: beta-adrenergic signaling in cancer. Clin Cancer Res. 2012;18:1201–6.
Moretti S, Massi D, Farini V, et al. b-adrenoceptors are upregulated in humanmelanoma and their activation releases pro-tumorigenic cytokines and metalloproteases in melanoma cell lines. Lab Invest. 2013;93:279–90.
Dal Monte M, Calvani M, Cammalleri M, et al. b-Adrenoceptors as drug targets in melanoma: novel preclinical evidence for a role of b (3) -adrenoceptors. Br J Pharmacol. 2019;176:2496–508.
Baik I, Lee S, Thomas RJ, Shin C. Obstructive sleep apnea, low transferrin saturation levels, and male-pattern baldness. Int J Dermatol. 2019;58:67–74.
Reintgen C, Leavitt A, Pace E, Molas-Pierson J, Mast BA. Risk factor analysis for mastectomy skin flap necrosis. implications for intraoperative vascular analysis. Ann Plast Surg. 2016;76(Suppl 4):S336–9.
Pépin JL, Leger P, Veale D, Langevin B, Robert D, Lévy P. Side effects of nasal continuous positive airway pressure in sleep apnea syndrome. Study of 193 patients in two French sleep centers. Chest. 1995;107:375–81.
Pepin JL, Leger P, Veale D, et al. Side effects of nasal continuous positive airway pressure in sleep apnea syndrome. Study of 193 patients in two French sleep centers. Chest. 1995;107:375–81.
Reynaerts A, Bruze M, Erikstam U, et al. Allergic contact dermatitis from a medical device, followed by depigmentation. Contact Dermatitis. 1998;39:204–5.
Elkin PL, Mullin S, Sakilay S. Rosacea patients are at higher risk for obstructive sleep apnea: automated retrospective research. Stud Health Technol Inform. 2020;270:1381–2.
Logger JGM, Peppelman M, Vugt RV, Driessen RJB. Rosacea and use of continuous positive airway pressure mask for obstructive sleep apnea syndrome: report of five cases. Ann Dermatol. 2020;32:3.
Matin A, Bliwise DL, Wellman JJ, Ewing HA, Rasmuson P. Resolution of dyshidrotic dermatitis of the hand after treatment with continuous positive airway pressure for obstructive sleep apnea. South Med J. 2002;95:253–4.
Nino G, Singareddy R. Severe onychophagia and finger mutilation associated with obstructive sleep apnea. J Clin Sleep Med. 2013;9:379–81.
Arnardottir ES, Thorleifsdottir B, Svanborg E, et al. Sleep-related sweating in obstructive sleep apnoea: association with sleep stages and blood pressure. J Sleep Res. 2010;19:122–30.
Schlaud M, Urschitz MS, Urschitz-Duprat PM, et al. The German study on sleep-disordered breathing in primary school children: epidemiological approach, representativeness of study sample, and preliminary screening results. Paediatr Perinat Epidemiol. 2004;18:431–40.
Eitner S, Urschitz MS, Guenther A, et al. Sleep problems and daytime somnolence in a German population-based sample of snoring school-aged children. J Sleep Res. 2007;16:96–101.
Arnardottir ES, Janson C, Bjornsdottir E, et al. Nocturnal sweating–a common symptom of obstructive sleep apnoea: The Icelandic sleep apnoea cohort. BMJ Open. 2013;3:e002795.
Gabryelska A, Sochal M, Wasik B, Bialasiewicz P. Patients with obstructive sleep apnea are over four times more likely to suffer from psoriasis than the general population. J Clin Sleep Med. 2018;14:153.
Martinez-Garcia MA, Campos-Rodriguez F, Almendros I, Garcia-Rio F, Sanchez-de-la-Torre M, Farre R, et al. Cancer and sleep apnea: cutaneous melanoma as a case study. Am J Respir Crit Care Med. 2019;200:1345–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Redondo, P. (2023). Dermatologic Changes Related to Patients with Obstructive Sleep Apnea. In: Baptista, P.M., Lugo Saldaña, R., Amado, S. (eds) Obstructive Sleep Apnea. Springer, Cham. https://doi.org/10.1007/978-3-031-35225-6_26
Download citation
DOI: https://doi.org/10.1007/978-3-031-35225-6_26
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-35224-9
Online ISBN: 978-3-031-35225-6
eBook Packages: MedicineMedicine (R0)