Abstract
In a healthy pregnancy, the best response to sexual insecurity is reassurance and telling the couple that they can continue to be sexually active. When the situation gets complicated, things can be different. This chapter elaborates on the sexual risks in conditions such as premature birth, shortened cervix, placental dysfunction, and multiple gestation. It will delineate the relationship between various sexual activities and their potential influence on the uterus and the pregnancy. The chapter will also address how to communicate when specific sexual acts should be discouraged (or forbidden) and simultaneously give room for other sexual acts, in other words: the sexual do’s and don’ts. Midwives and HCPs must be aware of the cultural taboos between the woman and the couple regarding sexuality and pregnancy. It is a common finding in research that patients have many questions about sex but do not ask them. The consequence is that the professional must anticipate when providing information, as it were, by ‘answering the not-asked questions’. This chapter provides the background information needed to do just that in high-risk and complicated pregnancies.
This chapter is part of ‘Midwifery and Sexuality’, a Springer Nature open-access textbook for midwives and related healthcare professionals.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Not-asked questions
- Preterm birth
- Balancing approach
- Ferguson reflex
- Shortened cervix
- Prostaglandin
- Oxytocin
1 Introduction
Complications during pregnancy tend to create much insecurity, also regarding sexuality. Then, it is tempting for HCPs to advise against ‘having sex’ or even more veiled to recommend ‘pelvic rest’. They are presumably building on a traditional assumption that sex’s primary role is to make pregnant and no more needed after reaching that goal. At the same time, we know that sexuality has many functions other than conception. So, in complicated and high-risk pregnancies, HCPs have to balance carefully with their restrictions and recommendations between, on the one hand, damage to the pregnancy, mother or baby and, on the other hand, damage to the sexual health of the woman, her partner, and the relationship. This chapter will start by addressing aspects of this ‘balancing approach’.
After that, we will pay attention to the various aspects of sexual behaviour with their potential influence on the health of pregnancy, woman, or baby.
Thereafter, the most relevant disruptions during pregnancy will be reviewed, with some explanation, and with, per disruption, advice/recommendation on what should be discouraged or avoided and what is permissible or recommended. The information relies heavily on an extensive review by MacPhedran [1].
2 The Balancing Approach in Communication
Couples and the partners within a couple tend to be different, and so are their sexual needs and their ability to abstain from sexual behaviour when pregnancy gets complicated. Then, some couples can adapt to a reduction or complete absence of sexual contact without really being bothered by it. For many other couples, sexuality is a more relevant or necessary aspect of their life and relationship, and they will have worries and questions about what is allowed and what is or could be dangerous. Most pregnant women will not tell these worries to their HCP, even not to the very trusted midwife. So, in case of complicated pregnancies, the HCP has to ‘decide’ which strategy to follow. Here are, in short, the essentials of the three strategies.
-
1.
Pay no attention at all. That is not optimal care because it can damage women’s and couples’ health and sexual health. Besides, it is not suitable for good contact between the HCP and the woman or couple.
-
2.
Pay only attention to what is not allowed and the potential dangers of sex: ‘Thou should not have sex!’. Some HCPs do that more implicit or veiled, for instance, by using the term ‘Keep pelvic rest’. That approach is not quality care either.
Both these strategies can and will have negative consequences. Without explicitly mentioning the discouraged or forbidden elements of sexual behaviour and without mentioning the sexual behaviour that is allowed, the HCP will create insecurity and perpetuate the taboo on openly addressing sexuality. HCPs must be aware of the power of taboo. Besides, the HCP misses an opportunity to establish a trustworthy relationship with the woman and the couple.
-
3.
Pay in detail attention to the discouraged elements of sexuality, and combine that with a proper explanation of the reason for that advice. Moreover, mention explicitly aspects of allowed sexual behaviour.
One could argue that it is the role of the HCP to answer the ‘not-asked questions’ proactively.
There are smooth transitions between what absolutely should not happen and what better might not occur. There are also smooth transitions between indicating that there is no danger associated with specific sexual acts and, on the other hand, explicitly advising to get started with that way of sex. Sometimes the last seems needed. An example is when penetration can be dangerous, but the male partner is not used to sex without penetration. Then, one can consider mentioning non-penetrative sexuality or masturbation.
On the content aspect: By explicitly mentioning several possibilities, the HCP generates wider sexual choices while at the same time reducing the taboo between the partners.
An example: ‘You could cuddle till you feel you need to come. You could continue and bring yourself to orgasm. Many of us learned that masturbation should be done without being seen. However, many also learned that there are other possibilities. When your wife feels in the mood, she can help you. Or you can do it yourself with her in your arms. Quite some couples feel that as very intimate!’
On the communication aspect: straightforward advice (e.g. ‘Try a vibrator’ or ‘Try masturbation on your own or together!’) can make the HCP virtually enter the woman’s or couple’s bedroom. It is better to use a detour (e.g. ‘In comparable situations, some couples tried masturbation, and that apparently worked well’).
3 The Damaging Potential of Sexuality in Case of Increased Risk
This part pays attention to how various aspects of sexual behaviour could negatively influence the health of the pregnancy, woman, or baby in situations of high-risk and complicated pregnancies. On the one hand, that needs a breakdown of sexuality into separate elements and, on the other hand, a clear explanation of how each part could damage. See Table 12.1.
Potential risk factors are:
-
increased genital/pelvic circulation (as part of sexual arousal),
-
increased blood pressure (as part of sexual arousal and orgasm),
-
increased oxytocin levels,
-
increased prostaglandin levels,
-
increased uterine contractions,
-
direct mechanical influence.
Although maybe not necessary to mention, let it be clear that none of these phenomena can do any harm in the absence of pathology or pregnancy pathology.
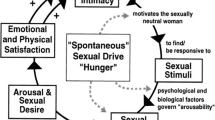
Arousal: When in the non-pregnant situation, the woman perceives sexual stimuli, there is a rapid (within 10–30 s) increase in vaginal circulation. During pregnancy, the genital/pelvic hypercongestion makes it challenging to estimate the additional circulation effects of sexual arousal. It is simply not known if a minor amount of sexual arousal could do any harm. That is different in the high arousal state. Then, the pelvic circulation becomes maximally engorged, and there is a rise in heart rate and systolic blood pressure.
Orgasm: In the third trimester, the clonic orgasm pattern (contract → relax → contract → etc.) can change into a pattern of one tonic spasm, which can last up to a minute, sometimes accompanied by deceleration of the foetal heart rate and recurrent contractions till half an hour after orgasm. There is much inter-individual variety in this orgasm pattern.
Whereas blood pressure and heart rate already can increase during arousal, peak values are found at the start of orgasm.
Oxytocin: causes uterine contractions. It increases at hugging and massage and more at stimulation of breast and nipples. Sexual arousal and orgasm both increase oxytocin levels, which is most clearly seen at orgasm and still is high 5 min. after orgasm. The direct pressure on the cervix and vaginal tissues by the penetrating penis will cause a surge in oxytocin (the ‘Ferguson reflex’). This effect is also seen after anal penetration.
There are no research data on the relationship between kissing and oxytocin.
Prostaglandin: PGE and PGF stimulate myometrial activity, can ripen the cervix, and induce labour. Endogenous PG is released when the penis, dildo, or finger touch the cervix. Exogenous PG is deposited with the semen in a higher dose than common cervical ripening agents. It can be found in the vagina up to 12 h after ejaculation. Exogenous PG can cause myometrial activity after being absorbed through the vaginal wall into the woman’s circulation, but it can also act directly on cervical ripening.
PGF acts much stronger than PGE. However, semen contains ±20x more PGE than PGF and also ±20x more 19-hydroxy-PGE than 19-hydroxy-PGF [2].
Whereas the PGs deposited at anal ejaculation will not ripen the cervix, they are easily absorbed through the anal mucosa into the woman’s circulation.
4 The Various Obstetric Disruptions
The rest of this chapter will successively pay attention to the sexual implications of the most common pregnancy disruptions. As far as possible, we will give for each disruption relevant information/explanation and also advice/recommendations on what should be discouraged or avoided and what is permissible or recommended. For part of these recommendations, there is not yet much scientific evidence. More detailed information can be found in the review by Sally MacPhedran [1].
4.1 Recurrent Miscarriage: (Habitual or Spontaneous Abortion/Pregnancy Loss)
This is usually defined as three failed clinical pregnancies, confirmed by either sonographic or histopathological examination.
One percent of fertile couples have recurrent miscarriages. Most of these are early losses before 14 weeks of pregnancy. The great majority results from parental chromosomal abnormalities (with many being anembryonic pregnancies that form half of all first-trimester miscarriages) and a small subset of uterine anomalies. Many women with recurrent miscarriages are scared and assume that coitus will harm the foetus or that direct contact between the penis and cervix could trigger a miscarriage. No research data support this possibility. Regarding orgasm: In the first trimester, the oxytocin increase by orgasm will do not harm since the uterus does not yet have enough oxytocin receptors. Regarding the damage of intravaginal ejaculation: the prostaglandin levels of semen are much lower than the high dose of prostaglandins needed for the induction of medical abortion in early pregnancy.
4.1.1 Restrictions or Recommendations?
‘Can sex cause a miscarriage?’ is possibly the most frequently asked (or unasked) question in early pregnancy. Despite even the slightest evidence, HCPs have urged caution (in a review called: ‘A concise history of not knowing’) [3].
Since the literature does not indicate any adverse effects of the various elements of sexual play in recurrent miscarriage, we can be mild in our recommendations. Maybe most important is a sex-positive approach with, in the discussion, a breakdown of various elements of intimate contact that will be beneficial to the couple and the value of sexual pleasure. Since many women and couples who suffer recurrent miscarriages have esteem issues, the affirmation obtained through sex could be beneficial.
In all literature, we found very few articles that pay any attention to other non-organic aspects of recurrent miscarriage except ‘Tender loving care’, which is defined as psychological support with weekly medical and ultrasonographic examinations and instructions to avoid heavy work and travel [4]. The authors also indicated avoiding sexual activity. We disagree with the last remark.
4.2 Bleeding in First Trimester
Bleeding in the first trimester of pregnancy can signify impending miscarriage, and molar or ectopic pregnancy. Bleeding is the most predictive risk factor for pregnancy loss. Among the other causes of bleeding are vanishing-twin or bleeding unrelated to the pregnancy (including cervical polyp, vaginal infection, rupture of cervical blood vessels, tumour, and trauma). The potential inflammatory consequences of penetration and ejaculation may serve as a secondary insult in an already compromised environment [1].
What Is Allowed: When intrauterine pregnancy is confirmed and no other pathology is found, we believe there is no objection to the full range of penetrative sexuality, excluding the below-mentioned activities.
What Should Not Be Done: We recommend not to have vaginal penetration, vaginal ejaculation, and orovaginal contact at the time of bleeding (because of an already compromised environment).
-
Be aware: these precautions of ‘no vaginal penetration during bleeding’ do not apply during menstruation. Although penetrative sex at that time can be messy or be unacceptable for emotional, cultural, or religious reasons, it does no harm.
4.3 Hyperemesis
Whereas 60–75% of pregnant women report usual nausea and vomiting, 0.5–2% report hyperemesis. Among the various causes are high or rapidly rising HCG levels and stress.
What Should Not Be Done: Everything that bothers the woman during nausea.
What Is Allowed/Recommended: Everything that distracts and relaxes her and does not increase nausea. Usually, massage is a good start. The sequel will be determined by the fears and emotional needs of the woman and her partner. And, of course, by how the couple has learned to continue or not to continue after foreplay. Especially when hyperemesis lasts long, it becomes relevant to pay attention to the sexual needs and worries of the partner.
4.4 Shortened Cervix
A short cervical length (below 25 mm. measured by transvaginal ultrasound between 16–24 weeks gestational age) developing in this pregnancy is a risk factor for preterm birth. The shorter the length, the greater the risk. Additional risk factors are prior preterm birth, blood loss (even spotting), and uterine contractions.
When there is a short cervix because of earlier conization or large loop excision of the transformation zone (LLETZ) for pre-cancerous cell changes, there seems no reason to abstain from any sexual activity.
What Should Not Be Done: Especially when a short cervix is combined with one or more of the other risk factors, the couple is advised to abstain from all penetrative sex, female orgasm, and other sexual activities that cause or can cause uterine contractions.
It could be wise to recommend that the woman or couple pay attention to the eventual sexual needs of the partner and find ways to deal with that without increasing risk for uterine activity.
4.5 Cerclage
The various cerclage types are intended to prevent the cervix from opening too early.
Transabdominal cerclage is done before the pregnancy because of severe cervical anatomy defects. Prophylactic cerclage is done early in pregnancy because of cervical incompetence in former pregnancies. Rescue cerclage is done because the cervix is already flattening or opening in the current pregnancy.
Recommendations: In all cerclage procedures, one should abstain from penetrative sex the week before and the 2 weeks after the procedure.
After prophylactic cerclage, condoms are recommended in penetrative sex because of the risk of infection and chorioamnionitis, leading to preterm birth. The potential inflammatory effect of semen and the penile flora may serve as a secondary insult in an already compromised environment [1]. There are no objections to all other sexual activities.
After rescue cerclage, it is wise to abstain from vaginal penetration, anal penetration, masturbation, and orgasm until approximately 37 weeks. That situation requires extra attention and regular checking if the woman and her partner can handle this situation.
4.6 High Blood Pressure and Preeclampsia
Hypertensive disorders complicate 5–10% of all pregnancies and contribute significantly to maternal morbidity and mortality. Part of the pregnant women already had (chronic) hypertension. Hypertension developed after week 20 of the pregnancy (termed gestational hypertension) is followed by signs and symptoms of preeclampsia in half of the cases, with preeclampsia in 3.9% of all pregnancies [5].
Which aspects of sexuality are risk factors in the woman with preeclampsia? Physical activity (as in aerobic exercise); autonomous nerve activity; uterine contractions; and increase in blood pressure.
When comparing the woman with a slight increase in blood pressure and the woman with high blood pressure and signs of preeclampsia, it will be apparent that sexual expression will not have the same consequences. That means the HCP should consider which sexual behaviour is still acceptable and which sexual behaviour poses a danger. Next is explaining such information in detail to the couple. And then check in how far the couple can deal with those recommendations.
In gestational hypertension, aerobic exercise is contraindicated, and accordingly, there should be no strenuous sexual activity (for instance, intercourse with the woman on top). When there are signs of preeclampsia, we believe that the woman should refrain from high arousal and orgasm.
There is no objection to gentle kissing, hugging, and cuddling. When penetration appears very needed, some couples could consider gentle penetration, tell how much they love each other, and eventually finish the encounter by the partner’s masturbation and ejaculation outside the vagina.
4.7 Poor Placental Function
Foetal growth restriction can be a sign of poor placental function. When that is related to the hypertension/preeclampsia complex, the woman better refrains from most aspects of sexual behaviour (see above).
Without preeclampsia, we do not know if sexual behaviour yields any risk for the mother or child. Sexual arousal is accompanied by increased uterine circulation. In pregnancy, however, we do not know if it benefices the circulation of the placenta and the foetus.
4.8 Urinary Tract Infection (UTI)
Women regularly have asymptomatic bacteriuria. So this is frequently found in prenatal care. When pregnant, the smooth muscles of the ureters relax. The subsequent dilatation and the increased abdominal pressure due to the growing uterus appear to facilitate the ascent of bacteria from the bladder to the kidney. That creates a dilemma. On the one hand, untreated bacteriuria is associated with more pyelonephritis and an increased risk of preterm birth, low birthweight, and perinatal mortality. On the other hand, treatment with antibiotics creates antibiotic resistance. That is a real disadvantage during pregnancy since several teratogenic antibiotics may not be used. Research focuses strongly on hygienic measures to prevent urinary tract infections. More urinary tract infection was found with sexual activity >2–3x per week and when the bladder was not voided after intercourse [6].
Non-sexual recommendations are as follows: wipe/wash the genital area from front to back after going to the toilet; do not delay when having to pass urine; and drink enough.
Sexual recommendations: void the bladder after intercourse; wash the genital area after intercourse [6]. In addition, we recommend not to have intercourse too frequently (when the need is high, consider having non-penetrative sex). After having anal sex, pay extra attention to perineal washing/cleaning; do not combine any anal activity with vaginal penetration.
4.9 Colpitis/Vaginal Infection
The microbiome in the healthy female genital tract is dominated by bacteria that produce lactic acid, maintaining a low pH and protecting against infections. Pregnancy influences that microbiome, resulting in more genital tract infections [7] with, in its wake, an increased risk of preterm birth and pelvic infections.
Pregnancy changes the woman’s microbiome. It can also influence her male partner’s sexual behaviour, sometimes resulting in extramarital contact and an increased risk of STI or trichomonas [8].
To varying degrees, vaginal infections are relevant because of the complaints (discharge, itching, dyspareunia, burning sensation in the vulva, and burning at passing urine) influencing sexuality and the increased risk for preterm birth and neonatal consequences.
Bacterial vaginosis (BV) is a misdistribution of the normal vaginal flora, resulting from high colonization of anaerobic organisms (Gardnerella vaginalis and others) and increased vaginal pH. BV prevalence among women of reproductive age varies from 5 to 60%, depending on the geographic area and diagnostic criteria. About half of the women with BV are symptomatic, with a fish-smelling discharge as the most common complaint. Although sexual intercourse appears to be a risk factor, there is no evidence that BV is an STI. Women using petroleum jelly as a lubricant have more BV [9]. BV early in pregnancy is a vital risk factor for preterm birth and spontaneous abortion [10]. Treatment of bacterial vaginosis during pregnancy improves symptoms but does not reduce the risk of preterm birth [11].
Candida albicans commonly colonizes the vagina of pregnant women. That can be asymptomatic or cause symptoms like pruritis of vaginal discharge. Reinfection is common without simultaneous treatment of the sexual partner(s). Vulvovaginal candidiasis is found more in women who receive oral sex and when using vaginal lubricants containing glycerine/glycerol because candida thrives on that.
Trichomoniasis is characterized by a foul-smelling discharge. Treatment must include the sexual partner(s).
Aerobic vaginitis shows an increase in mucosal inflammation with subsequently more dyspareunia [12].
GBS or streptococcus agalactiae is one of the potential microorganisms of aerobic vaginitis. Colonization with Group B streptococcal infections (GBS) is often asymptomatic and may cause UTI and PPROM (preterm premature rupture of membranes). Heavy maternal colonization with GBS at birth can be associated with fulminant neonatal infection.
Sexuality: In many couples, the complaints (discharge/smell) will prevent sex and especially the cunnilingus part. Since these troubles frequently are accompanied by dyspareunia, it seems wise to inform the couple that this could be the entrance to a long-lasting vicious circle of ‘pain → no desire → pain’ and recommend looking for non-penetrative ways of sexual interaction.
Since there are associations between the male-superior position, PPROM, and infections [13], it seems wise to recommend replacing the male-superior with other positions.
4.10 Uterine Contractions
Especially for the primigravid woman, uterine contractions may be frightening. The majority are Braxton–Hicks contractions that do not relate to the start of childbirth. They are uncomfortable but tend not to be painful (in contrast to labour pain). They can appear more frequently with sexual activity.
During an orgasm, the woman also has contractions. In the last weeks of pregnancy, some women experience a change in orgasm. The typical clonic pattern of ‘contract → relax → contract’ turns into a pattern of one strong tonic contraction. That appears to be enhanced by the oxytocin increase and intravaginal deposition of seminal prostaglandin. In a healthy pregnancy that neither does any harm nor causes preterm labour.
Recommendations: As long as the pregnancy is healthy and without signs of preterm birth, there are no contraindications to the whole gamut of sexual play.
However, when painful contractions seem to transition into signs of preterm birth (bleeding, shorter cervix, persisting contractions), the couple should refrain from such sexual activities.
4.11 Premature Rupture of Membranes
Preterm premature rupture of membrane (PPROM) refers to chorioamniotic membrane rupture before 37 weeks of gestation. Women with PPROM are at an increased risk of preterm birth because of infection or chorioamnionitis, progression of preterm labour, or placental abruption because of a change in uterine pressure with loss of amniotic fluid. Vaginal penetration, anal penetration, and orovaginal contact increase the risk for ascending infection and chorioamnionitis. Since, in PPROM, the uterus is prone to start labour, the couple/woman should refrain from all sexual/erotic activities that can cause uterine contractions.
What Should Not Be Done: vaginal penetration, anal penetration, orovaginal contact, nipple stimulation, female masturbation, and female orgasm.
What Is Allowed: Kissing, hugging, gentle massage, partner orgasm.
4.12 History of Preterm Birth (PTB)
A history of PTB poses an increased risk for recurrent spontaneous PTB. So, many couples will be concerned about the potential dangers of sexual contact. There are, however, no reliable research data to help us in this discussion [1].
In the absence of a short cervix or other obstetric risks, there appear no reasons to abstain from any sexual activity.
When this pregnancy has/had an episode with symptoms indicating preterm labour, it is better to avoid any sexual activity that causes an increase in frequency or intensity of uterine contractions.
After a detailed search, MacPhedran says: “Individualise recommendations based on consideration of obstetric history and comorbidities as well as patient and partner fears and emotional needs” [1].
4.13 Bleeding in the Second Half of Pregnancy
There are many reasons for blood loss, including impending preterm birth, placenta previa, vasa previa, abruptio placentae, and uterine rupture. There are also some non-pregnancy-related causes (cervical polyp or tumour, vaginal infection, or trauma). The couple should abstain from sexual activities until a proper diagnosis is made (and treatment started). After that, the HCP should give detailed recommendations. First, we will address placenta previa and then solutio placentae (placental abruption).
Placenta Previa: is an important cause of bleeding in the third trimester. When the placenta is implanted low, the development of the lower uterine segment and the accompanying mechanical separation between the placenta and lower segment can cause (painless) bleeding. Such first (‘sentinel’) bleeding warrants abstaining from aerobic exercise and all sexual acts that cause uterine contractions or that mechanically influence the lower segment, so no woman-on-top position, no nipple stimulation, no vaginal or anal penetration, and no orgasm.
The same seems recommendable in the case of vasa previa.
Solutio Placentae-Placental Abruption: is the situation where already, before birth, the placenta separates from its implantation site. Total separation is a life-threatening emergency. In partial (‘chronic’) placental abruption, there is very little scientific information available on how to advise [1]. In a stable chronic placental abruption, it seems wise to recommend abstaining from all sexual activities that result in frequent, intense, or painful uterine contractions and from sexual activities that result in bleeding.
4.14 Multiple Gestation
A twin pregnancy differs little from a singleton pregnancy, except for the duration, with childbirth on average taking place at 37 weeks. According to the limited research in this area, sexuality does not influence the onset of birth [14]. So, without complications, the instructions and recommendations on sexuality can be the same.
In affluent societies, some 20% of twin pregnancies result from in vitro fertilization. Those parents tend to have less sex because the pregnancy is so precious (and maybe also by the knowledge that these pregnancies have more obstetrical complications).
Multiple pregnancies (triplets or more) have more prematurity. There are no data on the influence of sexuality on such pregnancies.
Recommendations in twin pregnancy: there are no restrictions.
Recommendations in triplets or more: we guess it wise to inform about the potential consequences of labour-inducing sexual activities and look with the couple for a good balance between safety for pregnancy and baby and, on the other hand, sexual/emotional satisfaction.
4.15 Presence of Uterine Scars
In the great majority (>99%) of caesarean sections (CS), there is a transverse incision in the lower part of the uterus. Without other obstetric complications, such a scar does not risk uterine rupture. That is different from the ‘classical CS’ with a longitudinal midline incision, usually to allow more space to deliver the baby. That scar has a 2% risk of uterine rupture pre-labour and 6% during labour [1]. Comparable risks exist after extensive uterine surgery, for instance for uterus duplex or intramural myomata. In all these women, a contraction stress test is contraindicated, and elective CS is indicated.
Recommendations: we should explicitly and repeatedly explain that any sexual stimulation causing prolonged or painful uterine contractions must be abandoned, indicating the risk of uterine rupture. These are the situations where the partner’s sexual needs deserve extra attention.
5 Conclusion
When dealing with threatening pregnancy complications, the essential message of this chapter is to proactively address the not-asked questions in the area of sexuality and intimacy. It then seems sensible to clarify which elements of sexual behaviour in their situation are dangerous for the mother-pregnancy-child unit. However, it is also relevant to proactively address what is ‘allowed’ or ‘recommended’. Balancing is needed between the consequences for the pregnancy and the child, and the consequences for the woman, her partner, and their sexual relationship.
Change history
10 April 2024
A correction has been published.
References
MacPhedran SE. Sexual activity recommendations in high-risk pregnancies: what is the evidence? Sex Med Rev. 2018;6:343–57.
Bendvold E, Gottlieb C, Svanborg K, et al. Concentration of prostaglandins in seminal fluid of fertile men. Int J Androl. 1987;10:463–9.
Moscrop A. Can sex during pregnancy cause a miscarriage; a concise history of not knowing. Br J Gen Pract. 2012;62:e308–10.
American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98:1103–11.
Cunningham FG, et al., editors. Williams obstetrics. 25th ed. New York: McGraw Hill Medical; 2018.
Ghouri F, Hollywood A, Ryan K. A systematic review of non-antibiotic measures for the prevention of urinary tract infections in pregnancy. BMC Pregnancy Childbirth. 2018;18:99.
Han C, Li H, Han L, et al. Aerobic vaginitis in late pregnancy and outcomes of pregnancy. Eur J Clin Microbiol Infect Dis. 2019;38:233–9.
Whisman MA, Gordon KC, Chatav Y. Predicting sexual infidelity in a population-based sample of married individuals. J Fam Psychol. 2007;21:320–4.
Brown JM, Hess KL, Brown S, et al. Intravaginal practices and risk of bacterial vaginosis and candidiasis infection among a cohort of women in the United States. Obstet Gynecol. 2013;121:773–80.
Leitich H, Bodner-Adler B, Brunbauer M, et al. Bacterial vaginosis as a risk factor for preterm delivery: a meta-analysis. Am J Obstet Gynecol. 2003;189:139–47.
Paladine HL, Desai UA. Vaginitis: diagnosis and treatment. Am Fam Physician. 2018;97:321–9.
Donders G, Bellen G, Grinceviciene S, et al. Aerobic vaginitis: no longer a stranger. Res Microbiol. 2017;168:845–58.
Ekwo EE, Gosselink CA, Woolson R, et al. Coitus late in pregnancy: risk of preterm rupture of amniotic sac membranes. Am J Obstet Gynecol. 1993;168:22–31.
Stammler-Safar M, Ott J, Weber S, Krampl E. Sexual behaviour of women with twin pregnancies. Twin Res Hum Genet. 2010;13:383–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Simetinger, G., Gianotten, W.L. (2023). Sexual Aspects of High-Risk and Complicated Pregnancy. In: Geuens, S., Polona Mivšek, A., Gianotten, W. (eds) Midwifery and Sexuality. Springer, Cham. https://doi.org/10.1007/978-3-031-18432-1_12
Download citation
DOI: https://doi.org/10.1007/978-3-031-18432-1_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-18431-4
Online ISBN: 978-3-031-18432-1
eBook Packages: MedicineMedicine (R0)