Abstract
Molecular targeted therapies are characterized by blocking essential biochemical pathways or mutant proteins that are required for cancer cell growth and survival. Targeted cancer therapeutics are amongst the major treatment options for cancer today. These treatments are more selective for cancer cells and improve the quality of life for cancer patients undergoing therapy. Nevertheless, cardiotoxicity is a frequent side effect in targeted therapies, frequently described as myocardial dysfunction and heart failure. Cardiotoxicity includes also any subsequent functional or structural heart injury, with a possible accelerated development of cardiovascular diseases. Early identification of patients at risk for cardiotoxicity from cancer target therapies and the early diagnosis of CV complications related to cancer treatments are crucial. Anamnesis and risk stratification are the first steps of the diagnostic process to detect myocardial toxicity. Electrocardiography, cardiac biomarkers, and cardiac imaging modalities (echocardiography, CMR, PET, conventional imaging, and cardiac CT) are essential for a cardiotoxicity screening.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
12.1 Cancer Targeted Therapies
Molecular targeted therapies are characterized by blocking essential biochemical pathways or mutant proteins that are required for cancer cell growth and survival [1]. The National Cancer Institute defines a target therapy as “type of treatment that uses drugs or other substances to identify and attack specific types of cancer cells with less harm to normal cells. Some targeted therapies block the action of certain enzymes, proteins, or other molecules involved in the growth and spread of cancer cells. Other types of targeted therapies help the immune system kill cancer cells or deliver toxic substances directly to cancer cells and kill them. Targeted therapy may have fewer side effects than other types of cancer treatment. Most targeted therapies are either small molecule drugs or monoclonal antibodies” [2]. Targets selected for molecular targeted therapy include growth factors, signalling molecules, cell-cycle proteins, modulators of apoptosis and molecules that promote angiogenesis, among many others ([3], Fig. 12.1). Targets that are commonly used for imaging and therapy in nuclear medicine practice are radiolabelled peptides. Peptides are important regulators of growth, cellular function and intercellular communication and they act as neurotransmitters, regulating immune response and information transduction. Peptide ligands are neurotransmitters, hormones, chemokines, cytokines and growth factors. Receptors targeted with radiolabelled peptides have become an important topic, particularly in nuclear oncology [4].
Summary of molecular targeted therapy mechanisms. Molecular targeted therapy on cancer focuses on targeting specific cancer-associated molecules that are highly expressed in cancer cells or by modulating the tumour microenvironment related to tumour vasculature, metastasis or hypoxia. (Y.T. Lee et al. [3])
Targeted cancer therapeutics are amongst the major treatment options for cancer today, together with cytotoxic chemotherapies. These treatments are more selective for cancer cells and improve the quality of life for cancer patients undergoing therapy [5]. However, these molecular targets are expressed also in normal cells, which explains the different grades of toxicity, resulting from the disruption of normal cellular function. Along with the benefits of disease stabilization different adverse events are reported [6, 7]. The radiopeptide treatments improve survival in cancer patients without significant evidence of cardiac function impairment.
12.2 Cardiotoxicity of Cancer Targeted Therapy
One frequent side effect in targeted therapies is cardiotoxicity. Cardiotoxicity related to cancer therapy is a broad term and includes any functional or structural heart injury related to cancer treatment. Cardiotoxicity is well known to occur secondary to cancer chemo and radiotherapy and may lead to premature morbidity and death among cancer survivors because of the direct effects of the cancer treatment on heart function and structure. Cardiotoxic effects have also been observed in novel targeted therapies. In the context of underlying cardiovascular diseases (CVD), which are the leading cause of death in the Western world, it may accelerate the development of CVD, especially in the presence of traditional cardiovascular risk factors [7,8,9,10]. To identify patients at risk for cardiotoxicity from cancer therapy, it is crucial to detect previous subclinical cardiac abnormalities and to perform an early detection of possible cardiovascular complications during treatment by increasing, for example, the surveillance frequency [10, 11].
Myocardial dysfunction and heart failure (HF), frequently described as cardiotoxicity, are the most concerning cardiovascular complications of cancer therapies and cause an increase in morbidity and mortality [10]. Cardiotoxicity is grouped into two categories, based on different pathological changes and clinical characteristics:
-
Type I: traditional, related to traditional chemotherapy.
-
Type II: targeted, related to novel targeted therapeutic agents.
Anthracyclines are the prototype of type I agents and are associated with a significant risk of left ventricular dysfunction (LVD) or HF, compared with non-anthracycline therapies [12]. The pathophysiological mechanisms differ by drug and include accelerated atherosclerosis, coronary spasm, vascular endothelial damage and arterial thrombotic events [13]. In addition to cardiac dysfunction, which is typical for anthracycline-based chemotherapies, targeted cancer therapy-induced cardiotoxicities may manifest also as elevated blood pressure, atherosclerosis, thromboembolism, pericardial thickening and arrhythmia [12]. Unfortunately, the understanding of the underlying pathophysiology and natural history of cardiotoxicity remains limited. Therefore, it is critical to perform an early patient risk stratification [13].
12.3 Diagnostic Tools to Detect Myocardial Toxicity
12.3.1 Anamnesis and Risk Stratification
The first step to identify patients at increased risk for cardiotoxicity consists of a careful baseline anamnesis. Demographic (age, family history of CVD), lifestyle (smoking, obesity, high alcohol intake, sedentary habit) and other cardiovascular risk factors (i.e. arterial hypertension, diabetes mellitus, hypercholesterolemia) should be collected to perform a patient risk stratification before cancer therapy. Previous cancer treatments should be also recorded.
12.3.2 Electrocardiography
Electrocardiography (ECG) is recommended in all patients before and during the cancer treatments. It is useful to detect any ECG signs of cardiac toxicity, either transitory or chronic, including ST-T wave changes, conduction disturbances, arrhythmias, and others [10, 13].
12.3.3 Cardiac Biomarkers
The use of cardiac biomarkers during cardiotoxic chemotherapy may be considered in order to detect early cardiac injury. They are accurate, reproducible, widely available, and high-sensitive Troponin I, high-sensitivity Troponin I, B-type natriuretic Peptide (BNP) and NT-proBNP are generally recorded. However, there is currently no clear evidence about the role of cardiac biomarkers to detect cardiotoxicity due to both targeted molecular therapies as well as traditional chemotherapy [10].
12.3.4 Imaging Modalities for Cardiotoxicity Screening
Cardiac imaging modalities include echocardiography, cardiac magnetic resonance imaging, positron emission tomography, conventional nuclear imaging techniques, cardiac computer tomography and coronary computer tomography angiography. Functional testing with exercise or stress agents is also routinely used to diagnose either LV myocardial ischaemia or other LV perfusion abnormalities [10, 13, 14].
12.3.4.1 Echocardiography
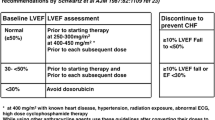
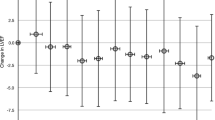
Cancer patients treated with potentially cardio-toxic therapy are at high risk of developing myocardial dysfunction and congestive HF. LV ejection fraction (LVEF) as a global marker of LV systolic function is currently used and several strategies have been applied over the past decades to detect it. Cardiac dysfunction resulting from exposure to cancer treatments was first recognized in the 1960s, with the widespread introduction of anthracyclines into the oncologic therapeutic setting. Different definitions of cancer therapeutics–related cardiac dysfunction (CTRCD) have been historically used [15]. A joint committee of the American Society of Echocardiography and the European Association of Cardiovascular Imaging defined the CTRCD as a decrease in the LVEF of >10% points, to a value <53% (normal reference value for two-dimensional (2D) echocardiography). The decrease should be confirmed by repeated cardiac imaging. The repeat study should be performed 2–3 weeks after the baseline diagnostic study showing the possible initial decrease in LVEF. That should be further categorized as symptomatic or asymptomatic, or with regard to reversibility [16].
2D-echocardiography is the method of choice to detect the LVEF before, periodically during and after potential cardiotoxic cancer therapy. This is because of its wide availability, reproducibility, versatility, lack of radiation exposure and also safety in patients with concomitant renal disease. The modified 2D-biplane Simpson method is recommended for estimation of LVEF and LV volumes. Echocardiography allows the evaluation of left and right ventricular dimensions, volumes, and function as well as valvular, and pericardial pathology. [10, 13, 16] Despite some limitations, the incorporation of modern techniques such as myocardial contrast echocardiography, three-dimensional (3D) echocardiography, Doppler tissue imaging and speckle-tracking echocardiography offer a prudent compromise between cost-effectiveness and clinical predictive value [14].
12.3.4.2 Cardiac Magnetic Resonance
Cardiac magnetic resonance (CMR) is a helpful tool for the evaluation of cardiac structures, myocardial function as well as pericardium. Late gadolinium enhancement (LGE) imaging may be useful to detect scarring or fibrosis and can sensitively detect a myocardial infarction. The quantitative myocardial perfusion mapping allows to quantify the regional myocardial perfusion reserve. CMR is an excellent test for the comprehensive evaluation of cardiac masses and infiltrative conditions. Accuracy and reproducibility are characteristics of CMR, despite its limited availability [10, 12].
12.3.4.3 Nuclear Positron Emission Tomography
Positron emission tomography (PET) is the gold standard technique to assess myocardial perfusion and metabolism in nuclear medicine practice, due to its high spatial and temporal resolution and high diagnostic sensitivity and accuracy. Hybrid systems with either computer tomography (CT) or magnetic resonance imaging (MRI) have been used.
The use of cardiac PET, and in particular of quantitative myocardial perfusion PET, has been growing during the last decade. [13N]-labelled ammonia, [15O]-labelled water and 82Rubidium have been employed as effective myocardial perfusion tracers. The acquisition protocols using dynamic acquisitions allow the absolute quantification of LV myocardial blood flow (MBF) at rest and after stress as well as the derivation of LV coronary flow reserve (CFR). Gating, that is an ECG synchronized registration, provides functional information such as LVEF, left ventricular volumes, wall motion and wall thickening. Moreover, quantitative PET makes possible to assess the presence of LV microvascular dysfunction, which is involved in various cardiac diseases, including the early stages of coronary artery atherosclerosis, hypertrophic and dilated cardiomyopathy, and hypertensive heart disease. Nevertheless, the acquisition and analysis of quantitative PET requires a high level of expertise [17, 18]. PET is also the gold standard technique to analyse myocardial metabolism or to assess myocardial viability using 2-[18F]fluorodeoxyglucose (FDG). Clinical studies applying cardiac PET to monitor for cardiotoxicity related to cancer target therapies are limited. Recent publications report accurate estimation of left and right functional parameters also from routine dynamic whole-body FDG PET scans for oncological purposes, which could open a new perspective for further clinical applications of the PET examinations [19].
Targeted cancer therapy-induced cardiotoxicities may manifest also as a development or a progression of atherosclerosis. During the past decade, studies suggested that PET/CT with FDG is a valid tool to assess and to reliably quantify atherosclerotic inflammatory activity by evaluating the glucose metabolism of corresponding immune cells and to predict severe cardio- and cerebrovascular events in oncological patients [20, 21]. Recently, it was reported a significant increase of arterial inflammation in large arteries in patients suffering from melanoma treated with immune checkpoint inhibitor therapy, using FDG PET/CT imaging [22].
Patients with haematological malignancies could rarely develop light chain amyloidosis, which may present with cardiac amyloidosis, an infiltrative cardiomyopathy, often presenting as heart failure with preserved LVEF. Echocardiography and CMR imaging are useful for the diagnosis of cardiac amyloidosis but they cannot reliably distinguish it from other infiltrative heart diseases. PET/CT with radiopharmaceuticals that were originally developed for the detection of cerebral amyloid deposits and diagnosis of Alzheimer’s disease, like 18F-florbetair or 11C-PIB have recently shown promising results for the detection of cardiac and extra-cardiac amyloidosis [23].
12.3.4.4 Conventional Nuclear Imaging
The American Society of Clinical Oncology guidelines 2016 recommend the use of multiple gated acquisition (MUGA) with technetium-99m [99mTc] labelled red blood cells to assess LVEF, if such a measurement is not feasible by echocardiography and CMR. Limitations include a radiation exposure and its inability to assess additional information on cardiac structure [10, 16].
An increasing number of Nuclear Medicine sites are routinely using single photon emission computer tomography (SPECT) systems to diagnose coronary artery disease or to detect myocardial ischemia. ECG-gated cardiac SPECT allows for reliable estimating myocardial perfusion as well as functional parameters (LVEF, LV volumes), LV wall motion and LV wall thickening with high accuracy [24].
12.3.4.5 Cardiac Computed Tomography, Angio-Coronary Computer Tomography
Whilst cardiotoxicity related to cancer therapy generally focuses on LV impairment, cancer treatments can cause other clinical cardiac syndromes including coronary events, pericardial disease, valvular heart diseases, pulmonary hypertension and right ventricular dysfunction. CT coronary angiography provides a non-invasive anatomical assessment of coronary artery disease. Among the immune and targeted therapeutics, those inhibiting the vascular endothelial growth factor (VEGF) signalling pathway have an increased risk for coronary thrombosis, which can be detected non-invasively by this technique [10, 12, 13].
12.4 Summary
Molecular targeted therapies are characterized by blocking essential biochemical pathways or mutant proteins that are required for cancer cell growth and survival. Targeted cancer therapeutics are amongst the major treatment options for cancer today. These treatments are more selective for cancer cells and improve the quality of life for cancer patients undergoing therapy. Nevertheless, one frequent side effect in targeted therapies is cardiotoxicity, frequently described as myocardial dysfunction and HF. Cardiotoxicity includes also any subsequent functional or structural heart injury, with a possible accelerated development of CVD. The early identification of patients at risk for cardiotoxicity from cancer target therapies and the early diagnosis of CV complications related to cancer treatments are crucial. Anamnesis and risk stratification are the first steps of the diagnostic process to detect myocardial toxicity. ECG detects cardiac electrical changes, cardiac biomarkers may be considered to detect early cardiac injury. Imaging modalities for cardiotoxicity screening include echocardiography, the method of choice to detect the LVEF, and CMR imaging, to evaluate cardiac structures, myocardial function and infiltrative conditions. Nuclear PET is the gold standard technique to assess LV myocardial perfusion and metabolism, to detect the development or a progression of acoronary artery therosclerosis and to identify cardiac and extra-cardiac amyloidosis. Conventional imaging in nuclear medicine practice includes MUGA and cardiac SPECT. Cardiac CT is a valid tool to detect morphological pathologies of heart, pericardial disease, valvular heart diseases, pulmonary hypertension, or right ventricular dysfunction. CT coronary angiography provides a non-invasive anatomical assessment of coronary artery disease.
References
Vanneman M, Dranoff G. Combining immunotherapy and targeted therapies in cancer treatment. Nat Rev Cancer. 2012;12(4):237–51.
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/targeted-therapy.
Lee YT, Tan YJ, Oon CE. Molecular targeted therapy: treating cancer with specificity. Eur J Pharmacol. 2018;834:188–96.
Ambrosini V, Fani M, Fanti S, Forrer F, Maecke HR. Radiopeptide imaging and therapy in Europe. J Nucl Med. 2011;52(Suppl 2):42S–55S.
Miller MJ, Foy KC, Kaumaya PT. Cancer immunotherapy: present status, future perspective, and a new paradigm of peptide immunotherapeutics. Discov Med. 2013;15(82):166–76.
Widakowich C, De Castro G Jr, De Azambija E, Dihn P, Awada A. Review: side effects of approved molecular targeted therapies in solid cancers. Oncologist. 2007;12:1443.
Zuppinger C, Suter TM. Cancer therapy-associated cardiotoxicity and signaling in the myocardium. J Cardiovasc Pharmacol. 2010;56(2):141–6.
WHO. Cardiovascular diseases (CVDs). Fact sheet no. 317. Geneva: World Health Organization; 2015. http://www.who.int/mediacentre/factsheets/fs317/en/.
2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016;37:2999–3058.
Zamorano JL, Lancellotti P, Rodriguez Muñoz D, Aboyans V, Asteggiano R, Galderisi M, Habib G, Lenihan DJ, Lip GYH, Lyon AR, Lopez Fernandez T, Mohty D, Piepoli MF, Tamargo J, Torbicki A, Suter TM, ESC Scientific Document Group. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(36):2768–801.
Poulin F, Thavendiranathan P. Cardiotoxicity due to chemotherapy: role of cardiac imaging. Curr Cardiol Rep. 2015;17(3):564.
Chen Z, Ai D. Cardiotoxicity associated with targeted cancer therapies. Mol Clin Oncol. 2016;4(5):675–81.
Seraphim A, Westwood M, Bhuva AN, Crake T, Moon JC, Menezes LJ, Lloyd G, Ghosh AK, Slater S, Oakervee H, Manisty CH. Advanced imaging modalities to monitor for cardiotoxicity. Curr Treat Options Oncol. 2019;20(9):73.
Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, Ganame J, Sebag IA, Agler DA, Badano LP, Banchs J, Cardinale D, Carver J, Cerqueira M, DeCara JM, Edvardsen T, Flamm SD, Force T, Griffin BP, Jerusalem G, Liu JE, Magalhães A, Marwick T, Sanchez LY, Sicari R, Villarraga HR, Lancellotti P. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2014;27(9):911–39.
Khouri MG, Douglas PS, Mackey JR, Martin M, Scott JM, Scherrer-Crosbie M, Jones LW. Cancer therapy-induced cardiac toxicity in early breast cancer: addressing the unresolved issues. Circulation. 2012;126(23):2749–63.
Awadalla M, Hassan MZO, Alvi RM, Neilan TG. Advanced imaging modalities to detect cardiotoxicity. Curr Probl Cancer. 2018;42(4):386–96.
Sciagrà R, Lubberink M, Hyafil F, Saraste A, Slart RHJA, Agostini D, Nappi C, Georgoulias P, Bucerius J, Rischpler C, Verberne HJ, Cardiovascular Committee of the European Association of Nuclear Medicine (EANM). EANM procedural guidelines for PET/CT quantitative myocardial perfusion imaging. Eur J Nucl Med Mol Imaging. 2021;48:1040–69.
Sciagrà R. Quantitative cardiac positron emission tomography: the time is coming! Scientifica (Cairo). 2012;2012:948653.
Rasul S, Beitzke D, Wollenweber T, et al. Assessment of left and right ventricular functional parameters using dynamic dual-tracer [13N]NH3 and [18F]FDG PET/MRI. J Nucl Cardiol. 2020;29:1003.
Bucerius J, Hyafil F, Verberne HJ, Slart RH, Lindner O, Sciagra R, Agostini D, Übleis C, Gimelli A, Hacker M, Cardiovascular Committee of the European Association of Nuclear Medicine (EANM). Position paper of the Cardiovascular Committee of the European Association of Nuclear Medicine (EANM) on PET imaging of atherosclerosis. Eur J Nucl Med Mol Imaging. 2016;43(4):780–92.
Rominger A, Saam T, Wolpers S, Cyran CC, Schmidt M, Foerster S, Nikolaou K, Reiser MF, Bartenstein P, Hacker M. 18F-FDG PET/CT identifies patients at risk for future vascular events in an otherwise asymptomatic cohort with neoplastic disease. J Nucl Med. 2009;50(10):1611–20.
Calabretta R, Hoeller C, Pichler V, Mitterhauser M, Karanikas G, Haug A, Li X, Hacker M. Immune checkpoint inhibitor therapy induces inflammatory activity in large arteries. Circulation. 2020;142:2396.
García-González P, Cozar-Santiago MDP, Maceira AM. Cardiac amyloidosis detected using 18F-florbetapir PET/CT. Rev Esp Cardiol (Engl Ed). 2016;69(12):1215.
Verberne HJ, Acampa W, Anagnostopoulos C, Ballinger J, Bengel F, De Bondt P, Buechel RR, Cuocolo A, van Eck-Smit BL, Flotats A, Hacker M, Hindorf C, Kaufmann PA, Lindner O, Ljungberg M, Lonsdale M, Manrique A, Minarik D, Scholte AJ, Slart RH, Trägårdh E, de Wit TC, Hesse B, European Association of Nuclear Medicine (EANM). EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur J Nucl Med Mol Imaging. 2015;42(12):1929–40.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Calabretta, R., Hacker, M. (2024). Cardiotoxicity of Targeted Therapies: Imaging of Heart Does Matter. In: Prasad, V. (eds) Beyond Becquerel and Biology to Precision Radiomolecular Oncology: Festschrift in Honor of Richard P. Baum. Springer, Cham. https://doi.org/10.1007/978-3-031-33533-4_12
Download citation
DOI: https://doi.org/10.1007/978-3-031-33533-4_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-33532-7
Online ISBN: 978-3-031-33533-4
eBook Packages: MedicineMedicine (R0)