Abstract
Pembrolizumab and nivolumab, two monoclonal antibodies (mAbs) targeting programmed cell death protein-1 (PD-1), improve the overall survival of patients with inoperable recurrent and/or metastatic (R/M) head and neck squamous cell carcinoma (HNSCC). For curable HNSCC, the role of immunotherapy is under investigation. In this chapter, we briefly review the current use of immunotherapy with surgery or radio(chemo)therapy in the treatment of HNSCC with curative intent.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
- Head and neck squamous cell carcinoma
- Locally advanced
- Curative intent
- Surgery
- Radio(chemo) therapy
- Immunotherapy
Introduction
Pembrolizumab and nivolumab, two monoclonal antibodies (mAbs) targeting programmed cell death protein-1 (PD-1), improve the overall survival of patients with inoperable recurrent and/or metastatic (R/M) head and neck squamous cell carcinoma (HNSCC) [1].
For curable HNSCC, the role of immunotherapy is under investigation. Standard curative treatments are still based on unimodal or multimodal treatments consisting of surgery and/or (chemo)radiation depending on the stage and location of disease and the expected functional outcome. These treatments result in a survival rate of 80% and 50% at five years for early and advanced stages [2], respectively. In this chapter, we briefly review the potential role of anti-PD-1/PD-ligand (L) 1 inhibitors in the curative treatment of HNSCC, either in combination with curative-intent (chemo)radiation or surgical treatment.
Anti-PD-1/PD-L1 mAbs in Combination with Curative-Intent Primary Surgery
Surgery remains a treatment of choice for head and neck cancers. However, in locally advanced (LA) disease, more than half the patients will recur even after curative surgery with pathological disease-free margins. There are currently many studies investigating the role of neo-adjuvant or adjuvant immunotherapy in the context of surgery to reduce the risk of disease recurrence.
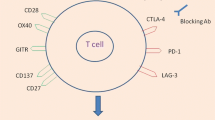
Mice bearing a mouse oral cancer and treated with pre-operative administration of anti-PD1 mAbs followed by surgery had a lower rate of new mouse oral cancer (MOC) cell engraftment after tumor re-challenge than controls or mice treated with surgery and adjuvant anti-PD-1 mAbs [3]. This means that pre-operative administration of anti-PD1 antibodies could promote the development of memory T cells. Furthermore, T cells recovered from tumor draining lymph nodes showed a significantly higher expression of interferon (INF)-gamma in response to the antigenic peptide in neoadjuvant treated mice compared to controls or adjuvant treated mice [3]. Similarly, Liu et al. [4] showed that triple-negative breast cancer mouse models treated with a neoadjuvant immune checkpoint inhibitor (ICI) (anti-PD1 and anti-CD137) plus surgery had better survival and higher levels of tumor-specific CD8+ cells in their blood and organs compared to mice treated with surgery and adjuvant immunotherapy. This provides a strong rationale for studying the efficacy of checkpoint inhibitors in head and neck cancers undergoing curative treatment, particularly before tumor surgery.
Anti-PD-1/PD(L)1 mAbs were investigated in several pre-operative window of opportunity studies. In a phase II study (NCT03021993), 12 patients with stage II-IVa oral squamous cell carcinoma (OSCC) were treated with three to four doses of nivolumab biweekly before curative surgery. The use of this checkpoint inhibitor during the 30 pre-operative days was found to be safe, and there was no delay in surgical management. The objective response rate was 33%, and 10 patients were still alive after a median follow-up of 2.23 years [5]. The phase I/II CheckMate 358 study investigated the safety and efficacy of two pre-operative doses of nivolumab in 26 patients with human papillomavirus (HPV)-positive HNSCC and in 26 patients with HPV-negative HNSCC. Nivolumab was administered on days 1 and 15 and curative surgery was performed on day 29. Four patients (19.2%) in the HPV-positive cohort and three patients (11.5%) in the HPV-negative cohort experienced severe treatment related adverse events (TRAEs). No delays in surgical treatment were observed. Nivolumab induced radiographic tumor shrinkage ≥30% according to RECIST criteria v1.1 in 12.0% and 8.3% of patients in the HPV-positive and HPV-negative cohorts, respectively. In addition, pathological regression was observed in 23.5% of patients with HPV-positive HNSCC and in 5.9% patients with HPV-negative tumors [6]. Another window of opportunity phase II study [7] investigated pembrolizumab as a single dose administered two to three weeks prior to surgery in 36 patients with HPV-negative HNSCC. Pathologic tumor-response (pTR) was defined as the proportion of the resection bed with tumor necrosis, giant cells/histiocytes and keratinous debris: pTR-0 (<10%), pTR-1 (10–49%), and pTR-2 (≥50%). The endpoints were safety, pTR-2 and the relapse rate at one year of patients with high-risk pathological features identified on their surgical specimens (extra nodal extension (ENE) and/or positive margins). Patients having high-risk pathology findings after surgery received adjuvant pembrolizumab. The administration of pembrolizumab in the pre-operative period was safe, and no surgical delays or immune-related adverse events were observed. Twelve patients received adjuvant pembrolizumab in combination with postoperative chemoradiation without any complications. With a median follow-up of 22 months after surgery, the one-year relapse rate was 16.7% and 0% for patients with pathological high-risk and low/intermediate-risk features after surgery, respectively. After neoadjuvant pembrolizumab, eight patients had pTR-2, including two patients who experienced a major pTR (>90%), and eight patients had pTR-1. Most patients maintained stable disease, but 19% had a decrease in pathological staging compared to clinical staging. PD-L1 expression and CD8+ T-cell infiltration in baseline biopsies were positively correlated with pTR. Deconvolution analysis using RNA-sequencing showed a significant increase in immune infiltrate (M1 macrophages, CD8+ T cells, and CD4+ T-cells) in baseline biopsies for pTR-1/2 patients compared to biopsies from pTR-0 patients. In baseline biopsies, a higher expression of inflammatory and immune genes (e.g., CXCL9, IFNG, CXCL10, …) was found in patients with pTR-1/2 compared to those with pTR-0. Accordingly, enrichment analyses showed an increased expression of signatures involved in inflammation (e.g., Hallmark interferon gamma response, Hallmark inflammatory response) in baseline biopsies of patients with pTR versus no pTR. Increased expression of checkpoint molecules (e.g., CTLA4, IDO1, PDCD1) was demonstrated in post-treatment tumor biopsies in pTR-0 patients. Whole exome sequencing of baseline biopsies showed no correlation between tumor mutational burden (TMB), predicted neoantigen burden, and pTR. Furthermore, patients with pTR-1/2 showed increased T-cell receptor (TCR) diversity and clonality in the blood after neoadjuvant pembrolizumab. A larger phase II study (NCT02641093) included 80 resectable p16-negative HNSCC patients with T3-T4 and/or two or more nodal metastases or clinical extra nodal extension (ENE). Patients were treated neoadjuvantly with pembrolizumab one to three weeks prior to surgery. After surgery, patients received pembrolizumab for a total of six doses with concurrent radiotherapy. Patients with high-risk HNSCC (positive margins and/or ENE) received concurrent cisplatin. Disease-free survival (DFS) after one year was the primary endpoint. One-year DFS was 97 and 66% in the intermediate and high-risk groups, respectively. Patients presenting a pathologic response had significantly improved DFS compared to patients without a pathologic response (93 vs. 72%) [8].
Currently, although anti-PD-1/PD-L1 therapy in combination with surgery with or without adjuvant (chemo)radiation gives promising signs of activity, the use of these drugs in combination with surgery for curative purposes is still not indicated in routine clinical practice.
Based on the results, several phase II/III studies are underway to better determine the role of anti-PD-1/PD(L)1 mAbs in curable HNSCC treated with primary surgery. These trials are described in Tables 11.1 and 11.2.
Anti-PD-1/PD-L1 mAbs in Combination with Primary Curative-Intent (Chemo)Radiation
Radiation therapy has the ability to enhance the immune response through several mechanisms. These include the release of neo-antigens during radiation-induced cell death [11], the activation of dendritic cells with enhanced expression of major histocompatibility (MHC) class I [12], and the release of cytokines [13], which all contribute to CD8+ T-cell activation. Radiation itself promotes the infiltration of immune cells into irradiated organs and increases PD-L1 expression [14]. However, radiation therapy can also induce cell damage to immune infiltrating cells. The complex interaction between immunotherapy, radiation therapy and optimal treatment sequencing still needs to be elucidated. The efficacy of radiotherapy combined with ICI depends on tumor models, dose, the irradiated site and type of irradiation, fractionation, and the timing/sequence of delivery. Similarly, Kanagavelu et al. [15] showed in different mouse models that the immune population in the tumor micro-environment is highly variable depending on the dose, irradiated site and tumor model. In addition, Marciscano et al. [16] found in some mouse models that irradiating the lymph nodes may be detrimental to the local control of the primary tumor and that immunocompetence was necessary to provoke a response to radiotherapy. Although conflicting, hypo-fractionated radiation is also of interest, and charged particles may be more immunogenic than photons [17]. However, there is no clinical evidence on which type of radiation therapy, combination and sequence is most appropriate for HNSCC patients, and there are conflicting results in several trials [18, 19].
Anti-PD1/PD(L)-1 mAbs in combination with (chemo)radiation have been investigated in several indications: (i) as a de-escalation strategy in good prognosis patients (e.g., stage I/II p16-positive oropharyngeal cancer), (ii) to replace chemotherapy in cisplatin-unfit patients, and (iii) as treatment intensification in combination with chemoradiation in poor prognosis patients (e.g., p16-negative LA HNSCC and stage 3 p16-positive oropharyngeal cancer) [20–22].
As anti-PD1/PD(L)-1 mAbs are generally well tolerated and have limited toxicities compared to standard chemotherapy, ICI are being investigated as a potential de-escalation strategy to avoid chemotherapy in good prognosis tumors [23]. HN005 (NCT03952585) is a three-arm randomized trial for non-smoking patients with T1-2 N1 or T3 N0-N1 p16-positive tumors that compares standard chemoradiation to reduced dose radiotherapy (60 Gy + nivolumab) versus reduced dose chemoradiation (60 Gy). Another trial (NCT03799445) combines nivolumab and ipilimumab with a reduced dose of radiotherapy for T1 N2, T2 N1-N2 or T3 N0-N2 HNSCC. The CCTG HN.9/EORTC1740, a randomized phase II trial, is currently investigating durvalumab plus radiation (concomitant and adjuvant) versus standard chemoradiation in p16-positive intermediate risk oropharyngeal cancer. All these trials involve highly selected populations with mainly low-risk oropharyngeal p16-positive cancers. A non-exhaustive list of the ongoing trials is described in Table 11.3.
ICI could also be used to replace chemotherapy in patients unfit for cisplatin. Patients unfit for cisplatin are generally defined as patients with either creatinin clearance <60 mL/min or neutrophils <1 500/μL or platelets <100 000/μL or serum albumin <35 g/L or peripheral neuropathy ≥ grade 2 or clinical hearing loss (confirmed by audiogram) or decreased left ventricular ejection fraction. In PembroRad (GORTEC 2015–01) [21], patients with locally advanced HNSCC unfit to receive high-dose cisplatin were randomized between radiotherapy (RT) + cetuximab and RT + pembrolizumab. Pembrolizumab was given only during RT. Loco-regional control (LRC), progression free survival (PFS) and overall survival (OS) were similar between the two groups. However, acute toxicity was lower in the pembrolizumab-RT arm than in the cetuximab-RT arm: 74% versus 92% patients with at least grade ≥3 acute adverse events (p = 0.006), mainly due to dermatitis in the radiation field, mucositis and cutaneous rash. In the REACH trial, patients unfit for cisplatin were randomized between avelumab + cetuximab + RT versus cetuximab + RT. In contrast to PembroRad, avelumab was not only administered concomitantly to RT but also for one year as adjuvant therapy. The primary endpoint was PFS. The avelumab-RT-based treatment did not significantly improve PFS compared to cetuximab-RT: the two-year PFS rates were 44% and 31%, respectively (p = 0.15) [24].
ICI therapy has also been investigated in combination with cisplatin-based chemoradiation in patients with LA HNSCC. As previously stated, LA HNSCC patients have a high recurrence rate [2], and 40–50% will relapse within two years despite multimodal treatment. JAVELIN 100 compared high dose cisplatin chemoradiation combined with avelumab or placebo. Avelumab was started one week before the initiation of chemoradiation, was continued every two weeks during chemoradiation, and then maintained as adjuvant treatment for one year. The trial did not meet its primary endpoint: median PFS was 16.9 months in the avelumab arm and not reached in the control arm (p = 0.92). Subgroup analysis showed that PD-L1 expressing tumors might benefit from the addition of avelumab, although this analysis was impaired by the low number of patients. In the REACH study, cisplatin fit patients were randomized between high-dose cisplatin chemoradiation and RT + avelumab + cetuximab. The trial was, however, closed prematurely for futility [24]. KEYNOTE 412 investigated concomitant and adjuvant pembrolizumab with cisplatin-based chemoradiation. After a median of almost 4 years of follow-up, median event-free survival was not reached with pembrolizumab plus chemoradiation and was 46.6 months with chemoradiation alone (hazard ratio [HR] = 0.83; P = .0429). This difference failed to meet the superiority threshold (efficacy boundary was P = .0242). The addition of pembrolizumab to chemoradiation appeared to result in greater event-free survival benefit compared with chemoradiation alone in PD-L1–positive patients, according to a post hoc analysis [25]. Other phase II and III studies are still ongoing in LA HNSCC and are described in Table 11.4. In particular, IMVoke010 is studying atezolizumab in the adjuvant setting only after concurrent chemoradiation and are described in Table 11.4.
Conclusion
Immunotherapy has the potential to improve the efficacy of treatment in patients with LA HNSCC. Although we await the outcome of several studies, the first reported trials have been discouraging.
Innovative approaches are needed to investigate the best way(s) to integrate ICI with multimodal curative treatment. For example, strategies such as better patient selection (PD-L1 expressing tumors), ICI after chemoradiation (similar to the PACIFIC trial in lung—IMVoke 100), or ICI in the neoadjuvant setting before surgery (KEYNOTE 689) are worthy of exploration. Another hypothesis to explain the non-benefit of anti-PD/PD(L)-1 mAbs in combination with (chemo)radiation is the large field of irradiation to regional lymph nodes that might neutralise immune competent cells. To circumvent that possibility, the REWRITE trial (NCT03726775) is investigating the activity of durvalumab in combination with less extensive nodal radiation therapy (irradiation of adjacent lymph nodes only). The primary endpoint of this trial is the rate of relapse in non-irradiated regional lymph nodes in a highly selected population (T1-T4 with clinical status N0-N1 or N2a-N2b non-palpable). Hopefully, the ongoing investigations and those of the future will guide how these agents can be best used in the curative setting.
Abbreviations
- CCTG:
-
Canadian Cancer Trials Group
- DFS:
-
Disease-Free Survival
- ENE:
-
Extra Nodal Extension
- EORTC:
-
European Organization for Research and Treatment of Cancer
- Gy:
-
Gray
- HNSCC:
-
Head and Neck Squamous Cell Carcinoma
- HPV:
-
Human Papillomavirus
- ICI:
-
Immune Checkpoint Inhibitor
- INF:
-
Interferon
- LA:
-
Locally Advanced
- mAbs:
-
Monoclonal Antibodies
- MHC:
-
Major Histocompatibility Complex
- MOC:
-
Mouse Oral Cancer
- PD(L)-1:
-
Programmed Cell Death Protein-(Ligand) 1
- pTR:
-
Pathologic Tumor Response
- R/M:
-
Recurrent and/or Metastatic
- RT:
-
Radiotherapy
- TRAEs:
-
Treatment Related Adverse Events
References
Ferris RL, Blumenschein G, Fayette J, Guigay J, Colevas AD, Licitra L, et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med. 2016;375(19):1856–67.
Machiels JP, Lambrecht M, Hanin FX, Duprez T, Gregoire V, Schmitz S, et al. Advances in the management of squamous cell carcinoma of the head and neck. F1000Prime Rep. 2014;6:44.
Friedman J, Moore EC, Zolkind P, Robbins Y, Clavijo PE, Sun L, et al. Neoadjuvant PD-1 immune checkpoint blockade reverses functional immunodominance among tumor antigen-specific T cells. Clin Cancer Res. 2020;26(3):679–89.
Liu J, Blake SJ, Yong MC, Harjunpää H, Ngiow SF, Takeda K, et al. Improved efficacy of neoadjuvant compared to adjuvant immunotherapy to eradicate metastatic disease. Cancer Discov. 2016;6(12):1382–99.
Knochelmann HM, Horton JD, Liu S, Armeson K, Kaczmar JM, Wyatt MM, et al. Neoadjuvant presurgical PD-1 inhibition in oral cavity squamous cell carcinoma. Cell Rep Med. 2021;2(10): 100426.
Ferris RL, Spanos WC, Leidner R, Gonçalves A, Martens UM, Kyi C, et al. Neoadjuvant nivolumab for patients with resectable HPV-positive and HPV-negative squamous cell carcinomas of the head and neck in the CheckMate 358 trial. J Immunother Cancer. 2021; 9(6).
Uppaluri R, Campbell KM, Egloff AM, Zolkind P, Skidmore ZL, Nussenbaum B, et al. Neoadjuvant and adjuvant pembrolizumab in resectable locally advanced, human papillomavirus-unrelated head and neck cancer: a multicenter, phase II trial. Clin Cancer Res. 2020;26(19):5140–52.
Wise-Draper TM, Gulati S, Palackdharry S, Hinrichs BH, Worden FP, Old MO, et al. Phase II clinical trial of neoadjuvant and adjuvant pembrolizumab in resectable local-regionally advanced head and neck squamous cell carcinoma. Clin Cancer Res. 2022;28(7):1345–52.
Uppaluri R, Lee NY, Westra W, Cohen EEW, Haddad RI, Temam S, et al. KEYNOTE-689: Phase 3 study of adjuvant and neoadjuvant pembrolizumab combined with standard of care (SOC) in patients with resectable, locally advanced head and neck squamous cell carcinoma. J Clin Oncol. 2019; 37(15_suppl): TPS6090–TPS.
Zech HB, Moeckelmann N, Boettcher A, Muenscher A, Binder M, Vettorazzi E, et al. Phase III study of nivolumab alone or combined with ipilimumab as immunotherapy versus standard of care in resectable head and neck squamous cell carcinoma. Future Oncol. 2020;16(36):3035–43.
Arina A, Gutiontov SI, Weichselbaum RR. Radiotherapy and immunotherapy for cancer: from “Systemic” to “Multisite.” Clin Cancer Res. 2020;26(12):2777–82.
Gupta A, Probst HC, Vuong V, Landshammer A, Muth S, Yagita H, et al. Radiotherapy promotes tumor-specific effector CD8+ T cells via dendritic cell activation. J Immunol. 2012;189(2):558–66.
Gerber SA, Sedlacek AL, Cron KR, Murphy SP, Frelinger JG, Lord EM. IFN-γ mediates the antitumor effects of radiation therapy in a murine colon tumor. Am J Pathol. 2013;182(6):2345–54.
Xing DT, Khor R, Gan H, Wada M, Ermongkonchai T, Ng SP. Recent research on combination of radiotherapy with targeted therapy or immunotherapy in head and neck squamous cell carcinoma: a review for radiation oncologists. Cancers (Basel). 2021; 13(22).
Kanagavelu S, Gupta S, Wu X, Philip S, Wattenberg MM, Hodge JW, et al. In vivo effects of lattice radiation therapy on local and distant lung cancer: potential role of immunomodulation. Radiat Res. 2014;182(2):149–62.
Marciscano AE, Ghasemzadeh A, Nirschl TR, Theodros D, Kochel CM, Francica BJ, et al. Elective nodal irradiation attenuates the combinatorial efficacy of stereotactic radiation therapy and immunotherapy. Clinical Cancer Res: An Official J Am Assoc Cancer Res. 2018;24(20):5058–71.
Oweida A, Lennon S, Calame D, Korpela S, Bhatia S, Sharma J, et al. Ionizing radiation sensitizes tumors to PD-L1 immune checkpoint blockade in orthotopic murine head and neck squamous cell carcinoma. Oncoimmunology. 2017;6(10): e1356153.
Lee Y, Auh SL, Wang Y, Burnette B, Wang Y, Meng Y, et al. Therapeutic effects of ablative radiation on local tumor require CD8+ T cells: changing strategies for cancer treatment. Blood. 2009;114(3):589–95.
Boustani J, Lecoester B, Baude J, Latour C, Adotevi O, Mirjolet C, et al. Anti-PD-1/Anti-PD-L1 drugs and radiation therapy: combinations and optimization strategies. Cancers (Basel). 2021; 13(19).
Rosenberg AJ, Agrawal N, Pearson A, Gooi Z, Blair E, Cursio J, et al. Risk and response adapted de-intensified treatment for HPV-associated oropharyngeal cancer: optima paradigm expanded experience. Oral Oncol. 2021;122: 105566.
Bourhis J, Sire C, Tao Y, Martin L, Alfonsi M, Prevost JB, et al. LBA38 Pembrolizumab versus cetuximab, concomitant with radiotherapy (RT) in locally advanced head and neck squamous cell carcinoma (LA-HNSCC): results of the GORTEC 2015–01 “PembroRad” randomized trial. Ann Oncol. 2020;31:S1168.
Lee NY, Ferris RL, Psyrri A, Haddad RI, Tahara M, Bourhis J, et al. Avelumab plus standard-of-care chemoradiotherapy versus chemoradiotherapy alone in patients with locally advanced squamous cell carcinoma of the head and neck: a randomised, double-blind, placebo-controlled, multicentre, phase 3 trial. Lancet Oncol. 2021;22(4):450–62.
Sedghizadeh PP, Billington WD, Paxton D, Ebeed R, Mahabady S, Clark GT, et al. Is p16-positive oropharyngeal squamous cell carcinoma associated with favorable prognosis? A systematic review and meta-analysis. Oral Oncol. 2016;54:15–27.
Bourhis J, Tao Y, Sun X, Sire C, Martin L, Liem X, et al. LBA35 Avelumab-cetuximab-radiotherapy versus standards of care in patients with locally advanced squamous cell carcinoma of head and neck (LA-SCCHN): Randomized phase III GORTEC-REACH trial. Ann Oncol. 2021;32:S1310.
Machiels JP, Tao Y, Burtness B, et al. Primary results of the phase 3 KEYNOTE-412 study: Pembrolizumab plus chemoradiation therapy (CRT) vs placebo plus CRT for locally advanced head and neck squamous cell carcinoma. 2022 ESMO Congress. Abstract LBA5. Presented September 11, 2022.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this paper
Cite this paper
Beyaert, S., Honoré, N., Machiels, JP. (2023). Immune Checkpoint Inhibitors in the Curative Setting: Pre-clinical and Clinical Data. In: Vermorken, J.B., Budach, V., Leemans, C.R., Machiels, JP., Nicolai, P., O'Sullivan, B. (eds) Critical Issues in Head and Neck Oncology. Springer, Cham. https://doi.org/10.1007/978-3-031-23175-9_11
Download citation
DOI: https://doi.org/10.1007/978-3-031-23175-9_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-23174-2
Online ISBN: 978-3-031-23175-9
eBook Packages: MedicineMedicine (R0)