Abstract
Imaging plays a key role in the assessment of blunt abdominal trauma patients since clinical examination has been shown unreliable in this setting. If ultrasound and conventional radiology are mainly used for the initial triage phase at the resuscitation bay (primary survey), CT has become the leading imaging tool to be systematically used in hemodynamically blunt abdominal stable patients. CT signs are now included in most of the classifications and grading organ systems used by the radiologists, the emergency physician, and the surgeons for both the diagnostic and the therapeutic management of these patients, in which angiographic interventional procedures also play a growing role (Pierre-Alexandre Poletti).
Abdominal pain is a common reason for presentation to the emergency department. Particularly given the fast-paced work environment and frequently nonspecific data from history and physical examination, medical imaging proves indispensable in guiding management of patients presenting with abdominal pain. While the number of conditions that may lead to abdominal pain are myriad, this portion of the chapter will begin with conditions divided by abdominal quadrants, followed by conditions that may present with more diffuse symptoms (Vincent M Mellnick).
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Computed tomography
- Multidetector
- Abdominal injury
- FAST
- Abdominal trauma
- Trauma
- Appendicitis
- Cholecystitis
- Diverticulitis
- Bowel obstruction
- Bowel ischemia
1.1 Trauma Part
Learning Objectives
-
To review the role and limitations of the various imaging modalities in the management of blunt abdominal trauma patients.
-
To review the imaging findings associated with blunt abdominal trauma.
-
To discuss the role of imaging in the grading systems used for the management of blunt abdominal trauma patients.
Key Points
-
Absence of free intraperitoneal fluid at FAST examination does not rule out a major traumatic visceral injury.
-
Abdominal CT protocols must include both arterial and porto-venous phases; they should be completed by delayed series if vascular or urinary tract injuries are seen on initial series.
-
Splenic post-traumatic pseudoaneurysms mandate angiographic embolization; they may develop 24–72 h after trauma.
1.1.1 Role of Imaging to Assess Blunt Abdominal Polytrauma (BAT) Patients
1.1.1.1 Primary Survey
In a patient admitted with a potential abdominal trauma, a normal clinical examination has been shown insufficient per se to rule out a major intra-abdominal injury [1]. An imaging method should therefore be systematically obtained. Based on the ATLS recommendations [2], a FAST (focused assessment with sonography for trauma) is immediately performed, in addition to pelvic X-Ray, for the initial triage of trauma patients. Six regions are classically examined at FAST: right upper quadrant, hepatorenal fossa (Morison’s pouch), left upper quadrant (subphrenic space), splenorenal recess, pelvis (Douglas recess), and pericardium.
Depiction of a large amount of free intraperitoneal fluid in a hemodynamically unstable patient will mandate immediate laparotomy, or CT examination in a stable patient. In a hemodynamically stable patient, a normal FAST examination along with a normal clinical examination are not sufficient to rule out a significant intra-abdominal injury [3]. Indeed, in addition to the well-known limitation of the clinical abdominal examination up to 34% of abdominal injury could be present without associated free fluid, 17% of them would eventually require surgery or angiography embolization [4]. Furthermore, FAST examination can miss a major retroperitoneal bleeding. In isolated minor abdominal trauma, there is no unanimously accepted criteria for systematically performing or not CT in the absence of free intraperitoneal fluid at FAST. It has been suggested that the addition of normal bedside imaging (chest and pelvis X-ray, FAST) normal blood tests and a normal clinical examination could be sufficient to safely discharge an alert patient without further observation or investigation [3]. However, only a minority of patients (<20%) with suspicion of blunt abdominal trauma fulfill these criteria. All other should undergo further investigations.
1.1.1.2 Secondary Survey
Abdominal CT imaging in a hemodynamically stable patient is usually obtained in the frame of a total body CT protocol (secondary survey). In spite of the fact that there is no consensus regarding an optimal CT protocol for polytrauma patients, most authors agree that unenhanced abdominal CT images are not recommended, and that arterial and portal venous phase should be systematically obtained for a better depiction of vascular lesions, using either two acquisitions [5] or one single acquisition with a split contrast bolus. Delayed series should systematically be obtained in case of suspicion of active bleeding on the initial series.
1.1.1.2.1 Imaging of Common Abdominal Traumatic Injuries
1.1.1.2.1.1 Intraperitoneal Fluid
Hemoperitoneum is the commonest CT sign to suggest an intra-abdominal organ injury. Rarely, hemoperitoneum can be associated to retroperitoneal organ traumatic lesions, classically kidney injuries (or pancreatic tail injuries) by fluid spreading through the splenorenal ligament. In the absence of active bleeding, hemoperitoneum has a density between 20 and 40 HU. At the direct contact of the lesion, clotted blood achieves a higher density (50–70 HU) which is referred to as the “sentinel clot sign.” This sign if often useful to identify the actual site of injury [6]. Free fluid without evident organ injury may be present at CT in 1–5% of trauma patients and does not always herald need for surgery.
1.1.1.2.1.2 Organ Injuries
In a consecutive series of trauma patients with positive CT for at least one intra-abdominal injury [7] the following organ were involved, by order of frequency: spleen (37%), liver (32%), urinary tract (15%), bowel and mesentery (11%), pancreas (3%), diaphragm (<1%).
1.1.1.2.1.3 Spleen Injuries
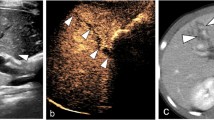
Spleen is the most frequently encountered organ injury in blunt abdominal trauma patients. Most splenic injuries can be treated conservatively, in the absence of absolute clinical indication for surgery at admission. However, delayed failure of nonsurgical treatment (bleeding) has been formerly reported in 10–31% of cases [8] and may occur up to 10 days (or even later) after trauma. A major improvement in the non-operative management of blunt splenic trauma patients was achieved when two major observations were reported in the scientific literature. Firstly, an association was established between the presence of intrasplenic vascular injuries at CT and an increased risk of delayed bleeding [9]. Secondly, the angiographic embolization of these vascular injuries has been associated with a significant drop in the rate of unsuccessful non-operative management (from 13% to 6%) [10]. Based on these observations, the classical AAST-1994 surgical splenic injury scale classification, only based on morphological criteria, was completed by a CT-based classification initially proposed by Stuart Mirvis [11] and slightly reshuffled in 2018 [12]. This classification takes into account vascular lesions (pseudoaneurysms, arteriovenous fistula or active bleedings) confined within the spleen (Fig. 1.1) and those extending beyond the spleen (active bleeding). Vascular splenic lesions appear at CT as focal blush of contrast with an attenuation close to arteries and greater than that of the spleen parenchyma. Delayed CT images must be systematically obtained in the presence of a vascular lesion to differentiate those that vanishes (pseudoaneurysms and arteriovenous fistula) from those which stay and expand (active bleeding).
Whether a systematic follow-up imaging patients should be performed in hemodynamically stable blunt splenic trauma patients remains a yet unsolved question. It has been reported that a majority of traumatic splenic pseudoaneuryms (38%–74%) would only be detected on control CT performed within 24–72 h after admission [13]. For practical reasons, most of the trauma associations do not recommend a systematic delayed CT in hemodynamically stable splenic trauma patients. With a reported 75% sensitivity and 100% specificity for detection of delayed splenic pseudoaneurysms (in skilled hands), bedside contrast enhanced sonographic examination has been advocated as a good option in this setting [14].
1.1.1.2.1.4 Liver Injuries
The AAST liver injury classification, as well as its adaptation for CT proposed by Stuart Mirvis in 1989, were based on the anatomic disruption of the liver, including the length and depth of the lacerations, as well as the size of the subcapsular hematoma.
Most of liver injuries, including high AAST grade lesions (III–V), can be managed non-operatively in hemodynamically stable patients. In 2018, the AAST-based liver grading system has been updated in a new organ injury scaling (OIS). The major change of the 2018 OIS is the inclusion of vascular lesions, confined in the liver parenchyma or freely bleeding into the peritoneum, to define severity. Such lesions are seen in about 20% of blunt liver trauma patients.
The most common ominous CT signs to be considered predictive of failure of non-operative management are the presence of an extracapsular bleeding into the peritoneal cavity, the extension of the laceration into the major hepatic veins or vena cava, and the presence of an important hemoperitoneum [15, 16]. Systematic routine follow-up CT is not recommended in blunt liver trauma patients; repeated imaging should only be guided by a patient’s clinical status. Bile duct injuries (biloma, biliary fistula, bile leak) have been reported as a complication in 2–8% of blunt liver trauma patients. MRI with biliary specific contrast agent may be used to identify the involvement of a main bile duct which could mandate surgical management. CT or ultrasound follow-up examination can be recommended in case of clinical suspicion of liver abscess that complicate liver trauma in about 4% of cases.
1.1.1.2.1.5 Urinary Tract Injuries
Urinary tract injuries are usually, but not always, associated with a gross hematuria. CT examination is the reference standard for the evaluation of the urinary tract. Arterial phases are important to demonstrate vascular kidney injuries while portal venous phases will better show parenchymal damage and differentiate an active bleeding from a pseudoaneurysm. The AAST classification for renal injuries has been slightly revised in 2018. Grade I to III renal injuries, the vast majority (75–98%) of renal traumatic lesions, do not involve the collecting system and are managed non-operatively. Any vascular injuries, including active bleeding, confined within the Gerota fascia are still considered grade III. Grade IV injuries extend into the collecting system or involve segmental renal vein or artery injuries (active bleeding or thrombosis) (Fig. 1.2). Grade 5 injuries refer to avulsion of the main renal artery or vein, a devascularized kidney with active bleeding or an extended maceration with loss of identifiable parenchyma. Surgical treatment or angiographic therapeutic management may be indicated in grade IV and V injuries. Any attempt of reperfusion of a devascularized kidney should be performed within 5 h after trauma to avoid irreversible ischemic damages.
Left renal artery injury (AAST Grade IV). 39 year-old man, admitted after a fall. Contrast enhanced CT, arterial phase (a), shows a thrombus occluding the renal artery (arrow) associated with an extended hypoperfusion of the renal cortex (arrowheads). Angiography coronal image (b) shows the site of the occlusion and the reperfusion (c) after stent placement (arrows)
Ureteral injury is exceedingly rare in blunt trauma and CT signs may be very subtle, such as mild periureteral fluid or fat stranding. A 3–20 min delayed excretory phase series are required to make the definitive diagnosis of partial or complete ureteral tear.
Bladder injuries are associated with pelvic fractures in 90% of cases, while about 2–11% of pelvic fracture have bladder rupture. Thus, a CT cystography should complete the initial CT series in the presence of a pelvic rim fracture, ideally by instilling at least 250 mL of diluted contrast media into the bladder. This technique has been reported 95% sensitive and 99% specific to detect a bladder rupture. It should not be performed if the patient requires angiography since the extravasated contrast material can obscure the sites of bleeding. Extravasation of vesical contrast material in the extraperitoneal tissues, including the prevesical space of Retzius, is characteristic of extraperitoneal bladder rupture [17]. This is the most frequent type (80%) of bladder rupture in adult patients, which can be treated by transurethral or suprapubic bladder catheterization. Spreading of contrast media into the peritoneal recesses is the hallmark of intraperitoneal bladder rupture, which account for about 20% of cases [17]. They require surgical repair to avoid peritonitis (Fig. 1.3). Rarely, both intra- and extraperitoneal bladder ruptures may coexist.
Extraperitoneal and intraperitoneal bladder rupture. (a) Axial CT-cystographic image obtained after retrograde instillation of 250 mL of contrast media inside the bladder (b) through the urinary catheter, in a patient with pelvic fracture (not shown). Contrast media is spilling along the extraperitoneal lateral borders of the bladder (arrows). b) Delayed coronal image reformation obtained 10 min after completion of a contrast-enhanced abdominal CT in another patient shows a leak of contrast media from the dome of the bladder (arrow) spreading into the intraperitoneal spaces (stars)
1.1.1.2.1.6 Bowel and Mesenteric Injuries
CT signs of bowel and mesenteric injuries may be subtle and often require a meticulous analysis for not being overlooked. Delay in assessing the diagnosis of these conditions is associated with a high morbidity due to peritonitis, sepsis, hemorrhage, or bowel ischemia. Most traumatic bowel injuries involve the small bowel, especially the proximal jejunum and the distal ileum. The transverse colon is the most frequent site of large bowel traumatic injuries. Some CT signs of bowel injuries are usually very specific but few sensitive to assess the diagnosis of bowel rupture: discontinuity of the bowel wall (rare), intra- or retroperitoneal air without other reason to explain this air, segmental absence of enhancement (devascularization). Some nonspecific signs, such as segmental bowel thickening or free intraperitoneal fluid, unexplained by a solid organ injury, should alert for a potential bowel perforation.
However, an extended diffuse small bowel circumferential hyper-enhanced wall thickening is more suggestive of a shock bowel syndrome (hypoperfusion complex), especially in the presence of a flat vena cava, enhanced adrenal grands, and delayed nephrograms. A diffuse small bowel wall thickening (without hyperenhancement), along with a dilated vena cava, is classically observed after a vigorous resuscitation (volume overload). An update of the AAST-bowel and mesentery classification, including the recent advances in CT imaging has been recently released [18].
If a bowel injury is clinically suspected in the absence of clear CT signs of bowel rupture, a follow-up CT can be performed 4–6 h later, after admission of i.v. and oral contrast to look for an extravasation of intra-intestinal contrast material.
CT signs suggestive of mesenteric injuries consist in an active extravasation of contrast media from mesenteric vessels (Fig. 1.4), a mesenteric hematoma adjacent to a bowel wall thickening (devascularization), an abrupt termination (or a vascular beading) of mesenteric vessels, or in the presence of a high density fan-shaped interloop fluid. The two former signs are usually associated with the need for surgery [19].
1.1.1.2.1.7 Diaphragmatic Injuries
Diaphragmatic injuries are quite rare and can often be overlooked at admission CT, especially on the right side, where the sensitivity of CT has been reported as low as 50% (vs 78% on the left). Right-sided diaphragmatic injuries are associated with a worst outcome than the left-sided ones since they are usually encountered at higher trauma forces and associated with major liver laceration. CT signs of diaphragm rupture classically include a disruption of the diaphragm and the herniation of abdominal content into the chest, usually the liver on the right side and various intraperitoneal structures on the left (stomach, bowel, fat, spleen), associated with a cardiomediastinal shift on the contralateral side (Fig. 1.5). A direct contact of these structures on the posterior chest wall is referred to as “the dependent viscera sign.” Since many nontraumatic situations may mimic a diaphragmatic injury, such as a gastric distention, a phrenic nerve paresis, and a congenital hernia, identification of a constricted area of the ascended structure (“collar sign”) will be helpful to assert the diagnosis of a diaphragmatic rupture [20].
Left hemidiaphragm rupture with organs herniation. A 29-year-old man admitted after a severe motor vehicle collision. Axial contrast-enhanced CT image (a) shows a discontinuity and thickening of the left hemidiaphragm (arrow) with a posterior displacement of the spleen (star), abutting the thoracic wall (dependent visceral sign). Coronal reformation image (b) shows the herniation of the stomach (S), the large bowel (B), and the spleen (SP), through a large diaphragmatic rent (arrows)
1.1.1.2.1.8 Pancreatic Injuries
Due to its protected location in the retroperitoneal space, the pancreas is relatively rarely injured in blunt abdominal trauma. Abdominal CT is the standard diagnostic tool to assess pancreatic injury but is often falsely negative at admission. A progressive elevation of serum amylase and lipase should alert towards a potential pancreatic injury that could have been missed at initial CT and justify a repeat evaluation by CT, 24–48 h after trauma. The 5 grades AAST-pancreatic injury scale is based on the extent of the injury and on the presence and location of a duct injury (Grade III to IV). The involvement of the pancreatic duct is important to be assessed by imaging because of its implication on the patients’ management (Fig. 1.6). A distal duct injury (Grade III, to the left of the superior mesenteric artery), when partial, may still be treated by drainage while a proximal duct injury usually requires surgery [21]. Unless CT shows a completely transected pancreas, the integrity of the main pancreatic duct can often not be well demonstrated by this method and must be further investigated by magnetic resonance cholangiopancreatography (MRCP), usually with secretin. Endoscopic retrograde cholangiopancreatography (ERCP) still remains the reference standard diagnostic tool to confirm a pancreatic duct injury; it has been recently recommended for stent placement therapy that might reduce the need for surgical resection [22].
AAST Grade IV pancreatic injury. A 22-year-old man admitted after a motor bike accident. Contrast-enhanced CT axial image (a) shows a non-enhancing area through the pancreatic neck (arrowheads). MRI-cholangiopancreatogram (MRCP) coronal oblique image (b), performed a couple of days later, shows a complete transection of the main pancreatic duct (arrows), with extravasation of the pancreatic juice (star)
CT is also useful for depiction of post-traumatic complications, especially those associated with undetected pancreatic duct injuries that may be suggested by pseudocysts, duct dilatations, or signs of chronic pancreatitis.
Take-Home Messages
-
Knowledge of CT trauma grading systems plays a key role in the management of blunt abdominal trauma patients.
-
Depiction of vascular injuries on CT is important for the therapeutic and clinical follow-up of abdominal trauma patients.
-
While still limited in the current imaging armamentarium of the emergency radiologist, ultrasound with contrast agents and MRI have a looming role in the follow-up imaging and monitoring of blunt abdominal trauma patients.
1.2 Non-Traumatic Abdominal Pain
Learning Objectives
-
Identify the most common conditions to cause abdominal pain and their imaging appearance, grouped by quadrant.
-
Recognize acute conditions of the small and large bowel, including obstruction and ischemia.
-
Diagnose gynecologic conditions that may present with acute abdominal or pelvic pain.
Key Points
-
Chronic cholecystitis, xanthogranulomatous cholecystitis, and gangrenous cholecystitis may create a diagnostic challenge for interpreting radiologists, demanding knowledge of these entities.
-
CT allows for localization of a transition point when the small or large bowel is obstructed. Adhesions and malignancy are the most common cause of obstruction of the small and large bowel, respectively.
-
Small bowel ischemia and ischemic colitis are different diseases on the same spectrum and have often disparate causes, imaging appearance, and prognosis.
1.2.1 Modalities
Ultrasound is a useful first line test for right upper quadrant and flank pain as well as for evaluating potential gynecologic sources of abdominal pain. However, it is operator-dependent and may not be available at all centers at all hours of the day.
CT is truly the workhorse modality in the emergency department. Typically, intravenous contrast is indicated, unless clinical suspicion is high for renal colic or if there is a compelling contra-indication to contrast. While often a single, portal venous phase of contrast enhancement is obtained, arterial and venous phases may be acquired if gastrointestinal bleeding or bowel ischemia is suspected clinically. A pre-contrast scan or virtual non-enhanced series may be helpful in this setting as well.
MRI is often precluded in the evaluation of abdominal pain due to the acuity of emergency care, concerns regarding exam length, and potential for limited availability. However, it may play a role in stable patients, including pregnant patients and those with known inflammatory bowel disease.
1.2.2 Right Upper Quadrant
1.2.2.1 Acute Cholecystitis
When a patient presents with right upper quadrant pain, gallbladder pathology—specifically gallstones and/or cholecystitis—are often the first diagnosis considered by both clinicians and radiologists. This diagnosis can be made on multiple modalities, including CT and MRI, but frequently ultrasound is employed as a first line test. Findings of acute cholecystitis include a distended gallbladder, typically with associated sludge and/or stones, surrounding inflammation, and a sonographic Murphy’s sign.
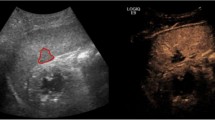
The diagnosis of acute cholecystitis may be more difficult in patients with superimposed chronic cholecystitis, in which case the gallbladder may be contracted rather than distended. Gangrenous cholecystitis may present with intramural gas and potentially a lack of Murphy’s sign. As it may lead to perforation, an early diagnosis is important and is suggested by the presence of mucosal defects or frank wall discontinuity (Fig. 1.7). Xanthogranulomatous variant of cholecystitis can be difficult to differentiate from gallbladder cancer but is suggested by the presence of lipid-containing spaces in the thickened gallbladder wall [23].
Gangrenous cholecystitis. A 82-year-old man with 2-week history of right upper quadrant pain. Ultrasound images show layering sludge and stones with subtle echogenic reflectors (a, arrows) representing intramural gas. There is also a contour abnormality of the gallbladder fundus with mucosal discontinuity (b, arrows), consistent with a walled off perforation
1.2.2.2 Duodenal Ulcers
The most frequent site of peptic ulcer disease is the duodenal bulb, which may project into the hepatic hilum near the gallbladder. Given this proximity, inflammation of the duodenum may be mistaken for acute cholecystitis or cholangitis. The imaging findings of a peptic ulcer include duodenal wall thickening and adjacent fat stranding with a mucosal defect and outpouching [24]. When the duodenal bulb perforates, free retroperitoneal or intraperitoneal air and paraduodenal fluid may be seen. Chronically, duodenal ulcers may cause strictures and gastric outlet obstruction.
Notably, when peptic ulcers occur distal to the duodenal bulb (post-bulbar), consideration should be given to the possibility of Zollinger-Ellison syndrome, caused by a gastrin-secreting tumor [25]. Crohn disease involving the duodenum may also cause post-bulbar duodenal ulcers. Importantly, perforation of the post-bulbar duodenum typically presents with retroperitoneal gas and/or fluid collections in contrast to the intraperitoneal duodenal bulb.
One diagnosis that may mimic duodenal ulcers is that of groove pancreatitis (“cystic degeneration of the duodenum.”) Thought to occur due to inflammation of intramural pancreatic rests, groove pancreatitis typically manifests with inflammation and cysts along the medial wall of the duodenum near its interface with the pancreas [26]. Chronic groove pancreatitis may result in strictures of the duodenum and/or distal common bile duct.
1.2.3 Left Upper Quadrant
1.2.3.1 Acute Pancreatitis
Acute pancreatitis is frequently considered in the patient presenting with left upper quadrant pain. CT is often the initial imaging modality to assess for complications of pancreatitis, including intrapancreatic and peripancreatic necrosis as well as fluid collections. Particularly when evaluating for parenchymal necrosis and vascular complications, intravenous contrast is useful. MRI may aid in characterizing ductal anatomy and detecting obstructing masses. Potential pitfalls in the diagnosis of acute pancreatitis include atypical cases such as from autoimmune inflammation. These patients present with less severe inflammation, a smooth “sausage” appearance to the pancreas, elevated IgG4 levels, and potentially other autoimmune findings such as nephritis [27]. Ultimately in both typical and autoimmune pancreatitis, imaging follow-up may prove useful in evaluating for an underlying neoplasm.
1.2.3.2 Gastritis
The stomach can become inflamed due to a variety of insults. Common examples include nonsteroidal anti-inflammatory medications, Helicobacter pylori infection, and alcohol. Imaging findings include mucosal hyperemia, submucosal edema, and perigastric fat stranding. When determining abnormal thickening of the gastric wall, care must be taken to account for gastric distention. A collapsed stomach may appear to be abnormally thick, particularly the gastric antrum which has a more muscular wall and is more peristaltic than other portions of the stomach. Similar to the duodenum, inflammation may be accompanied by ulcers, manifesting a focal outpouching, potentially with signs of perforation and/or bleeding (Fig. 1.8).
Gastric ulcer. A 56-year-old man with epigastric pain and hematemesis. Axial (a) and coronal (b) CT images show a large outpouching from the posterior lesser curvature with surrounding wall thickening, consistent with a peptic ulcer. Note the high attenuation material in the ulcer crater (arrows). This active bleeding was confirmed endoscopically
1.2.4 Right Lower Quadrant Pain
1.2.4.1 Acute Appendicitis
Acute appendicitis is the most common cause of a surgical emergency in the right lower quadrant. Imaging has substantially decreased negative appendectomy rates and is performed with CT in many settings. However, ultrasound and/or MRI may be used in young or pregnant patients to avoid exposure to ionizing radiation. Findings on all three modalities include a dilated, fluid-filled appendix more than 6 mm in diameter with surrounding inflammation. In addition to providing a diagnosis of acute appendicitis, imaging can also stratify patients into non-operative management and identify complications. For instance, gangrenous appendicitis may present with decreased mucosal enhancement, intramural gas, and/or perforation. While most cases of appendicitis are caused by obstructing appendicoliths, appendicitis may occasionally be caused by tumors of the appendix or cecal base [28].
1.2.4.2 Cecal Inflammation
Right-sided diverticula are more common in young patients and, when inflamed, may clinically mimic acute appendicitis. Cecal diverticulitis may also be confused for appendicitis on imaging as well, manifesting with a blind-ending structure with inflammation arising from the base of the cecum [29]. However, careful localization of a normal, typically longer appendix separate from the more rounded diverticulum is key to making this diagnosis and guiding the patient to what is often non-operative treatment. Other causes of primary cecal inflammation includes epiploic appendagitis. Although more often seen in the left colon, an inflamed oval, fat-containing mass along the surface of the cecum should suggest this diagnosis. In neutropenic patients, focal colitis (“neutropenic colitis” or “typhlitis”) can also present with localized inflammation in the right lower quadrant (Fig. 1.9). The clinical context and nondilated appendix may are important clues to this diagnosis.
1.2.4.3 Terminal Ileitis
The terminal ileum may become inflamed and clinically present similarly to acute appendicitis, often in the setting of Crohn disease. In this case, the inflammation usually manifests with asymmetric, nodular wall thickening with surrounding fat-stranding, potentially complicated by obstruction and/or penetrating disease. MRI may demonstrate increased T2 signal and diffusion restriction of the bowel wall in the acute phase. In addition to inflammatory bowel disease, the ileum may be inflamed due to infection, classically described with tuberculosis, Salmonella, and Yersinia species.
The terminal ileum may also become inflamed due to diverticulitis. This may occur due to acquired diverticula or Meckel diverticula, either of which may be a source of acute abdominal pain (Fig. 1.10). The key to this diagnosis is identifying a focal outpouching from the terminal ileum separate from the appendix surrounded by inflammation. Meckel diverticula may also present with intussusception, gastrointestinal bleeding, and volvulus of the small bowel [30].
Meckel diverticulitis. 28-year-old man with suspected appendicitis. Coronal CT image shows a thickened, inflamed terminal ileum, centered around a blind-ending structure in the right lower quadrant (arrows). This is separate from the normal appendix (dotted arrows) and was found to be a Meckel diverticulitis at surgery
1.2.5 Left Lower Quadrant Pain
1.2.5.1 Sigmoid Diverticulitis
Descending and/or sigmoid colon diverticulitis is one of most common causes of left lower quadrant abdominal pain. It manifests on imaging with an inflamed, rounded outpouching extending from the colon and may be complicated by bowel perforation and subsequent abscess formation. Chronically, fistulae may form from the colon to the adjacent bladder or other structures. Sometimes acute diverticulitis can appear mass-like and may be difficult to differentiate from malignancy. In such cases, the presence of lymphadenopathy is a feature more commonly seen in adenocarcinoma, whereas the presence of diverticula in the affected segment more strongly suggests diverticulitis [31]. Chronically, sigmoid diverticulitis results in muscular hypertrophy and potentially stenosis of the lumen.
1.2.5.2 Epiploic Appendagitis
Epiploic appendages are small pouches of peritoneal fat arising from subserosa of the colon, largest in size in the sigmoid region. They can be seen on CT primarily when they are surrounded by fluid, or when they become inflamed and/or infarcted after getting torsed resulting in epiploic appendagitis. The most common CT finding is small round or oval fat attenuation lesion abutting the colonic wall with surrounding inflammation. A central area of high attenuation is commonly seen representing a centrally thrombosed vessel.
1.2.5.3 Pelvic Pain: Endometriosis
Endometriosis is an important cause of infertility and chronic pelvic pain. In addition to the ovaries, endometrial implants can involve the sigmoid colon, rectum, and cul-de-sac and therefore cause left lower quadrant and pelvic pain. These implants can be complicated by bleeding, inflammation, and eventually fibrosis and adhesions [32]. The classic sonographic appearance of an endometrioma is a homogenous, hypoechoic lesion with thin walls and posterior acoustic enhancement demonstrating low-level internal echoes and no internal blood flow. MRI is very useful in detecting small implants. Endometriomas appear T1 hyperintense with corresponding low signal on T2-weighted imaging, referred to as “T2 shading.” However, CT may simply demonstrate inflammation surrounding a mass or ill-defined area of bowel wall thickening.
1.2.5.4 Ovarian Torsion
Ovarian torsion typically occurs in younger patients, commonly—although not necessarily—in the setting of an underlying mass. Imaging signs of a torsed ovary include ovarian enlargement, peripheralized follicles, a twisted ovarian vascular pedicle, deviation of the uterus towards the side of the torsion and surrounding inflammation. Ultrasound may show reduced or absent Doppler signal within a torsed ovary [33]. However, incomplete or intermittent torsion may result in a false-negative Doppler exam.
1.2.6 Diffuse Abdominal Pain
1.2.6.1 Small Bowel Obstruction
Small bowel obstruction (SBO) is a common cause of hospital admissions for abdominal pain. There are numerous causes of SBO, with adhesions representing the majority of cases. Other causes include inflammatory bowel disease, internal and external hernias, tumors, intussusception, volvulus, and foreign bodies. The classic symptoms for SBO include diffuse abdominal pain, abdominal distention, and vomiting. However, such symptoms and laboratory findings have limited sensitivity and specificity for diagnosing SBO.
Although radiography and fluoroscopic exams may play a role in the diagnosis of SBO, CT has become the mainstay of imaging when this clinical situation is suspected. This allows for identification of dilated (>3 cm) small bowel leading to a transition point for the obstruction and potentially an underlying cause. Depending on the severity of the obstruction, there may be abrupt decompression after the transition point. In addition, CT allows for identification of patients with complications or who are at risk for them. One such example is patients with closed loop obstruction, in which both the inlet and outlet of an obstructed bowel segment are compressed, often by a single source, like an adhesion or hernia neck [34] (Fig. 1.11).
Closed loop small bowel obstruction. A 43-year-old woman with abdominal pain and vomiting. Axial CT demonstrates clustered, dilated loops of small bowel in the right upper quadrant. The inlet and outlet of the obstruction occur at the same point (arrows), a configuration concerning for closed-loop obstruction. An adhesion was the underlying cause
Ischemia complicating small bowel obstruction may manifest with nonspecific findings including bowel wall and mesenteric edema. Decreased bowel wall enhancement and intramural hemorrhage are more specific findings for ischemia in the setting of SBO. Extraluminal gas and/or well-defined fluid collections can be seen with perforation complicating SBO [35].
1.2.6.2 Colonic Obstruction
In contrast to SBO, colonic tumors are the most common cause of large bowel obstruction [36] (Fig. 1.12). Obstructing colon cancers are more common on the left than on the right, likely due to the progressively narrower lumen distally. Although most commonly seen with primary colonic adenocarcinoma, direct invasion from another primary tumor or extrinsic metastatic involvement of the colon may also result in intestinal obstruction. On CT, obstructing colon tumors result a mass with soft tissue attenuation in the submucosa as well as other evidence of malignancy, including lymphadenopathy and metastases.
Large bowel obstruction due to colon cancer. A 60-year-old man with abdominal distention. Axial CT shows a soft tissue mass at the splenic flexure (arrows) causing marked dilatation of the transverse colon. The patient underwent colonic stent placement, confirming an obstructing adenocarcinoma. Note metastases in the inferior right liver
After malignancy, colonic volvulus is the second most common cause of colonic obstruction. This most commonly occurs in the cecum and sigmoid colon. Cecal volvulus results from increased mobility and twisting of the proximal ascending colon. In addition to twisting of the proximal colon, cecal obstruction can also result from anterior folding of the cecum relative to the ascending colon, the so-called cecal bascule.
Closed loop obstruction of the sigmoid classically occurs in elderly patients, and often those who are chronically debilitated and constipated. The most common site of colonic volvulus, sigmoid volvulus may be a chronic process of twisting and untwisting, resulting in an indolent presentation. Similar to cecal volvulus, CT may demonstrate the colonic closed loop obstruction with a twist or “whirl” sign in the sigmoid mesentery. As in volvulus of any segment of the bowel, prompt decompression—either endoscopic or surgical—is the mainstay of treatment [37].
1.2.6.3 Acute Mesenteric Ischemia
Acute mesenteric ischemia (AMI) is a rare but deadly disease process. The surgical literature states that arterial thromboembolic causes are most common, followed by nonocclusive and venous causes. However, the incidence of nonocclusive ischemia is likely underestimated. Clinical symptoms of AMI are nonspecific. Classically, the patient presents with sudden onset of severe abdominal pain out of proportion to the clinical exam. Elevated lactate and d-dimer levels can be seen but are nonspecific for AMI.
CT angiography with IV contrast is the recommended test of choice in adults with suspected acute mesenteric ischemia. However, many patients will be imaged with routine portal venous phase imaging because the diagnosis was not suspected clinically. MR angiography has high sensitivity and specificity for diagnosing AMI but is typically not used in the emergency setting due to availability and length of exam. Therefore, it is best reserved for patients with iodinated contrast allergies.
Classic and specific imaging findings for occlusive AMI include a filling defect in the mesenteric arteries, with associated hypoenhancing or non-enhancing bowel wall (Fig. 1.13). Gas within the small bowel—pneumatosis intestinalis—may be seen with other conditions but may be an ominous sign of bowel infarction. Other, more nonspecific, findings include mesenteric congestion, ascites, and bowel wall thickening. These findings are more commonly seen with venous ischemia and/or reperfusion [38].
Embolic small bowel ischemia. A 48 year-old woman with abdominal pain, elevated lactate. Axial CT shows a filling defect in the left ventricle (a, arrows). This has caused an embolism to the superior mesenteric artery (coronal CT b, arrows), resulting in small bowel ischemia. Note the hypoenhancing small bowel in the left upper quadrant (b, dotted arrows)
In contrast to small bowel ischemia, ischemic colitis is often caused by relatively mild episodes of hypotension. It is commonly self-limited but can manifest with full-thickness necrosis and peritonitis. While classically described in anatomic “water-shed” areas between major vascular beds, ischemic colitis can affect any portion of the colon. On imaging, ischemic colitis usually presents with wall thickening in more mild cases [39]. More severe cases can present with hypoenhancement, ileus, and pneumatosis.
Take-Home Messages
-
While cholecystitis is a common reason for right upper quadrant pain, consider alternative causes of inflammation in this location, including peptic ulcers and cholangitis.
-
Cecal diverticulitis and inflammation of the terminal ileum may mimic acute appendicitis, both clinically and radiologically.
-
Bowel ischemia may have a variety of appearances, depending on the cause, severity, and chronicity.
1.2.7 Concluding Remarks
Imaging is a mainstay in the emergency department, both in trauma and non-trauma settings. CT is often the workhorse modality in both situations, but ultrasound and MRI are useful in select clinical presentations and patient populations. Emergency and general radiologists should have familiarity with CT signs of hollow viscous and solid organ injuries and grade them to help guide clinical management. Likewise, radiologists should know common conditions—and their mimics—that occur in each quadrant of the abdomen as well as conditions that can appear in multiple locations.
References
Holmes JF, Wisner DH, McGahan JP, Mower WR, Kuppermann N. Clinical prediction rules for identifying adults at very low risk for intra-abdominal injuries after blunt trauma. Ann Emerg Med. 2009;54(4):575–84.
Kortbeek JB, Al Turki SA, Ali J, Antoine JA, Bouillon B, Brasel K, et al. Advanced trauma life support, 8th edition, the evidence for change. J Trauma. 2008;64(6):1638–50.
Poletti PA, Mirvis SE, Shanmuganathan K, Takada T, Killeen KL, Perlmutter D, et al. Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography? J Trauma. 2004;57(5):1072–81.
Shanmuganathan K, Mirvis SE, Sherbourne CD, Chiu WC, Rodriguez A. Hemoperitoneum as the sole indicator of abdominal visceral injuries: a potential limitation of screening abdominal US for trauma. Radiology. 1999;212(2):423–30.
Boscak AR, Shanmuganathan K, Mirvis SE, Fleiter TR, Miller LA, Sliker CW, et al. Optimizing trauma multidetector CT protocol for blunt splenic injury: need for arterial and portal venous phase scans. Radiology. 2013;268(1):79–88.
Hamilton JD, Kumaravel M, Censullo ML, Cohen AM, Kievlan DS, West OC. Multidetector CT evaluation of active extravasation in blunt abdominal and pelvic trauma patients. Radiographics. 2008;28(6):1603–16.
Poletti PA, Kinkel K, Vermeulen B, Irmay F, Unger PF, Terrier F. Blunt abdominal trauma: should US be used to detect both free fluid and organ injuries? Radiology. 2003;227(1):95–103.
Shackford SR, Molin M. Management of splenic injuries. Surg Clin North Am. 1990;70(3):595–620.
Gavant ML, Schurr M, Flick PA, Croce MA, Fabian TC, Gold RE. Predicting clinical outcome of nonsurgical management of blunt splenic injury: using CT to reveal abnormalities of splenic vasculature. AJR Am J Roentgenol. 1997;168(1):207–12.
Lee JT, Slade E, Uyeda J, Steenburg SD, Chong ST, Tsai R, et al. American Society of Emergency Radiology Multicenter Blunt Splenic Trauma Study: CT and clinical findings. Radiology. 2021;299(1):122–30.
Mirvis SE, Whitley NO, Gens DR. Blunt splenic trauma in adults: CT-based classification and correlation with prognosis and treatment. Radiology. 1989;171(1):33–9.
Kozar RA, Crandall M, Shanmuganathan K, Zarzaur BL, Coburn M, Cribari C, et al. Organ injury scaling 2018 update: spleen, liver, and kidney. J Trauma Acute Care Surg. 2018;85(6):1119–22.
Davis KA, Fabian TC, Croce MA, Gavant ML, Flick PA, Minard G, et al. Improved success in nonoperative management of blunt splenic injuries: embolization of splenic artery pseudoaneurysms. J Trauma. 1998;44(6):1008–13; discussion 13-5.
Poletti PA, Becker CD, Arditi D, Terraz S, Buchs N, Shanmuganathan K, et al. Blunt splenic trauma: can contrast enhanced sonography be used for the screening of delayed pseudoaneurysms? Eur J Radiol. 2013;82(11):1846–52.
Fang JF, Wong YC, Lin BC, Hsu YP, Chen MF. The CT risk factors for the need of operative treatment in initially hemodynamically stable patients after blunt hepatic trauma. J Trauma 2006;61(3):547–53; discussion 53–4.
Poletti PA, Mirvis SE, Shanmuganathan K, Killeen KL, Coldwell D. CT criteria for management of blunt liver trauma: correlation with angiographic and surgical findings. Radiology. 2000;216(2):418–27.
Gross JA, Lehnert BE, Linnau KF, Voelzke BB, Sandstrom CK. Imaging of urinary system trauma. Radiol Clin N Am. 2015;53(4):773–88. ix
Tominaga GT, Crandall M, Cribari C, Zarzaur BL, Bernstein M, Kozar RA, et al. Organ injury scaling 2020 update: bowel and mesentery. J Trauma Acute Care Surg. 2021;91(3):e73–e7.
Alabousi M, Mellnick VM, Kashef Al-Ghetaa R, Patlas MN. Imaging of blunt bowel and mesenteric injuries: current status. Eur J Radiol. 2020;125:108894.
Killeen KL, Mirvis SE, Shanmuganathan K. Helical CT of diaphragmatic rupture caused by blunt trauma. AJR Am J Roentgenol. 1999;173(6):1611–6.
Lin BC, Hwang TL. Resection versus drainage in the management of patients with AAST-OIS grade IV blunt pancreatic injury: a single trauma Centre experience. Injury. 2022;53(1):129–36.
Biffl WL, Ball CG, Moore EE, Lees J, Todd SR, Wydo S, et al. Don’t mess with the pancreas! A multicenter analysis of the management of low-grade pancreatic injuries. J Trauma Acute Care Surg. 2021;91(5):820–8.
O’Connor OJ, Maher MM. Imaging of cholecystitis. Am J Roentgenol. 2011;196(4):W367–W74.
Tonolini M, Ierardi AM, Bracchi E, Magistrelli P, Vella A, Carrafiello G. Non-perforated peptic ulcer disease: multidetector CT findings, complications, and differential diagnosis. Insights Imaging. 2017;8(5):455–69.
Davila A, Menias CO, Alhalabi K, Lall C, Pickhardt PJ, Lubner M, et al. Multiple endocrine neoplasia: spectrum of abdominal manifestations. AJR Am J Roentgenol. 2020;215(4):885–95.
Kim DU, Lubner MG, Mellnick VM, Joshi G, Pickhardt PJ. Heterotopic pancreatic rests: imaging features, complications, and unifying concepts. Abdom Radiol (NY). 2017;42(1):216–25.
Vlachou PA, Khalili K, Jang HJ, Fischer S, Hirschfield GM, Kim TK. IgG4-related sclerosing disease: autoimmune pancreatitis and extrapancreatic manifestations. Radiographics. 2011;31(5):1379–402.
Shademan A, Tappouni RF. Pitfalls in CT diagnosis of appendicitis: pictorial essay. J Med Imaging Radiat Oncol. 2013;57(3):329–36.
Pooler BD, Lawrence EM, Pickhardt PJ. Alternative diagnoses to suspected appendicitis at CT. Radiology. 2012;265(3):733–42.
Rossi P, Gourtsoyiannis N, Bezzi M, Raptopoulos V, Massa R, Capanna G, et al. Meckel’s diverticulum: imaging diagnosis. AJR Am J Roentgenol. 1996;166(3):567–73.
Gryspeerdt S, Lefere P. Chronic diverticulitis vs. colorectal cancer: findings on CT colonography. Abdom Imaging. 2012;37(6):1101–9.
Mason BR, Chatterjee D, Menias CO, Thaker PH, Siegel CL, Yano M. Encyclopedia of endometriosis: a pictorial rad-path review. Abdom Radiol (NY). 2020;45(6):1587–607.
Dawood MT, Naik M, Bharwani N, Sudderuddin SA, Rockall AG, Stewart VR. Adnexal torsion: review of radiologic appearances. Radiographics. 2021;41(2):609–24.
Elsayes KM, Menias CO, Smullen TL, Platt JF. Closed-loop small-bowel obstruction: diagnostic patterns by multidetector computed tomography. J Comput Assist Tomogr. 2007;31(5):697–701.
Scaglione M, Galluzzo M, Santucci D, Trinci M, Messina L, Laccetti E, et al. Small bowel obstruction and intestinal ischemia: emphasizing the role of MDCT in the management decision process. Abdom Radiol (NY). 2022;47(5):1541–55.
Verheyden C, Orliac C, Millet I, Taourel P. Large-bowel obstruction: CT findings, pitfalls, tips and tricks. Eur J Radiol. 2020;130:109155.
Wortman JR, Dhyani M, Ali SM, Scholz FJ. Pearls and pitfalls in multimodality imaging of colonic volvulus. Radiographics. 2020;40(4):1039–40.
Srisajjakul S, Prapaisilp P, Bangchokdee S. Comprehensive review of acute small bowel ischemia: CT imaging findings, pearls, and pitfalls. Emerg Radiol. 2022;29(3):531–44.
Taourel P, Aufort S, Merigeaud S, Doyon FC, Hoquet MD, Delabrousse E. Imaging of ischemic colitis. Radiol Clin N Am. 2008;46(5):909–24. vi
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Mellnick, V.M., Poletti, PA. (2023). Emergency Radiology of the Abdomen and Pelvis. In: Hodler, J., Kubik-Huch, R.A., Roos, J.E., von Schulthess, G.K. (eds) Diseases of the Abdomen and Pelvis 2023-2026. IDKD Springer Series. Springer, Cham. https://doi.org/10.1007/978-3-031-27355-1_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-27355-1_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-27354-4
Online ISBN: 978-3-031-27355-1
eBook Packages: MedicineMedicine (R0)