Abstract
A major transformation of life in the last decades has been the delay in fertility – that is, the decrease in fertility among people below age 25–30. At the same time that fertility has been delayed, the proportion of people having children later in life has increased, but in many countries, completed fertility has declined. In this chapter I (re)consider the extent to which these three phenomena –fertility delay, increase in later fertility, and fertility decline – are related. I examine whether fertility delay causes fertility decline and review evidence that an increasing number of people are facing constraints to childbearing in later life. Finally, I discuss the relevance of changes in partnership dynamics for fertility decline, as well as some implications of fertility delay on future completed fertility.
I take a cohort and life course approach. While I acknowledge the temporality of fertility behavior and the importance of period “shocks” (e.g., recessions, pandemics), a cohort approach is the most natural way to examine the link between fertility timing (i.e., delay) and fertility quantum: the key question is, after all, whether the same people who delay fertility earlier in life wind up with fewer children at the end of their reproductive window. To explore overall trends as well as cross-country variation, I cover a range of low fertility countries at different stages of fertility delay and with different childbearing contexts over the 1940–80 birth cohorts.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Fertility timing
- Fertility quantum
- Infertility
- Medically assisted reproduction
- Postponement
- Recuperation
- Late fertility
1 Introduction
A major transformation of life in the last decades has been the delay in fertility – that is, the decrease in fertility among people below age 25 to 30 (Beaujouan & Toulemon, 2021; Lesthaeghe, 2016; Sobotka et al., 2011). At the same time that fertility has been delayed, the proportion of people having children later in life has increased, but in many countries, completed fertility has declined. In this chapter I (re)consider the extent to which these three phenomena –fertility delay, increase in later fertility, and fertility decline – are related. I examine whether fertility delay causes fertility decline and review evidence that an increasing number of people are facing constraints to childbearing in later life. Finally, I discuss the relevance of changes in partnership dynamics for fertility decline, as well as some implications of fertility delay on future completed fertility.
I take a cohort and life course approach. While I acknowledge the temporality of fertility behavior and the importance of period “shocks” (e.g., recessions, pandemics), a cohort approach is the most natural way to examine the link between fertility timing (i.e., delay) and fertility quantum: the key question is, after all, whether the same people who delay fertility earlier in life wind up with fewer children at the end of their reproductive window. To explore overall trends as well as cross-country variation, I cover a range of low fertility countries at different stages of fertility delay and with different childbearing contexts over the 1940–80 birth cohorts.
2 Recent Trends in Early, Late, and Completed Fertility in Low Fertility Countries
2.1 The Mean Age at First Birth Has Increased
Fifty years after the first signs of delayed fertility in Western Europe, the average age at which women have their first child is now increasing in countries of most world areas (Bongaarts et al., 2017; Lima et al., 2018; Neels et al., 2017). Figure 4.1 displays the increase in women’s mean age at first birth in selected low fertility countries in Europe, North America and East Asia among the cohorts born between 1940 and 1980. The mean age at first birth started increasing among women born in the 1940–50s in the countries of North America, Western and Southern Europe and East Asia (see also Frejka & Sardon, 2006). In most Eastern Europe countries, there has been a more recent but strong increase in the mean age at first birth among women born in the 1960s. Compared with other low fertility countries, the Eastern European countries are at an earlier stage of their “postponement transition” (Kocourková & Šťastná, 2021). In some countries, such as the Netherlands and Spain, the mean age at first birth appears to have stabilized across birth cohorts, as well as periods (Neels et al., 2017). Variability in first birth schedule has also stabilized in these countries, which suggests that the capacity to further delay the first birth towards later ages may be limited (Kohler & Ortega, 2002; Nathan & Pardo, 2019).
2.2 Large Cross-Country Differences with Regard to Later Fertility
The increase in mean age at first birth can be driven by a decrease in first birth rates at younger ages, an increase at older ages, or a combination of both. To disentangle trends in earlier and later fertility in the low fertility countries, and also link them to completed fertility, Fig. 4.2 compares changes in cumulated cohort fertility rate (CCFR) up to age 30 (CCFR30) and between age 30 and 43 (CCFR30–43) as well as changes in the CFR up to age 43 (presumably close to completed fertility; CCFR43) for the cohorts born 1940–80 in selected low-fertility countries. Across all countries shown but to varying extents, fertility below age 30 has declined and fertility between age 30 and 43 has increased. Increases in later fertility can (partially) compensate for decreases in earlier fertility, so that completed fertility remains more or less stable. As seen in Fig. 4.2, with the exception of the United States, decreases in CFR30 have outweighed increases in CFR30-43, and the CFR43 has declined. Nevertheless, the degree to which increases in CFR30-43 have offset decreases in CFR30 differs quite a bit across the countries shown. For example, the drop in fertility before age 30 was similar in Austria and Sweden, but the increase in later fertility in Sweden was much larger than in Austria: completed fertility remained almost stable there, while it decreased quickly in Austria.
Many studies have confirmed that increases in later fertility have rarely completely offset decreases in earlier fertility, but also that there is substantial cross-country variation (Beaujouan & Toulemon, 2021; Frejka & Calot, 2001; Neels & De Watcher, 2010; Sobotka et al., 2011). Compared to women born in 1945–50, women born in the late 1960s in Sweden and the United States had fewer children earlier in life but more children later in life, such that their completed fertility was more or less comparable with their predecessors in earlier cohorts (Sobotka et al., 2011). In contrast, in the same birth cohorts in Austria and Spain, the increase in later fertility was much smaller in magnitude than the decrease in early fertility, resulting in a strong decrease in completed fertility (Sobotka et al., 2011). The decline in completed fertility in most countries is particularly attributable to a decline in second and higher order birth rates, but childlessness has also risen quickly in Southern Europe, Western Europe and East Asia (Frejka & Sardon, 2006; Sobotka, 2017, 2021; Zeman et al., 2018).
In most countries, delay and decrease in completed fertility occurred within the same birth cohorts. Figure 4.2 shows nonetheless that decreases in earlier fertility have not always coincided with decreases in completed fertility: across several cohorts in Japan, Sweden and the Netherlands, completed fertility remained stable despite a drop in earlier fertility. In addition, in the Netherlands and Spain, a sharp decrease in completed fertility was observed in the late 1930s-early 1940s birth cohorts, even though fertility below age 30 was rather stable. This is explained by family size limitation at parity 3 and higher, prevalent in these cohorts in the Netherlands and Spain, irrespective of fertility delay (Zeman et al., 2018).
2.3 Fertility Delay or Postponement?
Scholars have commonly referred to the widely observed decline in fertility below age 25 or 30 as “fertility postponement”, and the increase in later life fertility as “fertility recuperation” (see extensive discussion in Frejka, 2011). The terms “postponement” and “recuperation” suggest that people who do not have children at an earlier age entertain the idea of having children later, and then try to achieve a specific, pre-set fertility target later in life (Frejka, 2011). It is not obvious that this is the case, neither empirically, as we have shown previously, nor conceptually. Research suggests that most people – especially most young people – lack concrete, long-term fertility intentions (Bachrach & Morgan, 2013; Ní Bhrolcháin & Beaujouan, 2019; Trinitapoli & Yeatman, 2018). Intended family size primarily reflects a person’s perceptions of the normative family (Bachrach & Morgan, 2013). Young adults in particular report wanting a number of children that is close to the number of children observed in the previous generation and their own number of siblings (Heiland et al., 2008; Régnier-Loilier, 2006). Younger peoples’ fertility intentions predict their shorter-term fertility behavior fairly well, but poorly predict their fertility behavior in the longer-term (Schoen et al., 1999). Also later in the life course, fertility aspirations (intentions, desires, expectations) are rather unstable and only weakly related to future fertility (Beaujouan et al., 2019; Buhr & Huinink, 2017; Gemmill, 2018; Gray et al., 2013; Rybińska & Morgan, 2019). In sum, fertility aspirations do not appear to be a meaningful construct for many people (Ní Bhrolcháin, 1992; Schoen, 2004).
Given the nebulous nature of fertility aspirations particularly earlier in life, it seems unlikely that fertility delay has primarily been driven by a conscious decision to “postpone” and then “recuperate” fertility later in life once the structural and individual conditions for having the intended number of children were met. In the birth cohorts in which fertility delay occurred, young people probably lacked a clearly defined idea about whether they wanted to have children (and if so, how many) at the same time that they were already having comparatively fewer children than young people in the previous cohort. Instead of “postponement”, fertility delay could just as well reflect that fertility has become a non-issue for young adults in more recent cohorts. Compared to their predecessors, members of more recent cohorts are more likely to be enrolled in education, unemployed or at the very beginning of their career well into their reproductive windows – all situations that are hardly compatible with childbearing (Mills et al., 2011; Ní Bhrolcháin & Beaujouan, 2012). It seems likely that such normative changes to early adult life have led young people to defer the decision to have children. It is also possible that fertility delay has been the result of lower fertility aspirations. In either case, there is no particular reason to expect that later fertility would systematically increase in response to decreases in fertility in earlier life (Ní Bhrolcháin & Toulemon, 2005). “Fertility postponement” and “fertility recuperation” would thus appear to be misnomers. I therefore prefer to use the more neutral term “fertility delay” as opposed to “fertility postponement” when referring to the decrease in fertility rates below age 30 (as compared to the previous birth cohorts) and increase in mean age at first birth. In the same vein, I prefer to use “increase in later fertility” as opposed to “fertility recuperation” to refer to increases in fertility rates above age 30 that (sometimes) follow a drop in earlier fertility.
3 Does Fertility Delay Cause Fertility Decline?
To what extent does fertility delay actually cause fertility decline? Or, in other words, to what extent does fertility delay per se act as a barrier to family formation and expansion? Most of the studies on the relationship between fertility delay and decline are descriptive or correlational, and hence provide little evidence of causality. It nevertheless seems probable that the fertility decline observed in cohorts born after 1940 is at least partly attributable to fertility delay for at least three reasons.
First, fertility delay implies that more people are exposed to biological constraints when they attempt to begin or expand a family. The ability to give birth to a live child decreases exponentially from age 32 among women (Broekmans et al., 2007). Other less tangible constraints related to age also seem to exist, whether cultural, normative or individual (Beaujouan et al., 2019). Consequently, women who – consciously or not – defer childbearing to a later age are much more likely to be affected by biological or normative constraints to childbearing (Leridon & Slama, 2008; te Velde et al., 2012).
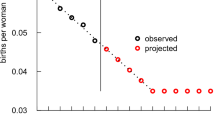
Age constraints appear to be most relevant for second and higher order births (Sobotka et al., 2011). Given the overwhelming preference for two children in many countries (Sobotka & Beaujouan, 2014), one can expect that people who have had a first child will want a second one. Figure 4.3 displays the probability of having a second child by age among women who already have one child, in the same countries as in Fig. 4.2 across the cohorts born 1946–81. Figure 4.3 confirms that the probability of having a second birth in the 30s and early 40s increased massively among women who delayed having a first child (only from the 1960s for Hungary and Czechia). Sweden and Spain had the highest second birth probabilities at age 35 (around 20% of women with one child) and at age 40 (around 7%). It is however striking that from age 35, in all countries observed –even those that delayed having a first child most such as the Netherlands and Spain–, second birth probabilities decreased extremely fast. The rapidly decreasing probability of second birth with age and its stabilization in countries where it is the highest suggest that further delaying the first birth towards the 35–45 age range would very probably lead to a systematic decrease in completed fertility, particularly via a reduction in higher order births. Adjusting for the duration since the first birth is nonetheless necessary to quantify the loss of higher order births due to fertility delay (Rallu & Toulemon, 1994).
A second reason why fertility delay has probably had a causal effect on fertility decline is that the delay implies that people are spending a shorter period trying to have children. People are “at risk” of having a child across the entire reproductive window, but their level of risk depends on their particular situation. For instance, their risk is lower if they are single or in education, and the risk is higher if they are in a stable union. When exposure to low-risk situations earlier in life increases, less people have a child early and fertility in early life decreases. This systematically increases the share of persons at risk of having a child later in life in the birth cohort. Hence, if the risk of having a child later in life remains the same as in the previous birth cohort, later fertility rates increase due to higher exposure (which we could call structural recuperation, see Winkler-Dworak et al. (2022)). However, in order for completed fertility to remain stable, the risk of childbearing later in life would have to increase, as established by Winkler-Dworak et al. (2022) using micro-simulation modelling. As an example, if union formation is normatively delayed from the 20s to the 30s, more people will be single in their 20s. Being single is a low-risk situation, so fertility in the 20s will decrease. More people will be in their 30s when they enter a partnership, and hence more people will have children in their 30s. However, so far, the overall risk of childbearing is lower in the 30s as compared to the 20s, which corresponds to lower childbearing risk for the same exposure. Hence, fertility delay does provoke systematic fertility decline, and the extent to which increases in later fertility compensate for decreases in earlier fertility is contingent upon changing behavior, for instance more people entering a union or increasing birth intensity at later ages (Winkler-Dworak et al., 2022). Through the same mechanisms, the cumulation of shocks such as unemployment or uncertainty due to a pandemic also creates periods of lower risk of having children (Comolli & Vignoli, 2021; Luppi et al., 2020; Matysiak et al., 2020), and can eventually contribute to fertility decline.
Third, there is evidence that fertility delay can also cause people to want fewer children, or none at all. As fertility is delayed, people have more time to invest in other activities (e.g., volunteering, hobbies, sports, travel, night life), and get used to the idea of living without children or in small families. The interference of childbearing with these other activities seems to frequently result in a reduced desire to have a(nother) child (Berrington & Pattaro, 2014; Morgan, 2003). Morgan (2003, p. 599) notes that “continuing delay and competing opportunities translate some delayed fertility into forgone fertility”. Particularly, those who postpone fertility have smaller families than those who started having children earlier (Andersson et al., 2009; Castro, 2014; Kocourková & Šťastná, 2021; Kohler et al., 2002), and those who strongly intend to have a child after age 30 are less likely to have it than younger people (Beaujouan et al., 2019; Brzozowska & Beaujouan, 2021; Kocourková & Šťastná, 2021).
To conclude, while there are reasons to believe that fertility delay has contributed to fertility decline, it is also clear that the relationship between fertility delay and fertility decline is not entirely straightforward. Fertility delay and decline sometimes occur independently (see Fig. 4.2), and there is no evidence that increases in age at first birth between the 1952 and 1972 birth cohorts were related to decreases in completed cohort fertility across European countries (Beaujouan & Toulemon, 2021). Also, the family size of mothers starting to have children in their 30s remained strikingly low in some countries even though more people were having children at these ages (Beaujouan et al., 2023). Fertility delay is clearly not the only factor driving fertility decline, but studies that quantify the relationship between fertility delay and fertility decline are rare. So far, the direct negative impact of further fertility delay on completed fertility appears to be modest, around 0.1 to 0.2 fewer children per woman for 3–4 years of delay in the mean age of first child in France where completed fertility is around 2 children per woman (Leridon, 2017).
4 Evidence Suggests That an Increasing Number of People Are Experiencing Constraints to Childbearing in Later Reproductive Life
In the following, I review evidence that many people experience constraints to childbearing in later reproductive life: namely, (a) an increasing share of people would still like to have a(nother) child in the late 30s and 40s; (b) the use of medically-assisted reproduction (MAR) has increased especially among older persons; and (c) behavior becomes more conducive to childbearing as people near the end of the reproductive window.
4.1 Many People in Their Late 30s and 40s Would Still Like to Start or Expand Their Family
Permanent childlessness has risen dramatically across Europe (Sobotka, 2017). The extent to which childlessness is voluntary, a consequence of perpetual delay, or due to infertility is a debated topic in demography and sociology (Berrington, 2004; Fiori et al., 2017; Letherby, 2002). The instability of fertility aspirations across the life course makes it difficult to determine the extent to which childlessness is “voluntary” or “involuntary”. Nevertheless, fertility intentions do tend to become more concrete as life unfolds (Ní Bhrolcháin & Beaujouan, 2019). Examining fertility intentions and fertility behavior as people near the end of their reproductive window therefore constitutes a reasonable first step in quantifying the share of persons who unintentionally end up childless or with fewer children than they would have liked to have had because they “postponed too long” (Berrington, 2017; Tanturri & Mencarini, 2008).
Figure 4.4 shows the share of women childless at age 35–39 in Austria, France and the United Kingdom, distinguishing between those who did and did not want a child. The change in the proportion of childless women who still wanted a child at age 35–39 provides an indication of whether the share of involuntary childlessness was increasing as fertility delay was unrolling. In all the three countries, the share of women childless at age 35–39 more or less doubled from over 10 to over 20% in approximatively the same period (late 1980s to around 2010). The share of women who intended to remain childless varied greatly across countries (5% in France, 10% in Austria, 13% in the United Kingdom) but remained more or less stable over time. Most of the increase in the share of women childless at age 35–39 can thus be attributed to women who still wanted to have a child. The constancy of this feature across three very different contexts is remarkable.
Other evidence likewise suggests that involuntary childlessness and late fertility intentions are substantial and increasing. According to survey data, a non-negligeable share of childless women have tried to have a child but did not have one. In the United Kingdom, 15% of childless women born in 1970 said that they were childless due to their own or their partner’s infertility (Berrington, 2017), which represents about 3% of all women and remains relatively low. In contrast, in Italy 29% of permanently childless women surveyed in 2002 reported that they had experienced difficulties while trying to have a child (Tanturri & Mencarini, 2008). In addition, more than half of childless women in Spain aged 45–49 in 2018 still wished a child (that is, around 10% of all women) (Esteve & Treviño, 2019). Among women aged 40–42 with one child, the share intending to have another child increased from almost none in 1980 to around 9% in 2003–2009 in the United Kingdom (Beaujouan & Sobotka, 2022) and from 1.5% in 1986 to 15% in 2016 in Austria (Beaujouan, 2022). At other parities however, there was little increase in the share intending to have another child, possibly because most people either stop having children once they have had the two normative children, or stop wishing for additional children if they are older and conscious of the difficulties to have them.
Together, Fig. 4.4 and evidence of a rise in late fertility intentions suggest that many people experience constraints to childbearing in later reproductive life. Moreover, it appears that fertility delay is causing a substantial share of people to fall short of their desired family size.
4.2 Medically-Assisted Reproduction Has Increased Particularly Among Older Age Groups
MAR has increased dramatically: across the low fertility countries, 2 to 7% of all children are currently born with the support of MAR (Gliozheni et al., 2021). Research shows that most of the increase in infertility treatments between 2008 and 2017 concerned women older than 34 years in France, and that the number of babies conceived through assisted reproductive technologies (ART) among older women has increased faster than the number of ART-babies among younger women in Australia (Ben Messaoud et al., 2020; Lazzari et al., 2021). Also, the share of treatments provided to women age 40+ has increased considerably: about 22% of in vitro fertilization (IVF) /intracytoplasmic sperm injection treatments were provided to women aged 40+ in 2018, compared with 15% in 2005 (author’s calculations for 21 European countries based on Andersen et al., 2009; Wyns et al., 2022).
The marked increase in the uptake of MAR among women at the end of their reproductive window suggests that a growing share of women are trying to overcome age-related biological constraints to fertility. Most likely, this is due to the rising share of women who are trying to have children relatively late (Beaujouan, 2020). It is also possible, though unlikely (Moreau et al., 2010; Olsen et al., 1998; Sobotka et al., 2008), that access to MAR has increased more for older than for younger women who needed it. The rising number of extremely late first births (48 years and older) suggests that increasing use of MAR is fueled by increasing demand at very late ages (Beaujouan, 2020).
4.3 Behavior Becomes More Conducive to Childbearing as People Near the End of Their Reproductive Window
As a further indication that many people face constraints to childbearing in later life, there are hints that behavior appears to become more conductive to childbearing as people approach the end of their reproductive windows (biological or social). Few studies have examined how people react to fertility deadlines (Wagner et al., 2019), so for now this remains a working hypothesis. There is however evidence that people relax their requirements for childbearing in their late 30s and early 40s. For example, people appear more willing to have a child without a partner as they near the end of the reproductive window. Childless people aged 35–37 in Germany are more likely to intend to have a child in the short-term even when they are not in a partnership (Wagner et al., 2019). Using the Belgian census, Schnor (2022) showed that more than half of the women who have a child using MAR without a partner are over 35 years old.
Although factors such as country-level unemployment and welfare regime are related to fertility at all ages (Neels et al., 2012; Pifarré i Arolas, 2017), there is also some evidence that later fertility is less affected by negative conditions. Campisi et al. (2022) showed in the Nordic countries that variation in fertility rates of women below age 30 are more strongly related to the area’s economic conditions than the fertility rates of women above age 30. Across Europe, the Great Recession had a strong effect on first birth risk among women below age 30 but no effect on first birth risk among women above age 30 (Goldstein et al., 2013; Neels et al., 2012). However, older women experienced a decrease in higher order birth rates (Goldstein et al., 2013).
Finally, there is some evidence that people try to accelerate childbearing later in life. The later people enter a first union, the faster they have their first child afterwards (Compans & Beaujouan, 2022). However, because more women have reduced fertility from age 35 onward, biological constraints may interfere with behavioral acceleration, so that looking only at birth timing is not sufficient to assess behavioral changes. Future research should investigate whether other indicators of behavioral acceleration (e.g., irregular use of contraception, less stringent criteria for a partner) increase as people near the end of their reproductive windows.
5 Changes in Partnership Dynamics Have Contributed to Fertility Decline
Considerable societal changes have taken place since the onset of fertility delay, including the introduction of the pill, increases in educational attainment, and increases in female labor force participation (Balbo et al., 2013; Wilkins, 2019). Recent progress in modelling demonstrates that, by reducing the time spent “at risk” of childbearing, a longer time spent in education tends to systematically reduce the total number of births by the end of reproductive life (Bijlsma & Wilson, 2020; Ciganda & Todd, 2021). Partnership dynamics have changed as well: median age at first cohabiting union has increased in a number of countries among men and women born since the 1950s, and risks of separation and divorce have skyrocketed (Sobotka & Berghammer, 2021; Sobotka & Toulemon, 2008). Consequently, the time available to have a family has declined considerably (Ciganda & Todd, 2019; Fostik et al., 2021; Winkler-Dworak et al., 2019).
Most people consider having a partner as a prerequisite for starting a family (Wagner et al., 2019). In the past, fertility was closely linked with entry into the first union. Over the past decades, the link between entering a first union and having a first child has loosened considerably, particularly in Western Europe. Most people have a partner at some point in their 20s, but many will not have a child within this relationship and many partnerships will breakup. Hence, people are more likely to be single when they start thinking of having children in their 30s (Mikolai, 2017). This has of course strong implications for fertility, as less time spent in a union contributes to lower fertility (Ciganda & Todd, 2019; Fostik et al., 2021). Nishikido et al. (2022) recently found that the reduced likelihood of having a partner before age 30 in Spain, as opposed to lower birth intensities within unions, was a crucial aspect of the difference in first birth rates in Spain and Sweden.
The decrease in union stability (more breakups, more divorce) is also highly relevant for fertility. Despite an increased risk of childbearing in a second union as compared to a stable first union, people who separate have lower fertility. This has been found in Europe, Latin America, the United States and in other contexts as well (see e.g., Fostik et al., 2021; Meggiolaro & Ongaro, 2010; Thomson et al., 2012; Van Bavel et al., 2012). Microsimulations also find a negative relationship between union separation and fertility (Winkler-Dworak et al., 2017), suggesting that the relationship is not only linked to the selection of people more apt to have children into more stable unions, but also because separation shortens the period one spends in situation conducive to childbearing. Among women born in the 1980s who ever entered a union, the microsimulations estimated a loss of 28% of completed fertility for those who separated in Italy, 18% in the United Kingdom and 20% in France. The impact was largest for higher order births. Further research confirms a strong relationship between partnership trajectories and childlessness in Norway (Hart, 2019) and Finland (Saarela & Skirbekk, 2019), where persons who lived in several short unions and those who entered the latest their first union and separated quickly were most likely to be permanently childless. Further investigations of the causal effect of delayed unions as well as of the higher frequency of “trial first unions” (short first childless unions) for fertility levels are warranted, but we can expect a clear depressing effect on fertility (Jalovaara & Fasang, 2017).
6 Some Implications of Fertility Delay for Future Completed Fertility
6.1 Access to MAR Will Increasingly Contribute to Completed Fertility
Given that more people will not start trying to have a child until later in life, access to MAR has and will become more relevant for completed fertility. The contribution of MAR to overall and particularly later fertility is already far from negligeable. It has been estimated that babies born with the support of IVF will comprise between 3.8 and 5% of children born to the 1978 birth cohort in Denmark (Sobotka et al., 2008) and around 4% for this same birth cohort in Australia (Lazzari, 2021). In Australia, it is predicted that ART will contribute to more than 25% of births after age 40 among women born in 1986 (extrapolated success and treatment rates scenario). If this is the case, ART would account for more than half of the fertility recuperation between the 1968 and 1986 birth cohorts, and the cohort fertility rate would be of 1.9 instead of 1.8 children per woman (Lazzari, 2021). Such scenarios are very likely. MAR is already relatively effective, but its effectiveness decreases with age, so it cannot be considered as a substitute to beginning attempts to have a child earlier in life (Leridon, 2004; Sobotka & Beaujouan, 2018). The success of non-donor IVF after age 40 has hardly improved over time (Sobotka & Beaujouan, 2018), but other forms of MAR such as oocyte banking, oocyte donation and surrogacy offer better chances of success to have children at older ages (CDC, 2018; Kocourkova et al., 2014; Passet-Wittig & Bujard, 2021). The increased uptake of such methods will probably improve the success of MAR, particularly at older ages, and hence become even more important for overall fertility levels. Yet, the appropriateness and efficiency of MAR as a stimulant of late fertility and fertility in general is still to be discussed in most societies (Baldwin, 2018; Rainer et al., 2011; van de Wiel, 2020).
6.2 Life Conditions in the 30s and Early 40s Will Become More Relevant
In a context of delayed fertility, life circumstances in the 30s and early 40s – and work and health in particular – have and will become more important determinants of completed fertility. By age 30, work has become a central component of most people’s lives. Work-related factors (e.g., dedication, satisfaction, working conditions, instability) are thus likely to be much more relevant for fertility in the 30s than in the 20s. Women who work many hours may be more dedicated to their career and experience more stress, leaving less space for building a family (Bratti & Tatsiramos, 2011). On the other hand, having a good position on the labor market and job flexibility act as resources for rearing children (Rondinelli et al., 2010). At equal parity, highly-educated women, who not only tend to have the best job conditions but also better gender equality in the household, are most likely to have children in that age range (Berrington & Pattaro, 2014; Neels & De Watcher, 2010; Nicoletti & Tanturri, 2008; Rondinelli et al., 2006).
Relative to people in their 20s, people in their 30s and 40s are more likely to have a long-term illness or report worse health, which may prevent them from having children (Gray et al., 2013; Heiland et al., 2008; Mynarska & Wróblewska, 2017). Subjective well-being (e.g., stress, life satisfaction) and its relationship to fertility may also vary across adulthood (Greil, 1997; Mencarini et al., 2018). So far, little is known about how such individual characteristics (e.g., work, health, well-being) affect fertility at different points in the reproductive life span.
6.3 The Effect of Further Delay on Completed Fertility Will Depend on the Country
In some countries, there is probably enough leeway for most people to delay having a first child without affecting their completed fertility: they would still be fertile when trying to have a second or higher order child, despite having started later. This seemed to be the case still recently in France, and probably in many other countries. A simulation of the biological consequences of a delay of first births by 3–4 years in the French context shows a rather small drop in completed cohort fertility of 0.1–0.2 children, of which about 10–20% could be compensated by assisted reproductive technologies (Leridon, 2017). In France, Toulemon and Mazuy (2001) also projected that later childbearing in the 1980 birth cohorts (average around age 30 years) would only marginally affect their completed fertility. This suggests that, in France, cohorts have not reached yet their biological limits and most of the slight drop in completed fertility can be attributed to other elements. Further fertility delay would probably have a stronger negative impact in Southern Europe where birth schedules are already very late, and possibly weaker in Eastern Europe where the mean age of first child is still relatively young. In a study comparing France and Spain, Compans et al. (2022) show that, despite similar transition rates to second birth by age in the two countries, the very different profiles of age at first birth (much later in Spain) corresponds to a substantially lower proportion of Spanish women proceeding to a second birth than in France.
7 Conclusions and Outlook
Among the birth cohorts born since 1940, the proportion of women who have had a child by age 30 has steadily declined. Fertility delay probably reflects the deferral of fertility decisions until later in life due to structural and ideational changes in the conditions of early adulthood (e.g., longer time spent in education, delay in union formation). Overall, the arguments and evidence brought together in this chapter support the hypothesis that fertility delay has directly contributed to declines in cohort fertility. I have argued that fertility delay has directly contributed to fertility decline because, once they try to conceive, more people experience biological and normative age constraints to attaining the number of children they want. Another way that fertility delay affects completed fertility is by shortening the period during which one is “at risk” of childbearing, and there is also evidence that delay causes people to want fewer children. Ongoing changes in partnership dynamics also seem to contribute to fertility decline. In some countries, an increase in later fertility has at least partially compensated for the decrease in earlier life fertility. The potential to offset fertility delay by intensifying efforts to have children later in life may be more limited in countries in which childbearing already takes place very late. In light of fertility delay, conditions of life in the 30s and early 40s (work, health) and access to MAR will be more relevant predictors of completed fertility in the future.
Much more empirical work is needed to understand the relationship between fertility delay and fertility decline. Further studies would be helpful for assessing the (in)flexibility of different populations with regard to their fertility schedule and the existence of a ceiling at later ages, and for quantifying the extent to which fertility delay contributes to fertility decline. Fertility delay appears most relevant for second and higher order births (Kohler & Ortega, 2002), but estimating how many higher order births are missed as a result of fertility delay is difficult. Possibly, using parity progression ratios by age over time allows better such estimation, but again it is challenging to evaluate which children are missed due to “too much” delay, and which ones are no longer particularly expected. Comparative studies combining fertility history and fertility intention questions over time appear to have potential in that respect (Beaujouan, 2022; Guzzo & Hayford, 2023), but samples large enough to allow detailed decomposition by age are scarce.
Inequalities that might give way to and also arise from fertility delay are currently not well understood. For instance, highly-educated women have their children later and may therefore be more affected by biological and normative constraints to later fertility, but lower-educated women are less likely to use MAR at any age even in countries where it is financed by the state (Goisis et al., 2020). Also, unequal childbearing opportunities may arise from inequalities in working conditions (e.g., flexibility, income, childcare) or from health inequalities, which are more relevant at older ages. Fertility delay may thus accentuate inequalities associated with socioeconomic status and education in particular. Finally, gender inequality may become increasingly pertinent as fertility is delayed, as men face less of a biological deadline than women. So far gender differences in the reproductive window have been primarily relevant for fertility in second unions or stepfamilies, but one can still wonder whether the ability of men to change partners in order to have children even when they are in their 50s and older may give them more power over women. Men delay fertility to a lesser extent than women, suggesting that if such gender inequalities develop, it will not occur until later (Beaujouan, 2020).
References
Andersen, A. N., Goossens, V., Bhattacharya, S., Ferraretti, A. P., Kupka, M. S., De Mouzon, J., & Nygren, K. G. (2009). Assisted reproductive technology and intrauterine inseminations in Europe, 2005: Results generated from European registers by ESHRE. Human Reproduction, 24(6), 1267–1287. https://doi.org/10.1093/humrep/dep035
Andersson, G., Rønsen, M., Knudsen, L. B., Lappegård, T., Neyer, G., Skrede, K., Teschner, K., & Vikat, A. (2009). Cohort fertility patterns in the Nordic countries. Demographic Research, 20(14), 313–352. https://doi.org/10.4054/DemRes.2009.20.14
Bachrach, C. A., & Morgan, S. P. (2013). A cognitive–Social model of fertility intentions. Population and Development Review, 39(3), 459–485. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1728-4457.2013.00612.x
Balbo, N., Billari, F. C., & Mills, M. C. (2013). Fertility in advanced societies: A review of research. European Journal of Population, 29(1), 1–38. https://doi.org/10.1007/s10680-012-9277-y
Baldwin, K. (2018). Conceptualising women’s motivations for social egg freezing and experience of reproductive delay. Sociology of Health and Illness, 40(5), 859–873. https://doi.org/10.1111/1467-9566.12728
Beaujouan, É. (2020). Latest-late fertility? Decline and resurgence of late parenthood across the low-fertility countries. Population and Development Review, 46(2), 219–247. https://doi.org/10.1111/padr.12334
Beaujouan, É. (2022). Late fertility intentions increase over time in Austria, but chances to have a child at later ages remain low. Reproductive Biomedicine & Society Online, 14, 125–139. https://doi.org/10.1016/j.rbms.2021.10.002
Beaujouan, É., & Sobotka, T. (2022). Is 40 the new 30? Increasing reproductive intentions and fertility rates beyond age 40. In D. Nikolaou & D. Seifer (Eds.), Optimizing the management of fertility in women over 40 (pp. 3–18). Cambridge University Press. https://doi.org/10.1017/9781009025270.002
Beaujouan, É., & Toulemon, L. (2021). European countries with delayed childbearing are not those with lower fertility. Genus, 77(2), 1–15. https://doi.org/10.1186/s41118-020-00108-0
Beaujouan, É., Brown, J. J. J., & Ní Bhrolcháin, M. (2011). Reweighting the general household survey 1979-2007. Population Trends, 145, 119–145. https://doi.org/10.1057/pt.2011.21
Beaujouan, É., Ní Bhrolcháin, M., Berrington, A., & Falkingham, J. (2015). Centre for population change general household survey database, 1979–2009: Special Licence Access [computer file] (SN: 7666). Office for National Statistics. Social Survey Division [Original data producer]. http://discover.ukdataservice.ac.uk/catalogue?sn=7666
Beaujouan, É., Reimondos, A., Gray, E., Evans, A., & Sobotka, T. (2019). Declining realisation of reproductive intentions with age. Human Reproduction, 34(10), 1906–1914. https://doi.org/10.1093/humrep/dez150
Beaujouan, É., Zeman, K., & Nathan, M. (2023). Delayed first births and completed fertility across the 1940–1969 birth cohorts. Demographic Research, 48, 387–420. https://doi.org/10.4054/DemRes.2023.48.15
Ben Messaoud, K., Bouyer, J., & de La Rochebrochard, E. (2020). Infertility treatment in France, 2008–2017: A challenge of growing treatment needs at older ages. American Journal of Public Health., 110, 1418–1420. https://doi.org/10.2105/AJPH.2020.305781
Berrington, A. (2004). Perpetual postponers? Women’s, men’s and couple’s fertility intentions and subsequent fertility behaviour. Population Trends, 117, 9–19.
Berrington, A. (2017). Childlessness in the UK. In M. Kreyenfeld & D. Konietzka (Eds.), Childlessness in Europe: Contexts, causes, and consequences (pp. 57–76). Springer Open. https://link.springer.com/book/10.1007/978-3-319-44667-7
Berrington, A., & Pattaro, S. (2014). Educational differences in fertility desires, intentions and behaviour: A life course perspective. Advances in Life Course Research, 21, 10–27. https://doi.org/10.1016/j.alcr.2013.12.003
Bijlsma, M. J., & Wilson, B. (2020). Modelling the socio-economic determinants of fertility: a mediation analysis using the parametric g-formula. Journal of the Royal Statistical Society – Series A, 183, 493–513. https://doi.org/10.1111/rssa.12520
Bongaarts, J., Mensch, B. S., & Blanc, A. K. (2017). Trends in the age at reproductive transitions in the developing world: The role of education. Population Studies, 71(2), 139–154. https://doi.org/10.1080/00324728.2017.1291986
Bratti, M., & Tatsiramos, K. (2011). The effect of delaying motherhood on the second childbirth in Europe. Journal of Population Economics, 25(1), 291–321. https://doi.org/10.1007/s00148-010-0341-9
Broekmans, F. J., Knauff, E. A. H., te Velde, E. R., Macklon, N. S., & Fauser, B. C. (2007). Female reproductive ageing: Current knowledge and future trends. Trends in Endocrinology and Metabolism: TEM, 18(2), 58–65. https://doi.org/10.1016/j.tem.2007.01.004
Brzozowska, Z., & Beaujouan, É. (2021). Assessing short-term fertility intentions and their realisation using the generations and gender survey: Pitfalls and challenges. European Journal of Population, 37, 405–416. https://doi.org/10.1007/s10680-020-09573-x
Buhr, P., & Huinink, J. (2017). Why childless men and women give up on having children. European Journal of Population., 33, 585–606. https://doi.org/10.1007/s10680-017-9429-1
Campisi, N., Kulu, H., Mikolai, J., Klüsener, S., & Myrskylä, M. (2022). A spatial perspective on the unexpected Nordic fertility decline: The relevance of economic and social contexts. Applied Spatial Analysis and Policy., 16, 1–31. https://doi.org/10.1007/s12061-022-09467-x
Castro, R. (2014). Late-entry-into-motherhood women are responsible for fertility recuperation. Journal of Biosocial Science, 47, 275–279. https://doi.org/10.1017/S0021932014000121
CDC. (2018). Assisted reproductive technology. 2016 fertility clinic success rates report. https://www.cdc.gov/art/reports/2016/fertility-clinic.html
Ciganda, D., & Todd, N. (2019). The limits to fertility recuperation. MPIDR working paper, WP 2019-02. https://www.demogr.mpg.de/papers/working/wp-2019-024.pdf
Ciganda, D., & Todd, N. (2021). Demographic models of the reproductive process: Past, interlude, and future. Population Studies, 76(3), 495–513. https://doi.org/10.1080/00324728.2021.1959943
Comolli, C. L., & Vignoli, D. (2021). Spreading uncertainty, shrinking birth rates: A natural experiment for Italy. European Sociological Review, 37(4), 555–570. https://doi.org/10.1093/esr/jcab001
Compans, M.-C., & Beaujouan, É. (2022). From union formation to first birth : The role of age at first cohabitation in the transition to motherhood and fatherhood. Population (English Edition), 77(3), 411–436. https://doi.org/10.3917/popu.2203.0439
Compans, M.-C., Beaujouan, É., & Suero García, C. (2022). Later fertility and birth intervals: A comparison of progressions to a second child between Spain and France [poster]. European Population Conference 2022. https://epc2022.popconf.org/abstracts/210401
Esteve, A., & Treviño, R. (2019). The main whys and wherefores of childlessness in Spain. Perspectives Demogràfiques, 015, 1–4.
Fiori, F., Rinesi, F., & Graham, E. (2017). Choosing to remain childless? A comparative study of fertility intentions among women and men in Italy and Britain. European Journal of Population, 33, 319–350. https://doi.org/10.1007/s10680-016-9404-2
Fostik, A. L., Soto, M. F., Ciganda, D., & Ruiz Vallejo, F. (2021). Union instability and fertility: An international perspective. International population conference 2021 (IUSSP). https://ipc2021.popconf.org/abstracts/210412
Frejka, T. (2011). The role of contemporary childbearing postponement and recuperation in shaping period fertility trends. Comparative Population Studies, 36(4), 927–958. https://doi.org/10.4232/10.CPoS-2011-20en
Frejka, T., & Calot, G. (2001). Cohort reproductive patterns in low-fertility countries. Population and Development Review, 27(1), 103–132. https://doi.org/10.1111/j.1728-4457.2001.00103.x
Frejka, T., & Sardon, J.-P. (2006). First birth trends in developed countries: Persistent parenthood postponement. Demographic Research, 15, 147–180. https://doi.org/10.4054/DemRes.2006.15.6
Gemmill, A. (2018). From some to none? Fertility expectation dynamics of permanently childless women. Demography, 56(8), 129–149. https://doi.org/10.1007/s13524-018-0739-7
Gliozheni, O., Hambartsoumian, E., Strohmer, H., Kreuz-Kinderwunschzentrum, O., SPG, Petrovskaya, E., Tishkevich, O., Bogaerts, K., I-Biostat, C. W., Balic, D., Sibincic, S., Antonova, I., Vrcic, H., Ljiljak, D., Rezabek, K., Markova, J., Lemmen, J., Sõritsa, D., Gissler, M., Pelkonen, S., et al. (2021). ART in Europe, 2017: Results generated from European registries by ESHRE. Human Reproduction Open, 2021(3). https://doi.org/10.1093/hropen/hoab026
Goisis, A., Håberg, S. E., Hanevik, H. I., Magnus, M. C., & Kravdal, Ø. (2020). The demographics of assisted reproductive technology births in a Nordic country. Human Reproduction, 35(6), 1441–1450. https://doi.org/10.1093/humrep/deaa055
Goldstein, J. R., Kreyenfeld, M., Jasilioniene, A., & Örsal, D. K. (2013). Fertility reactions to the ‘great recession’ in Europe: Recent evidence from order-specific data. Demographic Research, 29(July), 85–104. https://doi.org/10.4054/DemRes.2013.29.4
Gray, E., Evans, A., & Reimondos, A. (2013). Childbearing desires of childless men and women: When are goals adjusted? Advances in Life Course Research, 18(2), 141–149. https://doi.org/10.1016/j.alcr.2012.09.003
Greil, A. L. (1997). Infertility and psychological distress: A critical review of the literature. Social Science and Medicine, 45(11), 1679–1704. https://doi.org/10.1016/S0277-9536(97)00102-0
Guzzo, K. B., & Hayford, S. R. (2023). Evolving fertility goals and behaviors in current U.S. Childbearing cohorts. Population and Development Review, online fir. doi:https://doi.org/10.1111/padr.12535.
Hart, R. K. (2019). Union histories of dissolution: What can they say about childlessness? European Journal of Population, 35(1), 101–131. https://doi.org/10.1007/s10680-018-9464-6
Heiland, F., Prskawetz, A., & Sanderson, W. C. (2008). Are individuals’ desired family sizes stable? Evidence from west German panel data. European Journal of Population – Revue Européenne de Démographie, 24(2), 129–156. http://www.springerlink.com/index/10.1007/s10680-008-9162-x
Human Fertility Database. (2022). Max Planck Institute for Demographic Research (Germany) and Vienna Institute of Demography (Austria). https://www.humanfertility.org
Jalovaara, M., & Fasang, A. E. (2017). From never partnered to serial cohabitors: Union trajectories to childlessness. Demographic Research (Descriptive Findings), 36, 1703–1720. https://doi.org/10.4054/DemRes.2017.36.55
Kocourková, J., & Šťastná, A. (2021). The realization of fertility intentions in the context of childbearing postponement: Comparison of transitional and post-transitional populations. Journal of Biosocial Science, 53(1), 82–97. https://doi.org/10.1017/S002193202000005X
Kocourkova, J., Burcin, B., & Kucera, T. (2014). Demographic relevancy of increased use of assisted reproduction in European countries. Reproductive Health, 11. https://doi.org/10.1186/1742-4755-11-37
Kohler, H.-P., & Ortega, J. A. (2002). Tempo-adjusted period parity progression measures: Assessing the implications of delayed childbearing for cohort fertility in Sweden, The Netherlands and Spain. Demographic Research, 6, 145–190. https://doi.org/10.4054/DemRes.2002.6.7
Kohler, H.-P., Billari, F. C., & Ortega, J. A. (2002). The emergence of lowest-low fertility in Europe during the 1990s. Population and Development Review, 28(4), 641–680. https://doi.org/10.1111/j.1728-4457.2002.00641.x
Lazzari, E. (2021). Projecting the contribution of assisted reproductive technology to completed cohort fertility. YSSP Report. https://pure.iiasa.ac.at/id/eprint/17686/
Lazzari, E., Gray, E., & Chambers, G. M. (2021). The contribution of assisted reproductive technology to fertility rates and parity transition: An analysis of Australian data. Demographic Research, 45(November), 1081–1096. https://doi.org/10.4054/DEMRES.2021.45.35
Leridon, H. (2004). Can assisted reproduction technology compensate for the natural decline in fertility with age? A model assessment. Human Reproduction, 19(7), 1548–1553. https://doi.org/10.1093/humrep/deh304
Leridon, H. (2017). Biological effects of first birth postponement and assisted reproductive technology on completed fertility. Population, 72(3), 445–472. https://doi.org/10.3917/popu.1703.0463
Leridon, H., & Slama, R. (2008). The impact of a decline in fecundity and of pregnancy postponement on final number of children and demand for assisted reproduction technology. Human Reproduction, 23(6), 1312–1319. https://doi.org/10.1093/humrep/den106
Lesthaeghe, R. J. (2016). Following the evolution of fertility in second demographic transition settings: The life-cycle sensitive approach. In H. De Grande & H. Vandenheede (Eds.), Back to the roots of demography (pp. 105–114). ZenonPlus.
Letherby, G. (2002). Childless and bereft? Stereotypes and realities in relation to ‘voluntary’ and ‘involuntary’ childlessness and womanhood. Sociological Inquiry, 72(1), 7–20. https://doi.org/10.1111/1475-682X.00003
Lima, E. E. C., Zeman, K., Sobotka, T., Nathan, M., & Castro, R. (2018). The emergence of bimodal fertility profiles in Latin America. Population and Development Review, 0(1), 1–2. https://doi.org/10.1111/padr.12157
Luppi, F., Arpino, B., & Rosina, A. (2020). The impact of COVID-19 on fertility plans in Italy, Germany, France, Spain, and the United Kingdom. Demographic Research, 43(47), 1399–1412. https://doi.org/10.4054/DemRes.2020.43.47
Matysiak, A., Sobotka, T., & Vignoli, D. (2020). The great recession and fertility in Europe: A sub-national analysis. European Journal of Population, 37, 29–64. https://doi.org/10.1007/s10680-020-09556-y
Meggiolaro, S., & Ongaro, F. (2010). The implications of marital instability for a woman’s fertility: Empirical evidence from Italy. Demographic Research, 23, 963–996. https://doi.org/10.4054/DemRes.2010.23.34
Mencarini, L., Vignoli, D., Zeydanli, T., & Kim, J. (2018). Life satisfaction favors reproduction. The universal positive effect of life satisfaction on childbearing in contemporary low fertility countries. PLoS One, 13(12), 1–19. https://doi.org/10.1371/journal.pone.0206202
Mikolai, J. (2017). Partnership histories and the transition to motherhood in later reproductive ages in Europe. Population (English Edition), 72(1), 123–154. https://doi.org/10.3917/popu.1701.0127
Mills, M. C., Rindfuss, R. R., Mcdonald, P., Velde, E. T., & Force, E. R. S. T. (2011). Why do people postpone parenthood? Reasons and social policy incentives. Human Reproduction Update, 17(6), 848–860. https://doi.org/10.1093/humupd/dmr026
Moreau, C., Bouyer, J., Ducot, B., Spira, A., & Slama, R. (2010). When do involuntarily infertile couples choose to seek medical help? Fertility and Sterility, 93(3), 737–744. https://doi.org/10.1016/j.fertnstert.2008.10.011
Morgan, S. P. (2003). Is low fertility a twenty-first-century demographic crisis? Demography, 40(4), 589–603. https://doi.org/10.1353/dem.2003.0037
Mynarska, M., & Wróblewska, W. (2017). The health of women of reproductive age and their childbearing intentions. Zdrowie Publiczne i Zarządzanie, 15(2), 135–143. https://doi.org/10.4467/20842627oz.17.014.6784
Nathan, M., & Pardo, I. (2019). Fertility postponement and regional patterns of dispersion in age at first birth: Descriptive findings and interpretations. Comparative Population Studies, 44, 37–60. https://doi.org/10.12765/CPoS-2019-07en
Neels, K., & De Watcher, D. (2010). Postponement and recuperation of Belgian fertility: How are they related to rising female educational attainment? Vienna Yearbook of Population Research, 8, 77–106. https://doi.org/10.1553/populationyearbook2010s77
Neels, K., Theunynck, Z., & Wood, J. (2012). Economic recession and first births in Europe: Recession-induced postponement and recuperation of fertility in 14 European countries between 1970 and 2005. International Journal of Public Health, 58(1), 43–55. https://doi.org/10.1007/s00038-012-0390-9
Neels, K., Murphy, M., Ní Bhrolcháin, M., & Beaujouan, É. (2017). Rising educational participation and the trend to later childbearing. Population and Development Review, 43(4), 667–693. https://doi.org/10.1111/padr.12112
Ní Bhrolcháin, M. (1992). Period paramount? A critique of the cohort approach to fertility. Population and Development Review, 18(4), 599–629. https://doi.org/10.2307/1973757
Ní Bhrolcháin, M., & Beaujouan, É. (2012). Fertility postponement is largely due to rising educational enrolment. Population Studies, 66(3), 311–327. https://doi.org/10.1080/00324728.2012.697569
Ní Bhrolcháin, M., & Beaujouan, É. (2019). Do people have reproductive goals? Constructive preferences and the discovery of desired family size. In R. Schoen (Ed.), Analytical family demography (pp. 27–56). Springer. https://doi.org/10.1007/978-3-319-93227-9_3
Ní Bhrolcháin, M., & Toulemon, L. (2005). Does postponement explain the trend to later childbearing in France? Vienna Yearbook of Population Research, 83–107.
Ní Bhrolcháin, M., Beaujouan, É., & Murphy, M. (2011). Sources of error in reported childlessness in a continuous British household survey. Population Studies, 65(3), 305–318. https://doi.org/10.1080/00324728.2011.607901
Nicoletti, C., & Tanturri, M. L. (2008). Differences in delaying motherhood across European countries: Empirical evidence from the ECHP. European Journal of Population – Revue Européenne de Démographie, 24(2), 157–183. https://doi.org/10.1007/s10680-008-9161-y
Nishikido, M., Cui, Q., & Esteve, A. (2022). Partnership dynamics and the fertility gap. Genus, 78, 1–20. https://doi.org/10.1186/s41118-022-00170-w
Olsen, J. R. N., Basso, O., Spinelli, A., & Kuppers-chinnow, M. (1998). Correlates of care seeking for infertility treatment in Europe. European Journal of Public Health, 8, 15–20.
Passet-Wittig, J., & Bujard, M. (2021). Medically assisted reproduction in developed countries: Overview and societal challenges. In N. F. Schneider & M. Kreyenfeld (Eds.), Research handbook on the sociology of the family (pp. 417–438). Elgar Online. https://doi.org/10.4337/9781788975544.00039
Pifarré i Arolas, H. (2017). A cohort perspective of the effect of unemployment. Journal of Population Economics, 30, 1211–1239. https://doi.org/10.1007/s00148-017-0640-5
Rainer, H., Selvaretnam, G., & Ulph, D. (2011). Assisted reproductive technologies (ART) in a model of fertility choice. Journal of Population Economics, 24(3), 1101–1132. https://doi.org/10.1007/s00148-010-0320-1
Rallu, J.-L., & Toulemon, L. (1994). Period fertility measures: The construction of different indices and their application to France, 1946-89. Population, an English Selection, 6, 59–130. https://www.jstor.org/stable/pdf/2949144.pdf
Régnier-Loilier, A. (2006). Influence of own Sibship size on the number of children desired at various times of life. The Case of France. Population (English Edition), 61(3), 165–194. https://doi.org/10.3917/popu.603.0193
Rondinelli, C., Aassve, A., & Billari, F. C. (2006). Socio-economic differences in postponement and recuperation of fertility in Italy: Results from a multi-spell random effect model. ISER working paper, Article 2006–46.
Rondinelli, C., Aassve, A., & Billari, F. C. (2010). Women’s wages and childbearing decisions: Evidence from Italy. Demographic Research, 22, 549–578. https://doi.org/10.4054/DemRes.2010.22.19
Rybińska, A., & Morgan, S. P. (2019). Childless expectations and childlessness over the life course. Social Forces, 97(4), 1571–1602. https://doi.org/10.1093/sf/soy098
Saarela, J., & Skirbekk, V. (2019). Childlessness and union histories: Evidence from Finnish population register data. Journal of Biosocial Science, 2020, 78–96. https://doi.org/10.1017/S0021932019000257
Schnor, C. (2022). Single mothers by choice? Trends in single mothers’ socio-economic profiles and mode of conception in Belgium, 1996-2020. European Population Conference, 2022. https://epc2022.eaps.nl/abstracts/210294
Schoen, R. (2004). Timing effects and the interpretation of period fertility. Demography, 41(4), 801–819. http://www.ncbi.nlm.nih.gov/pubmed/15622955
Schoen, R., Astone, N. M., Kim, Y. J., Nathanson, C. A., & Fields, J. M. (1999). Do fertility intentions affect fertility behavior? Journal of Marriage and the Family, 61(3), 790–799.
Sobotka, T. (2017). Childlessness in Europe: Reconstructing long-term trends among women born in 1900-1972. In M. Kreyenfeld & D. Konietzka (Eds.), Childlessness in Europe: Contexts, causes, and consequences (pp. 17–53). Springer.
Sobotka, T. (2021). World’s highest childlessness levels in East Asia. Population & Societies, 595, 1–4. https://www.ined.fr/fichier/s_rubrique/32255/595_ang.en.pdf
Sobotka, T., & Beaujouan, É. (2014). Two is best? The persistence of a two-child family ideal in Europe. Population and Development Review, 40(3), 391–419. http://onlinelibrary.wiley.com/doi/10.1111/j.1728-4457.2014.00691.x/abstract
Sobotka, T., & Beaujouan, É. (2018). Late motherhood in low-fertility countries: Reproductive intentions, trends and consequences. In D. Stoop (Ed.), Preventing age related fertility loss (pp. 11–29). Springer International Publishing Switzerland.
Sobotka, T., & Berghammer, C. (2021). Demography of family change in Europe. In N. F. Schneider & M. Kreyenfeld (Eds.), Research handbook on the sociology of the family (pp. 162–186). Elgar Online. https://doi.org/10.4337/9781788975544
Sobotka, T., & Toulemon, L. (2008). Changing family and partnership behaviour: Common trends and persistent diversity across Europe. Demographic Research, 19(Special Collection 7), 85–138.
Sobotka, T., Hansen, M. A., Jensen, T. K., Pedersen, A. T., Lutz, W., & Skakkebæk, N. E. (2008). The contribution of assisted reproduction to completed fertility: An analysis of Danish data. Population and Development Review, 34(1), 79–101.
Sobotka, T., Zeman, K., Lesthaeghe, R. J., Frejka, T., & Neels, K. (2011). Postponement and recuperation in cohort fertility: Austria, Germany and Switzerland in a European context. Comparative Population Studies, 36(2–3), 417–452. https://doi.org/10.4232/10.CPoS-2011-16en
Tanturri, M. L., & Mencarini, L. (2008). Childless or childfree? Paths to voluntary childlessness in Italy. Population and Development Review, 34(1), 51–77. http://onlinelibrary.wiley.com/doi/10.1111/j.1728-4457.2008.00205.x/abstract
te Velde, E. R., Habbema, J. D. F., Leridon, H., & Eijkemans, M. J. C. (2012). The effect of postponement of first motherhood on permanent involuntary childlessness and total fertility rate in six European countries since the 1970s. Human Reproduction, 27(4), 1179–1183. https://doi.org/10.1093/humrep/der455
Thomson, E., Winkler-Dworak, M., Spielauer, M., & Prskawetz, A. (2012). Union instability as an engine of fertility? A Microsimulation Model for France. Demography, 49(1), 175–195. https://doi.org/10.1007/s13524-011-0085-5
Toulemon, L., & Mazuy, M. (2001). Les naissances sont retardées mais la fécondité est stable. Population (French Edition), 56(4), 611–644.
Trinitapoli, J., & Yeatman, S. (2018). The flexibility of fertility preferences in a context of uncertainty. Population and Development Review, 44(1), 87–116. https://doi.org/10.1111/padr.12114
Van Bavel, J., Jansen, M., & Wijckmans, B. (2012). Has divorce become a pro-Natal Force in Europe at the turn of the 21st century? Population Research and Policy Review, 31(5), 751–775. https://doi.org/10.1007/s11113-012-9237-6
van de Wiel, L. (2020). The speculative turn in IVF: Egg freezing and the financialization of fertility. New Genetics and Society, 39(3), 306–326. https://doi.org/10.1080/14636778.2019.1709430
Wagner, M., Huinink, J., & Liefbroer, A. C. (2019). Running out of time? Understanding the consequences of the biological clock for the dynamics of fertility intentions and union formation. Demographic Research, 40, 1–26. https://doi.org/10.4054/DemRes.2019.40.1
Wilkins, E. (2019). Low fertility: A review of the determinants. UNFPA working paper series, 2, 54. https://www.unfpa.org/publications/low-fertility-review-determinants
Winkler-Dworak, M., Beaujouan, É., Di Giulio, P., & Spielauer, M. (2017). Union instability and fertility: A microsimulation model for Italy and Great Britain. VID working paper, 8/2017.
Winkler-Dworak, M., Beaujouan, É., Di Giulio, P., & Spielauer, M. (2019). Simulating family life courses: An application to Italy, Great Britain, and Norway. VID working paper, 08/2019. https://www.oeaw.ac.at/vid/publications/serial-publications/vid-working-papers/
Winkler-Dworak, M., Pohl, M., & Beaujouan, É. (2022). Scenarios of fertility postponement and associated cohort fertility levels. European Population Conference 2022. https://epc2022.eaps.nl/abstracts/210345
Wyns, C., De Geyter, C., Calhaz-Jorge, C., Kupka, M. S., Motrenko, T., Smeenk, J., Bergh, C., Tandler-Schneider, A., Rugescu, I., & Goossens, V. (2022). ART in Europe, 2018: Results generated from European registries by ESHRE. Human Reproduction Open, 2022, 1–20. https://doi.org/10.1093/hropen/hoac022
Zeman, K., Beaujouan, É., Brzozowska, Z., & Sobotka, T. (2018). Cohort fertility decline in low fertility countries: Decomposition using parity progression ratios. Demographic Research, 38, 651–690. https://doi.org/10.4054/DemRes.2018.38.25
Acknowledgments
I thank Bob Schoen and Brian Buh for stimulating discussions, Katja Köppen for feedback and Katie Bowen for language editing. This research was funded by the BIC.LATE grant from the European Research Council, European Union’s Horizon 2020 research and innovation programme, grant Agreement No 101001410. The Office for National Statistics provided access to the British General Household Survey series (originally constructed by the ESRC Centre for Population Change).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Beaujouan, E. (2023). Delayed Fertility as a Driver of Fertility Decline?. In: Schoen, R. (eds) The Demography of Transforming Families. The Springer Series on Demographic Methods and Population Analysis, vol 56. Springer, Cham. https://doi.org/10.1007/978-3-031-29666-6_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-29666-6_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-29665-9
Online ISBN: 978-3-031-29666-6
eBook Packages: Social SciencesSocial Sciences (R0)