Abstract
Reconstruction of the facial skeleton is a complex task with multiple factors to consider. The rapid development of three-dimensional planning now allows surgeons to plan resection and reconstruction to a high degree of precision, with a number of associated benefits. This chapter discusses the indications and processes involved in three-dimensional planning and its application to surgical resection and reconstruction of the facial bones.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
Introduction
Head and neck reconstruction has undergone significant evolution over the last 20–30 years. This period has seen the development and rapid evolution of digital systems to aid in surgical planning and treatment. Three-dimensional (3D) planning, also referred to as virtual surgical planning (VSP) or computer aided design/computer aided manufacture (CAD/CAM), has evolved to allow surgeons to digitally plan resection and reconstruction to a high degree of precision. It then allows for the manufacture of adjuncts to surgery such as cutting guides and patient specific plates, which aim to reduce operative time and increase accuracy of reconstruction. Recent years have seen the exponential growth in the use of these systems with improvements in intra-operative time, ease of use and cost [1, 2].
Reconstruction of the facial skeleton is a complex task with a number of aims that the surgeon must consider. The primary aims are to restore form and function. The surgeon must attempt to reconstruct the complex geometry of the face so as to maintain the continuity of the jaws and also replicate the curvature of the arches where possible. The amount of osseous and soft tissue required and the potential for dental rehabilitation must be considered carefully. Any reconstruction must also attempt to restore the complex functional requirements of this region, namely speech, swallow and mastication. Other considerations include the final aesthetic result, the potential impact on quality of life for the patient and the ability of the reconstruction to withstand radiotherapy, if this is likely to be required.
Essential Steps
There are a number of essential steps required to achieve success in 3D planning. Firstly, accurate digital design is needed. A recent computed tomography (CT) scan in DICOM format with thin slices should be obtained. If planning will be used for both the ablative and reconstructive components, then a scan of the proposed donor bone is also necessary. Often the imaging will need to be ‘cleaned-up’ to remove artifacts. In the oral cavity, dental restorations may create significant scatter artifact and software systems may be needed to remove this.
Accurate planning is the next step to undertake. This should be multi-disciplinary in nature with the surgeon, technician and possibly restorative dentist involved. In modern practice most propriety companies will undertake these sessions virtually. If design and manufacture is undertaken ‘in-house’ then these sessions may be more frequent and also allow for rapid feedback and modification if required. Planning at this stage will consider the resection and surgical margins to be obtained as well as any involved or adjacent structures. Other issues that may need to be considered include how best to register cutting guides and the position of screws with regard to potential implant rehabilitation (Fig. 17.1).
Indications
When 3D planning was initially developed, its use was often limited to complex reconstruction cases. As recent years have seen a reduction in costs and manufacturing time, some units would now consider 3D planning for the majority, if not all, of their cases. The process remains most beneficial in complex defects of the maxilla and mandible, such as those requiring large amount of soft and hard tissue resection and/or multiple osteotomies of the donor flap. The process is also very beneficial when dental implant rehabilitation is planned. Short span mandibular and low-level maxillary defects may not require 3D planning but may still benefit from the improved accuracy possible in both resection and reconstruction, as discussed below.
Resection
The primary aim of ablative head and neck surgery is to remove any lesion with adequate histological margins. In oncological practice this will generally be a 1 cm surgical margin. Where possible, aesthetic units and vital structures should be preserved although this should not take precedence over oncological clearance. In the mandible, if resection margins are close to the condyle, a decision must be made on whether to preserve this segment or to incorporate it into the resection. 3D planning allows for the creation of specific cutting guides to accurately achieve the planned resection intraoperatively. The guides and planned resection margins may also allow for the potential of interval tumour growth between the planning stage and the actual time of surgical resection.
After the lesion is exposed intra-operatively, the custom guides are seated on the mandible or maxilla. The guides should be constructed so as to seat passively and directly adjacent to the bone and may have special locators to assist in this (Fig. 17.2). The guides may then also be secured with mono-cortical screws. The bony resection is then undertaken without concern for stabilising the bony remnants. If planned, the guides may also contain guide holes to be drilled to allow later screw placement for securing the reconstruction plates.
Mandibular Reconstruction
Composite free flap reconstruction is now the gold standard in mandibular reconstruction. When planning the reconstruction, the height and vertical position of the donor bone is a key consideration. A lower position along the mandibular border maximises form while a higher position near the alveolus will allow for easier implant placement and dental rehabilitation. Once the bony position is confirmed, a 3D model of the planned reconstruction can be printed and a plate contoured to this. The plate length is determined so as to ensure there are three screws on either side of the resection.
Intra-operatively, the pre-bent plate is seated onto the native mandible following resection using temporary localisation guides soldered to the plate. This ensures an accurate fit prior to placement on the donor bone. If the cutting guides did not contain guide holes, then the plate can be used to pre-drill screws holes at this time. The plate is then removed and the localisation guides removed. The plate is secured onto the donor bone with mono-cortical screws so as to avoid damage to the vascular pedicle on the deep aspect of the bone. Usually, two screws are placed per bony segment. The plate and flap reconstruction is then inset into the defect and secured using the pre-drilled holes and bi-cortical screws (Figs. 17.3 and 17.4).
There are a number of bony flaps that may be used for mandibular reconstruction. A number of considerations such as the quantity and quality of hard and soft tissue required, if dental implant placement is planned and the pedicle length required will help guide selection. The fibula free flap remains the work-horse flap of mandibular reconstruction for a number of reasons. Its lower limb location makes it easily accessible and permits two team operating thus shortening operative time. It is straightforward to raise, provides a significant length of bone and results in low levels of donor site morbidity. Importantly, it also allows for 3D planning and the construction of specific cutting guides (Fig. 17.5) [3]. Although the bone stock may be limited in vertical and cross-sectional dimensions, dental implant rehabilitation is usually possible. Other flaps that may be considered include the deep circumflex iliac artery (DCIA) flap, the composite scapula flap and the composite radial flap. All of these flaps have their own individual advantages and disadvantages with regard to mandibular reconstruction.
The DCIA flap provides good bone stock although the length of vascular pedicle is often a concern. A two-team approach is also permitted with this flap and although it may be raised as an osteo-cutaneous composite flap a myo-osseous flap utilising the internal oblique muscle is more commonly. Donor site morbidity is a concern with this flap and meticulous closure is required to minimise the risk of hernias. The composite scapula flap is often considered when large volumes of soft tissue is required in addition to bony reconstruction. The flap, based on the subscapular arterial system, may also be raised in a chimeric fashion to provide two or more reconstructive components. The composite radial free flap is less commonly used in mandibular reconstruction due to the limited amount of bone stock available and the potential for donor site morbidity.
Maxillary Reconstruction
Maxillary defects may create a number of issues that must be addressed when planning any reconstruction. There may be loss of vertical support with potential enophthalmos, orbital dystopia or reduced projection of the midface. Loss of horizontal support may also create issues with speech and swallow and may make the retention of prosthetic devices difficult. Maxillary defects are easily classified using the Brown classification system, which incorporates both vertical and horizontal components [4]. The vertical component is classified from class I to class V. Defects not creating an oro-antral defect and thus usually confined to the maxillary alveolus are referred to as class I. Class II defects have a more vertical extent that result in an oro-antral defect but do not involve the orbit. If the defect extends to include the orbital contents, but with orbital retention, it is referred to as class III and if orbital exenteration or enucleation is required, as class IV. Class V and VI refer to orbitomaxillary and nasomaxillary defects respectively. This system can also be used to guide reconstruction as some options are more suitable than others depending on the defect.
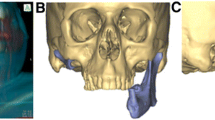
In a similar fashion to the mandible, 3D planning will usually involve the printing of models that allow for the fabrication of cutting guides and plates that are pre-bent for the planned reconstruction. We have previously published our approach to reconstructing maxillary defects [5]. In low level, class I and some class II, defects we recommend soft tissue reconstruction and the use of prosthetic obturators. For larger or anterior class II defects a strut of bone is often required and the use of a fibula or scapula flap may be a good option in these cases. Class III defects pose particular challenges with the loss of alveolar bone, the orbital floor and cheek support. No single flap can solve all of these issues but the DCIA flap with a custom orbital reconstruction plate is perhaps the best option. The DCIA flap can be harvested with a shape and contour that readily reconstructs the lost buttresses of the maxilla. 3D planning allows for the construction of specialised cutting guides to simplify harvest. Inset can then be achieved using a pre-bent plate and customised orbital floor reconstruction plate (Figs. 17.6, 17.7 and 17.8).
Class V (orbitomaxillary) and VI (nasomaxillary) defects are less common and pose different challenges. In class IV cases, the primary aim is to create a base on which to base a future prosthesis. There is no need to reconstruct the orbital floor however. Both the DCIA and scapula flap are good options to consider as they can provide good muscle bulk with which to fill the orbital defect. Reconstruction of class V defects requires only a small amount of bone and often the composite radial forearm free flap is a good option to utilise.
Limitations and Future Developments
While 3D planning clearly provides some advantages over conventional head and neck reconstructive surgery, there are some potential limitations and drawbacks. Firstly, there is a potential for surgeons to become reliant on these systems with a resultant loss in free hand skills. Although 3D planning aims to be highly accurate, there is always the potential for unexpected findings intra-operatively or problems with the hardware. In these scenarios the surgeon must be able to adapt and potentially revert to traditional techniques. Secondly, most current planning systems cannot account for soft tissue factors. In the past, cutting guides and hardware were bulkier and at times this posed problems in cases with a tight soft tissue envelope. Newer systems continue to adapt to this problem with lower profile guides and a move away from thicker metalwork. Finally, these systems can incur significant costs, both financially and in terms of time. Manufacturing costs may be significant although proponents of these systems point to the cost savings in reduced intra-operative time which some studies have reported [6, 7]. The use of ‘in-house’ planning and manufacture may also reduce costs significantly [8]. The time taken for planning and manufacture, and thus the potential for a delay in surgery, has been cited by some detractors of these systems in the past. As the technology has evolved, this concern has receded. Much if not all of the planning is now conducted virtually and manufacturing times have significantly improved. Indeed, recent studies have confirmed the oncological safety of this approach [9, 10].
The next decade is likely to see further refinements and progress in this field. Manufacturing time and costs are likely to reduce further as these systems gain widespread use. Although most current 3D planning focuses on bony reconstruction, future developments are likely to see a move towards soft tissue planning. The potential to plan soft tissue flaps based on the donor and recipient site vasculature would be a significant advantage and further evolution of this technique. Augmented reality is another rapidly emerging technology in surgery and may also play a role in head and neck reconstruction in future years [11, 12].
Conclusion
3D planning has evolved significantly in recent years and continues to do so. If a number of key principles are adhered to, it can allow for highly accurate resection and reconstruction of the facial bones. As more centres use these systems, further advancements in manufacture times, cost and planning ability are likely.
References
Miles BA, McMullen CP, Sweeny L, Zenga J, Ryan L, Divi V, et al. Practice patterns of virtual surgical planning: survey of the reconstructive section of the American Head and Neck Society. Am J Otolaryngol. 2022;439(1):103225.
Rodby KA, Turin S, Jacobs RJ, Cruz JF, Hasid VJ, Kolokythas A, et al. Advances in oncologic head and neck reconstruction: systematic review and future considerations of virtual surgical planning and computer aided design/computer aided modelling. J Plast Reconstr Aesthet Surg. 2014;67(9):1171–85.
Blanc J, Fuchsmann C, Nistiriuc-Muntean V, Jacquenot P, Philouze P, Ceruse P. Evaluation of virtual surgical planning systems and customized devices in fibula free flap mandibular reconstruction. Eur Arch Otorhinolaryngol. 2019;276(12):3477–86.
Brown JS, Rogers SN, McNally DN, Boyle M. A modified classification for the maxillectomy defect. Head Neck. 2000;22(1):17–26.
Breik O, Idle M, Martin T, Praveen P, Parmar S. Three-dimensional computer-assisted surgical planning and manufacturing in complex maxillary reconstruction. Atlas Oral Maxillofac Surg Clin North Am. 2020;28(2):151–64.
Padilla PL, Mericli AF, Largo RD, Garvey PB. Computer-aided design and manufacturing versus conventional surgical planning for head and neck reconstruction: a systematic review and meta-analysis. Plast Reconstr Surg. 2021;148(1):183–92.
Mazzola F, Smithers F, Cheng K, Mukherjee P, Low THH, Ch’ng S, et al. Time and cost-analysis of virtual surgical planning for head and neck reconstruction: a matched pair analysis. Oral Oncol. 2020; 100:104491.
Moe J, Foss J, Herster R, Powell C, Helman J, Ward BB, et al. An in-house computer-aided design and computer-aided manufacturing workflow for maxillofacial free flap reconstruction is associated with a low cost and high accuracy. J Oral Maxillofac Surg. 2021;79(1):227–36.
Barry CB, MacDhabheid C, Tobin K, Stassen LF, Lennon P, Toner M, et al. ‘Out of house’ virtual surgical planning for mandible reconstruction after cancer resection: is it oncologically safe? Int J Oral Maxillofac Surg. 2021;50(8):999–1002.
Knitschke M, Bäcker C, Schmermund D, Böttger S, Steckbein P, Howaldt HP, et al. Impact of planning method (conventional versus virtual) on time to therapy initiation and resection margins: a retrospective analysis of 104 immediate jaw reconstructions. Cancers (Basel). 2021;13(12):3013.
Ettinger KS, Alexander AE, Arce K. Computed tomographic angiography perforator localization for virtual surgical planning of osteocutaneous fibular free flaps in head and neck reconstruction. J Oral Maxillofac Surg. 2018;76(1):2220–30.
Yodrabum N, Rudeejaroonrung K, Chaikangwan I, Prompattanapakdee J, Noraset T. Precision of low-cost augmented reality in prefabricated cutting guide for fibular free flap surgery. J Craniofac Surg. 2021 Aug 6 [online ahead of print].
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this paper
Cite this paper
McGoldrick, D., Praveen, P., Parmar, S. (2023). Modern Day Reconstruction of the Facial Bones. In: Vermorken, J.B., Budach, V., Leemans, C.R., Machiels, JP., Nicolai, P., O'Sullivan, B. (eds) Critical Issues in Head and Neck Oncology. Springer, Cham. https://doi.org/10.1007/978-3-031-23175-9_17
Download citation
DOI: https://doi.org/10.1007/978-3-031-23175-9_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-23174-2
Online ISBN: 978-3-031-23175-9
eBook Packages: MedicineMedicine (R0)